Medical Breakthroughs Set to be Fast-Tracked by Innovative New Health Agency

Pippy Rogers, second from left, with her four siblings, who worry that they are at risk for Alzheimer's and are calling for an acceleration of research.
In 2007, Matthew Might's son, Bertrand, was born with a life-threatening disease that was so rare, doctors couldn't diagnose it. Might, a computer scientist and biologist, eventually realized, "Oh my gosh, he's the only patient in the world with this disease right now." To find effective treatments, new methodologies would need to be developed. But there was no process or playbook for doing that.
Might took it upon himself, along with a team of specialists, to try to find a cure. "What Bertrand really taught me was the visceral sense of urgency when there's suffering, and how to act on that," he said.
He calls it "the agency of urgency"—and patients with more common diseases, such as cancer and Alzheimer's, often feel that same need to take matters into their own hands, as they find their hopes for new treatments running up against bureaucratic systems designed to advance in small, steady steps, not leaps and bounds. "We all hope for a cure," said Florence "Pippy" Rogers, a 65-year-old volunteer with Georgia's chapter of the Alzheimer's Association. She lost her mother to the disease and, these days, worries about herself and her four siblings. "We need to keep accelerating research."
We have a fresh example of what can be achieved by fast-tracking discoveries in healthcare: Covid-19 vaccines.
President Biden has pushed for cancer moonshots since the disease took the life of his son, Beau, in 2015. His administration has now requested $6.5 billion to start a new agency in 2022, called the Advanced Research Projects Agency for Health, or ARPA-H, within the National Institutes of Health. It's based on DARPA, the Department of Defense agency known for hatching world-changing technologies such as drones, GPS and ARPANET, which became the internet.
We have a fresh example of what can be achieved by fast-tracking discoveries in healthcare: Covid-19 vaccines. "Operation Warp Speed was using ARPA-like principles," said Might. "It showed that in a moment of crisis, institutions like NIH can think in an ARPA-like way. So now the question is, why don't we do that all the time?"
But applying the DARPA model to health involves several challenging decisions. I asked experts what could be the hardest question facing advocates of ARPA-H: which health problems it should seek to address. "All the wonderful choices lead to the problem of which ones to choose and prioritize," said Sudip Parikh, CEO of the American Association for the Advancement of Science and executive publisher of the Science family of journals. "There is no objectively right answer."
The Agency of Urgency
ARPA-H will borrow at least three critical ingredients from DARPA: goal-oriented project managers, many from industry; aggressive public-private partnerships; and collaboration among fields that don't always interact. The DARPA concept has been applied to other purposes, including energy and homeland security, with promising results. "We're learning that 'ARPA-ism' is a franchisable model," said Might, a former principal investigator on DARPA projects.
The federal government already pours billions of dollars into advancing research on life-threatening diseases, with much of it channeled through the National Institutes of Health. But the purpose of ARPA-H "isn't just the usual suspects that NIH would fund," said David Walt, a Harvard biochemist, an innovator in gene sequencing and former chair of DARPA's Defense Science Research Council. Whereas some NIH-funded studies aim to gradually improve our understanding of diseases, ARPA-H projects will give full focus to real-world applications; they'll use essential findings from NIH research as starting points, drawing from them to rapidly engineer new technologies that could save lives.
And, ultimately, billions in healthcare costs, if ARPA-H lives up to its predecessor's track record; DARPA's breakthroughs have been economic game-changers, while its fail-fast approach—quickly pulling the plug on projects that aren't panning out—helps to avoid sunken costs. ARPA-H could fuel activities similar to the human genome project, which used existing research to map the base pairs that make up DNA, opening new doors for the biotech industry, sparking economic growth and creating hundreds of thousands of new jobs.
Despite a nearly $4 trillion health economy, "we aren't innovating when it comes to technological capabilities for health," said Liz Feld, president of the Suzanne Wright Foundation for pancreatic cancer.
Individual Diseases Ripe for Innovation
Although the need for innovation is clear, which diseases ARPA-H should tackle is less apparent. One important consideration when choosing health priorities could be "how many people suffer from a disease," said Nancy Kass, a professor of bioethics and public health at Johns Hopkins.
That perspective could justify cancer as a top objective. Cancer and heart disease have long been the two major killers in the U.S. Leonidas Platanias, professor of oncology at Northwestern and director of its cancer center, noted that we've already made significant progress on heart disease. "Anti-cholesterol drugs really have a wide impact," he said. "I don't want to compare one disease to another, but I think cancer may be the most challenging. We need even bigger breakthroughs." He wondered whether ARPA-H should be linked to the part of NIH dedicated to cancer, the National Cancer Institute, "to take maximum advantage of what happens" there.
