Don’t fear AI, fear power-hungry humans

Story by Big Think
We live in strange times, when the technology we depend on the most is also that which we fear the most. We celebrate cutting-edge achievements even as we recoil in fear at how they could be used to hurt us. From genetic engineering and AI to nuclear technology and nanobots, the list of awe-inspiring, fast-developing technologies is long.
However, this fear of the machine is not as new as it may seem. Technology has a longstanding alliance with power and the state. The dark side of human history can be told as a series of wars whose victors are often those with the most advanced technology. (There are exceptions, of course.) Science, and its technological offspring, follows the money.
This fear of the machine seems to be misplaced. The machine has no intent: only its maker does. The fear of the machine is, in essence, the fear we have of each other — of what we are capable of doing to one another.
How AI changes things
Sure, you would reply, but AI changes everything. With artificial intelligence, the machine itself will develop some sort of autonomy, however ill-defined. It will have a will of its own. And this will, if it reflects anything that seems human, will not be benevolent. With AI, the claim goes, the machine will somehow know what it must do to get rid of us. It will threaten us as a species.
Well, this fear is also not new. Mary Shelley wrote Frankenstein in 1818 to warn us of what science could do if it served the wrong calling. In the case of her novel, Dr. Frankenstein’s call was to win the battle against death — to reverse the course of nature. Granted, any cure of an illness interferes with the normal workings of nature, yet we are justly proud of having developed cures for our ailments, prolonging life and increasing its quality. Science can achieve nothing more noble. What messes things up is when the pursuit of good is confused with that of power. In this distorted scale, the more powerful the better. The ultimate goal is to be as powerful as gods — masters of time, of life and death.
Should countries create a World Mind Organization that controls the technologies that develop AI?
Back to AI, there is no doubt the technology will help us tremendously. We will have better medical diagnostics, better traffic control, better bridge designs, and better pedagogical animations to teach in the classroom and virtually. But we will also have better winnings in the stock market, better war strategies, and better soldiers and remote ways of killing. This grants real power to those who control the best technologies. It increases the take of the winners of wars — those fought with weapons, and those fought with money.
A story as old as civilization
The question is how to move forward. This is where things get interesting and complicated. We hear over and over again that there is an urgent need for safeguards, for controls and legislation to deal with the AI revolution. Great. But if these machines are essentially functioning in a semi-black box of self-teaching neural nets, how exactly are we going to make safeguards that are sure to remain effective? How are we to ensure that the AI, with its unlimited ability to gather data, will not come up with new ways to bypass our safeguards, the same way that people break into safes?
The second question is that of global control. As I wrote before, overseeing new technology is complex. Should countries create a World Mind Organization that controls the technologies that develop AI? If so, how do we organize this planet-wide governing board? Who should be a part of its governing structure? What mechanisms will ensure that governments and private companies do not secretly break the rules, especially when to do so would put the most advanced weapons in the hands of the rule breakers? They will need those, after all, if other actors break the rules as well.
As before, the countries with the best scientists and engineers will have a great advantage. A new international détente will emerge in the molds of the nuclear détente of the Cold War. Again, we will fear destructive technology falling into the wrong hands. This can happen easily. AI machines will not need to be built at an industrial scale, as nuclear capabilities were, and AI-based terrorism will be a force to reckon with.
So here we are, afraid of our own technology all over again.
What is missing from this picture? It continues to illustrate the same destructive pattern of greed and power that has defined so much of our civilization. The failure it shows is moral, and only we can change it. We define civilization by the accumulation of wealth, and this worldview is killing us. The project of civilization we invented has become self-cannibalizing. As long as we do not see this, and we keep on following the same route we have trodden for the past 10,000 years, it will be very hard to legislate the technology to come and to ensure such legislation is followed. Unless, of course, AI helps us become better humans, perhaps by teaching us how stupid we have been for so long. This sounds far-fetched, given who this AI will be serving. But one can always hope.
Last month, a paper published in Cell by Harvard biologist David Sinclair explored root cause of aging, as well as examining whether this process can be controlled. We talked with Dr. Sinclair about this new research.
