Artificial Intelligence Needs Doctors As Much As They Need It

In this futuristic medical concept, a doctor assesses a patient with robust machine assistance.
The media loves to hype concerns about artificial intelligence: What if machines become super-intelligent and self-aware? How will humanity compete and survive? But artificial intelligence today is a far cry from a robot takeover. "AI" is a catch-all term that often refers to machine training or machine learning: There is an abundance of data, vastly more than the human mind can assimilate, being tagged, captured and stored. This systematic data processing requires methodologies that can put it in usable form and formats. While these new developments stoke fear in some corners, the ability to predict outcomes is generally seen as a good thing, as it can mitigate risks and even save lives.
We, collectively, want AI even though it is seldom expressed this way.
The prospects and attempts toward artificial intelligence has been with us for decades. Only recently have the underlying technologies and infrastructure--including computer processing, storage, networking speed and advanced software platforms--become omnipresent. These technological advances enabled the implementation of data mining concepts and the subsequent advantages that were not feasible just a decade ago.
AI is fantastical by vision, evolutionary by experience, and disruptive upon reflection. In the world of health care, AI is already transforming research and clinical practice. We, collectively, want AI even though it is seldom expressed this way. What we, the patient population, patient advocates and caregivers, agree on and want is: (1) timely, precise and inexpensive diagnoses of our ailments, injuries and disorders; (2) timely, personalized, highly effective and efficient courses of therapies; and (3) expedited recovery with minimum deficits, complications and recurrence.
"Artificial intelligence and machine learning will impact healthcare as profoundly as the discovery of the microscope."
Implicitly, we all are saying that we want our healthcare systems and clinicians to accomplish truly inhuman feats: to incorporate all sources of structured data (such as published statistics and reports) and unstructured data (including news articles, conversational analysis by care givers, nuances of similar cases, talks at professional societies); to analyze the data sourced and uncover patterns, reveal side effects, define probable success and outcomes; and to present the best personalized course of treatment for the patient that addresses the ailment and mitigates associated risks. It is hard to argue against any of this.
In a recent published interview, Keith J. Dreyer, executive director of the Massachusetts General Hospital and Brigham and Women's Hospital Center for Clinical Data Science, says that "artificial intelligence and machine learning will impact healthcare as profoundly as the discovery of the microscope."
But as AI helps physicians in profound ways, like detecting subtle lesions on scans or distinguishing the symptoms of a stroke from a brain tumor, we humans can't get too complacent. Evolving AI platforms will provide more sophisticated sets of "tools" to address both mundane and complex medical challenges, albeit with humans very much in the mix and routinely at the helm.
Humans do not appear endangered to be replaced anytime soon.
Human beings are capable of a level of nuance and contextual understanding of complex medical scenarios and, consequently, do not appear endangered to be replaced anytime soon. These platforms will do some heavy lifting for sure and provide considerable assistance across the healthcare industry. But human involvement is crucial, as we are best at adaptive learning, cognition, ensuring accuracy of the data, and continually providing feedback to improve the machine learning components of the AI platforms that the health industry will increasingly rely upon.
The human/machine interface is not binary; there is no line in the sand. It is fuzzy and evolutionary, a synchronicity that we all will surely witness and experience. In the future, it may be possible that all recorded knowledge, including genetic, genomic and laboratory data, from structured and unstructured sources, can be at the fingertips of your clinician, and then factored into diagnosing your condition and prescribing your course of treatment. This is precision and personalized medicine on a grand scale applied at the micro level--you!
But none of this will diminish the importance of doctors, nurses and all assortment of care providers. Though they all will undoubtedly become more effective with such awesome AI assistance, their job will always be to heal you with compassion, wisdom, and kindness, for the essence of humanity cannot be automated.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
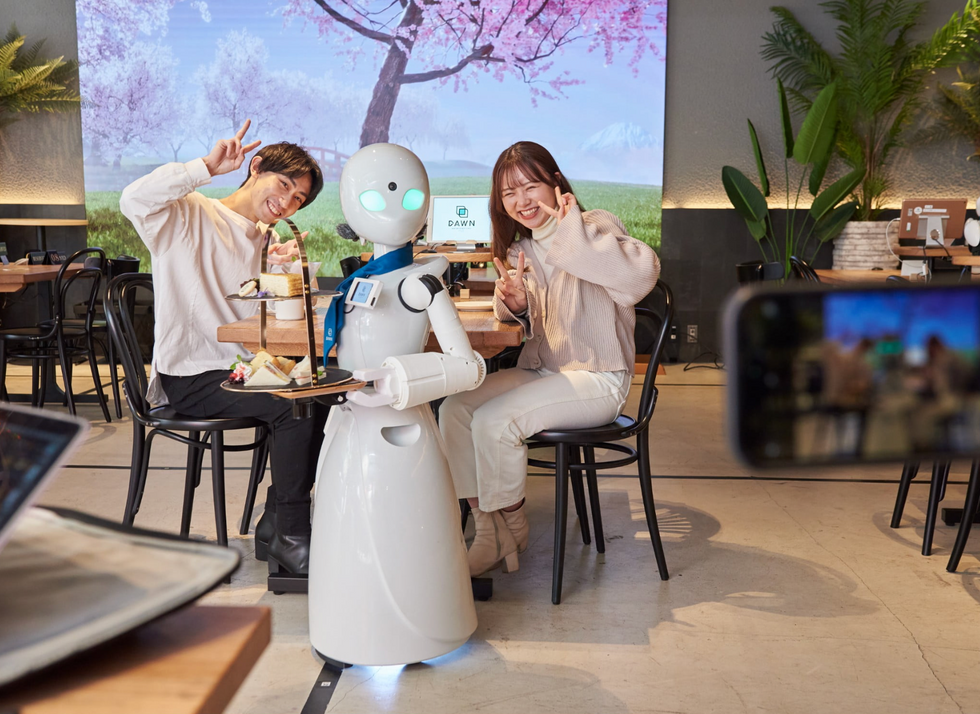
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