Previous cancer moonshots have laid a foundation for success. And this sort of disease-by-disease approach makes sense in a way. "We know that concentrating on some diseases has led to treatments," said Parikh. "Think of spinal muscular atrophy or cystic fibrosis. Now, imagine if immune therapies were discovered ten years earlier."
But many advocates think ARPA-H should choose projects that don't revolve around any one disease. "It absolutely has to be disease agnostic," said Feld, president of the pancreatic cancer foundation. "We cannot reach ARPA-H's potential if it's subject to the advocacy of individual patient groups who think their disease is worse than the guy's disease next to them. That's not the way the DARPA model works." Platanias agreed that ARPA-H should "pick the highest concepts and developments that have the best chance" of success.
Finding Connections Between Diseases
Kass, the Hopkins bioethicist, believes that ARPA-H should walk a balance, with some projects focusing on specific diseases and others aspiring to solutions with broader applications, spanning multiple diseases. Being impartial, some have noted, might involve looking at the total "life years" saved by a health innovation; the more diseases addressed by a given breakthrough, the more years of healthy living it may confer. The social and economic value should increase as well.
For multiple payoffs, ARPA-H could concentrate on rare diseases, which can yield important insights for many other diseases, said Might. Every case of cancer and Alzheimer's is, in a way, its own rare disease. Cancer is a genetic disease, like his son Bertrand's rare disorder, and mutations vary widely across cancer patients. "It's safe to say that no two people have ever actually had the same cancer," said Might. In theory, solutions for rare diseases could help us understand how to individualize treatments for more common diseases.
Many experts I talked with support another priority for ARPA-H with implications for multiple diseases: therapies that slow down the aging process. "Aging is the greatest risk factor for every major disease that NIH is studying," said Matt Kaeberlein, a bio-gerontologist at the University of Washington. Yet, "half of one percent of the NIH budget goes to researching the biology of aging. An ARPA-H sized budget would push the field forward at a pace that's hard to imagine."
Might agreed. "It could take ARPA-H to get past the weird stigmas around aging-related research. It could have a tremendous impact on the field."
For example, ARPA-H could try to use mRNA technology to express proteins that affect biological aging, said Kaeberlein. It's an engineering project well-suited to the DARPA model. So is harnessing machine learning to identify biomarkers that assess how fast people are aging. Biological aging clocks, if validated, could quickly reveal whether proposed therapies for aging are working or not. "I think there's huge value in that," said Kaeberlein.
By delivering breakthroughs in computation, ARPA-H could improve diagnostics for many different diseases. That could include improving biowearables for continuously monitoring blood pressure—a hypothetical mentioned in the White House's concept paper on ARPA-H—and advanced imaging technologies. "The high cost of medical imaging is a leading reason why our healthcare costs are the highest in the world," said Feld. "There's no detection test for ALS. No brain detection for Alzheimer's. Innovations in detection technology would save on cost and human suffering."
Some biotech companies may be skeptical about the financial rewards of accelerating such technologies. But ARPA-H could fund public-private partnerships to "de-risk" biotech's involvement—an incentive that harkens back to the advance purchase contracts that companies got during Covid. (Some groups have suggested that ARPA-H could provide advance purchase agreements.)
Parikh is less bullish on creating diagnostics through ARPA-H. Like DARPA, Biden's health agency will enjoy some independence from federal oversight; it may even be located hundreds of miles from DC. That freedom affords some breathing room for innovation, but it could also make it tougher to ensure that algorithms fully consider diverse populations. "That part I really would like the government more involved in," Parikh said.
Might thinks ARPA-H should also explore innovations in clinical trials, which many patients and medical communities view as grindingly slow and requiring too many participants. "We can approve drugs for very tiny patient populations, even at the level of the individual," he said, while emphasizing the need for safety. But Platanias thinks the FDA has become much more flexible in recent years. In the cancer field, at least, "You now see faster approvals for more drugs. Having [more] shortcuts on clinical trial approvals is not necessarily a good idea."
With so many options on the table, ARPA-H needs to show the public a clear framework for measuring the value of potential projects. Kass warned that well-resourced advocates could skew the agency's priorities. They've affected health outcomes before, she noted; fundraising may partly explain larger increases in life expectancy for cystic fibrosis than sickle cell anemia. Engaging diverse communities is a must for ARPA-H. So are partnerships to get the agency's outputs to people who need them. "Research is half the equation," said Kass. "If we don't ensure implementation and access, who cares." The White House concept paper on ARPA-H made a similar point.
As Congress works on authorizing ARPA-H this year, Might is doing what he can to ensure better access to innovation on a patient-by-patient basis. Last year, his son, Bertrand, passed away suddenly from his disorder. He was 12. But Might's sense of urgency has persisted, as he directs the Precision Medicine Institute at the University of Alabama-Birmingham. That urgency "can be carried into an agency like ARPA-H," he said. "It guides what I do as I apply for funding, because I'm trying to build the infrastructure that other parents need. So they don't have to build it from scratch like I did."