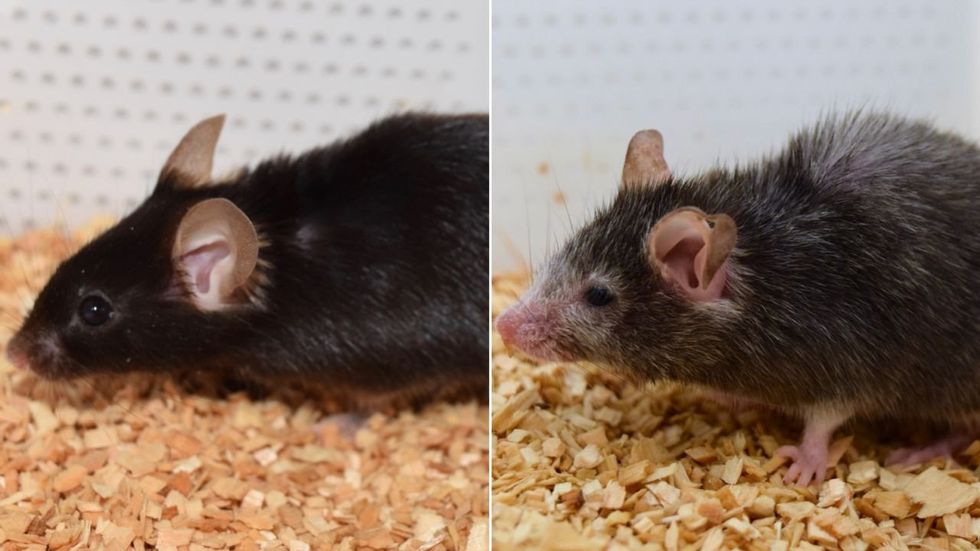
What causes aging? In a paper published last month, Dr. David Sinclair, Professor in the Department of Genetics at Harvard Medical School, reports that he and his co-authors have found the answer. Harnessing this knowledge, Dr. Sinclair was able to reverse this process, making mice younger, according to the study published in the journal Cell.
I talked with Dr. Sinclair about his new study for the latest episode of Making Sense of Science. Turning back the clock on mouse age through what’s called epigenetic reprogramming – and understanding why animals get older in the first place – are key steps toward finding therapies for healthier aging in humans. We also talked about questions that have been raised about the research.
Show links:
Dr. Sinclair's paper, published last month in Cell.
Recent pre-print paper - not yet peer reviewed - showing that mice treated with Yamanaka factors lived longer than the control group.
Dr. Sinclair's podcast.
Previous research on aging and DNA mutations.
Dr. Sinclair's book, Lifespan.

Harvard Medical School
Breakthrough therapies are breaking patients' banks. Key changes could improve access, experts say.
Single-treatment therapies are revolutionizing medicine. But insurers and patients wonder whether they can afford treatment and, if they can, whether the high costs are worthwhile.
CSL Behring’s new gene therapy for hemophilia, Hemgenix, costs $3.5 million for one treatment, but helps the body create substances that allow blood to clot. It appears to be a cure, eliminating the need for other treatments for many years at least.
Likewise, Novartis’s Kymriah mobilizes the body’s immune system to fight B-cell lymphoma, but at a cost $475,000. For patients who respond, it seems to offer years of life without the cancer progressing.
These single-treatment therapies are at the forefront of a new, bold era of medicine. Unfortunately, they also come with new, bold prices that leave insurers and patients wondering whether they can afford treatment and, if they can, whether the high costs are worthwhile.
“Most pharmaceutical leaders are there to improve and save people’s lives,” says Jeremy Levin, chairman and CEO of Ovid Therapeutics, and immediate past chairman of the Biotechnology Innovation Organization. If the therapeutics they develop are too expensive for payers to authorize, patients aren’t helped.
“The right to receive care and the right of pharmaceuticals developers to profit should never be at odds,” Levin stresses. And yet, sometimes they are.
Leigh Turner, executive director of the bioethics program, University of California, Irvine, notes this same tension between drug developers that are “seeking to maximize profits by charging as much as the market will bear for cell and gene therapy products and other medical interventions, and payers trying to control costs while also attempting to provide access to medical products with promising safety and efficacy profiles.”
Why Payers Balk
Health insurers can become skittish around extremely high prices, yet these therapies often accompany significant overall savings. For perspective, the estimated annual treatment cost for hemophilia exceeds $300,000. With Hemgenix, payers would break even after about 12 years.
But, in 12 years, will the patient still have that insurer? Therein lies the rub. U.S. payers, are used to a “pay-as-you-go” model, in which the lifetime costs of therapies typically are shared by multiple payers over many years, as patients change jobs. Single treatment therapeutics eliminate that cost-sharing ability.
"As long as formularies are based on profits to middlemen…Americans’ healthcare costs will continue to skyrocket,” says Patricia Goldsmith, the CEO of CancerCare.