Donna Shirley pictured at her home in Tulsa, with a model of the Sojourner rover she was in charge of that explored Mars.
When NASA's Perseverance rover landed successfully on Mars on February 18, 2021, calling it "one giant leap for mankind" – as Neil Armstrong said when he set foot on the moon in 1969 – would have been inaccurate. This year actually marked the fifth time the U.S. space agency has put a remote-controlled robotic exploration vehicle on the Red Planet. And it was a female engineer named Donna Shirley who broke new ground for women in science as the manager of both the Mars Exploration Program and the 30-person team that built Sojourner, the first rover to land on Mars on July 4, 1997.
For Shirley, the Mars Pathfinder mission was the climax of her 32-year career at NASA's Jet Propulsion Laboratory (JPL) in Pasadena, California. The Oklahoma-born scientist, who earned her Master's degree in aerospace engineering from the University of Southern California, saw her profile skyrocket with media appearances from CNN to the New York Times, and her autobiography Managing Martians came out in 1998. Now 79 and living in a Tulsa retirement community, she still embraces her status as a female pioneer.
"Periodically, I'll hear somebody say they got into the space program because of me, and that makes me feel really good," Shirley told Leaps.org. "I look at the mission control area, and there are a lot of women in there. I'm quite pleased I was able to break the glass ceiling."
Her $25-million, 25-pound microrover – powered by solar energy and designed to get rock samples and test soil chemistry for evidence of life – was named after Sojourner Truth, a 19th-century Black abolitionist and women's rights activist. Unlike Mars Pathfinder, Shirley didn't have to travel more than 131 million miles to reach her goal, but her path to scientific fame as a woman sometimes resembled an asteroid field.
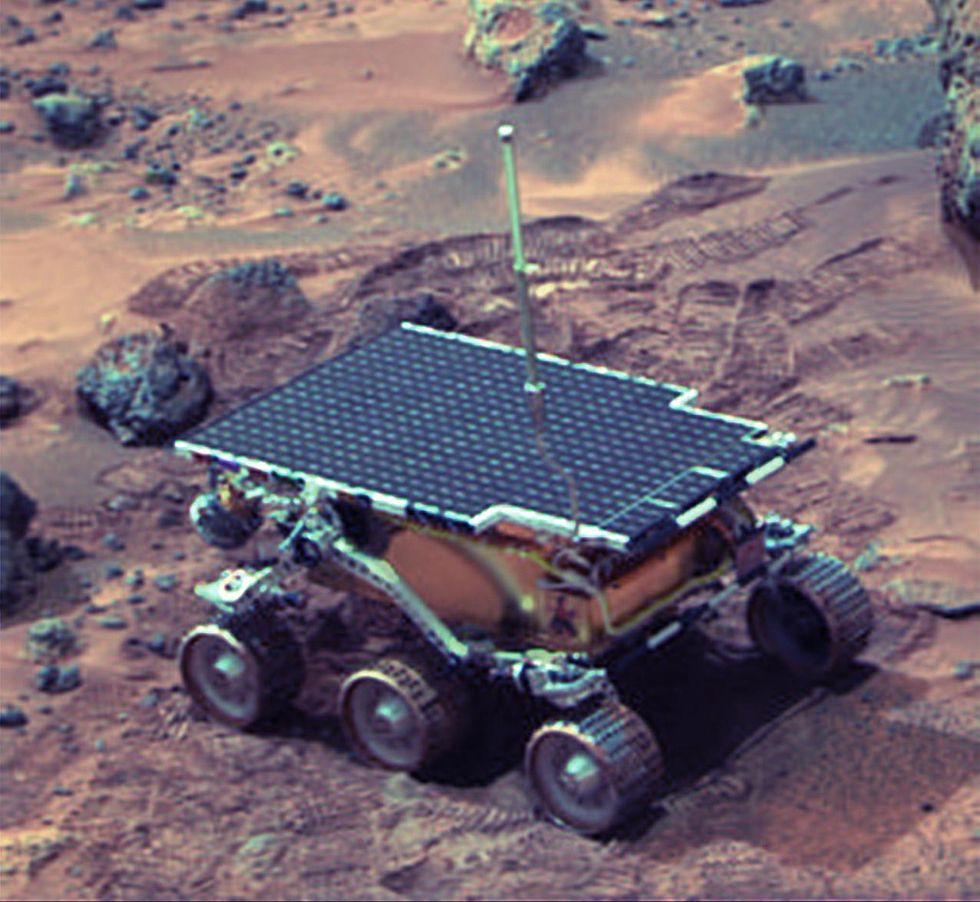 The Sojourner Rover in 1997 on Mars.NASA/JPL
The Sojourner Rover in 1997 on Mars.NASA/JPLAs a high-IQ tomboy growing up in Wynnewood, Oklahoma (pop. 2,300), Shirley yearned to escape. She decided to become an engineer at age 10 and took flying lessons at 15. Her extraterrestrial aspirations were fueled by Ray Bradbury's The Martian Chronicles and Arthur C. Clarke's The Sands of Mars. Yet when she entered the University of Oklahoma (OU) in 1958, her freshman academic advisor initially told her: "Girls can't be engineers." She ignored him.