“There is a phenomenally complex, bureaucratic reimbursement system that has grown, layer upon layer, during several decades,” Levin says. As medicine has innovated, payment systems haven’t kept up.
Therefore, biopharma companies begin working with insurance companies and their pharmacy benefit managers (PBMs), which act on an insurer’s behalf to decide which drugs to cover and by how much, early in the drug approval process. Their goal is to make sophisticated new drugs available while still earning a return on their investment.
New Payment Models
Pay-for-performance is one increasingly popular strategy, Turner says. “These models typically link payments to evidence generation and clinically significant outcomes.”
A biotech company called bluebird bio, for example, offers value-based pricing for Zynteglo, a $2.8 million possible cure for the rare blood disorder known as beta thalassaemia. It generally eliminates patients’ need for blood transfusions. The company is so sure it works that it will refund 80 percent of the cost of the therapy if patients need blood transfusions related to that condition within five years of being treated with Zynteglo.
In his February 2023 State of the Union speech, President Biden proposed three pilot programs to reduce drug costs. One of them, the Cell and Gene Therapy Access Model calls on the federal Centers for Medicare & Medicaid Services to establish outcomes-based agreements with manufacturers for certain cell and gene therapies.
A mortgage-style payment system is another, albeit rare, approach. Amortized payments spread the cost of treatments over decades, and let people change employers without losing their healthcare benefits.
Only about 14 percent of all drugs that enter clinical trials are approved by the FDA. Pharma companies, therefore, have an exigent need to earn a profit.
The new payment models that are being discussed aren’t solutions to high prices, says Bill Kramer, senior advisor for health policy at Purchaser Business Group on Health (PBGH), a nonprofit that seeks to lower health care costs. He points out that innovative pricing models, although well-intended, may distract from the real problem of high prices. They are attempts to “soften the blow. The best thing would be to charge a reasonable price to begin with,” he says.
Instead, he proposes making better use of research on cost and clinical effectiveness. The Institute for Clinical and Economic Review (ICER) conducts such research in the U.S., determining whether the benefits of specific drugs justify their proposed prices. ICER is an independent non-profit research institute. Its reports typically assess the degrees of improvement new therapies offer and suggest prices that would reflect that. “Publicizing that data is very important,” Kramer says. “Their results aren’t used to the extent they could and should be.” Pharmaceutical companies tend to price their therapies higher than ICER’s recommendations.
Drug Development Costs Soar
Drug developers have long pointed to the onerous costs of drug development as a reason for high prices.
A 2020 study found the average cost to bring a drug to market exceeded $1.1 billion, while other studies have estimated overall costs as high as $2.6 billion. The development timeframe is about 10 years. That’s because modern therapeutics target precise mechanisms to create better outcomes, but also have high failure rates. Only about 14 percent of all drugs that enter clinical trials are approved by the FDA. Pharma companies, therefore, have an exigent need to earn a profit.
Skewed Incentives Increase Costs
Pricing isn’t solely at the discretion of pharma companies, though. “What patients end up paying has much more to do with their PBMs than the actual price of the drug,” Patricia Goldsmith, CEO, CancerCare, says. Transparency is vital.
PBMs control patients’ access to therapies at three levels, through price negotiations, pricing tiers and pharmacy management.
When negotiating with drug manufacturers, Goldsmith says, “PBMs exchange a preferred spot on a formulary (the insurer’s or healthcare provider’s list of acceptable drugs) for cash-base rebates.” Unfortunately, 25 percent of the time, those rebates are not passed to insurers, according to the PBGH report.
Then, PBMs use pricing tiers to steer patients and physicians to certain drugs. For example, Kramer says, “Sometimes PBMs put a high-cost brand name drug in a preferred tier and a lower-cost competitor in a less preferred, higher-cost tier.” As the PBGH report elaborates, “(PBMs) are incentivized to include the highest-priced drugs…since both manufacturing rebates, as well as the administrative fees they charge…are calculated as a percentage of the drug’s price.
Finally, by steering patients to certain pharmacies, PBMs coordinate patients’ access to treatments, control patients’ out-of-pocket costs and receive management fees from the pharmacies.
Therefore, Goldsmith says, “As long as formularies are based on profits to middlemen…Americans’ healthcare costs will continue to skyrocket.”
Transparency into drug pricing will help curb costs, as will new payment strategies. What will make the most impact, however, may well be the development of a new reimbursement system designed to handle dramatic, breakthrough drugs. As Kramer says, “We need a better system to identify drugs that offer dramatic improvements in clinical care.”