Years later, Shirley would combat such archaic thinking, succeeding at JPL with her creative, collaborative management style. "If you look at the literature, you'll find that teams that are either led by or heavily involved with women do better than strictly male teams," she noted.
However, her career trajectory stalled at OU. Burned out by her course load and distracted by a broken engagement to marry a fellow student, she switched her major to professional writing. After graduation, she applied her aeronautical background as a McDonnell Aircraft technical writer, but her boss, she says, harassed her and she faced gender-based hostility from male co-workers.
Returning to OU, Shirley finished off her engineering degree and became a JPL aerodynamist in 1966 after answering an ad in the St. Louis Post-Dispatch. At first, she was the only female engineer among the research center's 2,000-odd engineers. She wore many hats, from designing planetary atmospheric entry vehicles to picking the launch date of November 4, 1973 for Mariner 10's mission to Venus and Mercury.
By the mid-1980's, she was managing teams that focused on robotics and Mars, delivering creative solutions when NASA budget cuts loomed. In 1989, the same year the Sojourner microrover concept was born, President George H.W. Bush announced his Space Exploration Initiative, including plans for a human mission to Mars by 2019.
That target, of course, wasn't attained, despite huge advances in technology and our understanding of the Martian environment. Today, Shirley believes humans could land on Mars by 2030. She became the founding director of the Science Fiction Museum and Hall of Fame in Seattle in 2004 after leaving NASA, and to this day, she enjoys checking out pop culture portrayals of Mars landings – even if they're not always accurate.
After the novel The Martian was published in 2011, which later was adapted into the hit film starring Matt Damon, Shirley phoned author Andy Weir: "You've got a major mistake in here. It says there's a storm that tries to blow the rocket over. But actually, the Mars atmosphere is so thin, it would never blow a rocket over!"
Fearlessly speaking her mind and seeking the stars helped Donna Shirley make history. However, a 2019 Washington Post story noted: "Women make up only about a third of NASA's workforce. They comprise just 28 percent of senior executive leadership positions and are only 16 percent of senior scientific employees." Whether it's traveling to Mars or trending toward gender equality, we've still got a long way to go.
Announcing March Event: "COVID Vaccines and the Return to Life: Part 1"
Leading medical and scientific experts will discuss the latest developments around the COVID-19 vaccines at our March 11th event.
EVENT INFORMATION
DATE:
Thursday, March 11th, 2021 at 12:30pm - 1:45pm EST
On the one-year anniversary of the global declaration of the pandemic, this virtual event will convene leading scientific and medical experts to discuss the most pressing questions around the COVID-19 vaccines. Planned topics include the effect of the new circulating variants on the vaccines, what we know so far about transmission dynamics post-vaccination, how individuals can behave post-vaccination, the myths of "good" and "bad" vaccines as more alternatives come on board, and more. A public Q&A will follow the expert discussion.
CONTACT:
kira@goodinc.com
LOCATION:
Zoom webinar
SPEAKERS:

Dr. Paul Offit speaking at Communicating Vaccine Science.
commons.wikimedia.orgDr. Paul Offit, M.D., is the director of the Vaccine Education Center and an attending physician in infectious diseases at the Children's Hospital of Philadelphia. He is a co-inventor of the rotavirus vaccine for infants, and he has lent his expertise to the advisory committees that review data on new vaccines for the CDC and FDA.

Dr. Monica Gandhi
UCSF Health
Dr. Monica Gandhi, M.D., MPH, is Professor of Medicine and Associate Division Chief (Clinical Operations/ Education) of the Division of HIV, Infectious Diseases, and Global Medicine at UCSF/ San Francisco General Hospital.

Dr. Onyema Ogbuagu, MBBCh, FACP, FIDSA
Yale Medicine
Dr. Onyema Ogbuagu, MBBCh, is an infectious disease physician at Yale Medicine who treats COVID-19 patients and leads Yale's clinical studies around COVID-19. He ran Yale's trial of the Pfizer/BioNTech vaccine.

Dr. Eric Topol
Dr. Topol's Twitter
Dr. Eric Topol, M.D., is a cardiologist, scientist, professor of molecular medicine, and the director and founder of Scripps Research Translational Institute. He has led clinical trials in over 40 countries with over 200,000 patients and pioneered the development of many routinely used medications.
REGISTER NOW
This event is the first of a four-part series co-hosted by LeapsMag, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.

Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.