Did Anton the AI find a new treatment for a deadly cancer?
Researchers used a supercomputer to learn about the subtle movement of a cancer-causing molecule, and then they found the precise drug that can recognize that motion.
Bile duct cancer is a rare and aggressive form of cancer that is often difficult to diagnose. Patients with advanced forms of the disease have an average life expectancy of less than two years.
Many patients who get cancer in their bile ducts – the tubes that carry digestive fluid from the liver to the small intestine – have mutations in the protein FGFR2, which leads cells to grow uncontrollably. One treatment option is chemotherapy, but it’s toxic to both cancer cells and healthy cells, failing to distinguish between the two. Increasingly, cancer researchers are focusing on biomarker directed therapy, or making drugs that target a particular molecule that causes the disease – FGFR2, in the case of bile duct cancer.
A problem is that in targeting FGFR2, these drugs inadvertently inhibit the FGFR1 protein, which looks almost identical. This causes elevated phosphate levels, which is a sign of kidney damage, so doses are often limited to prevent complications.
In recent years, though, a company called Relay has taken a unique approach to picking out FGFR2, using a powerful supercomputer to simulate how proteins move and change shape. The team, leveraging this AI capability, discovered that FGFR2 and FGFR1 move differently, which enabled them to create a more precise drug.
Preliminary studies have shown robust activity of this drug, called RLY-4008, in FGFR2 altered tumors, especially in bile duct cancer. The drug did not inhibit FGFR1 or cause significant side effects. “RLY-4008 is a prime example of a precision oncology therapeutic with its highly selective and potent targeting of FGFR2 genetic alterations and resistance mutations,” says Lipika Goyal, assistant professor of medicine at Harvard Medical School. She is a principal investigator of Relay’s phase 1-2 clinical trial.
Boosts from AI and a billionaire
Traditional drug design has been very much a case of trial and error, as scientists investigate many molecules to see which ones bind to the intended target and bind less to other targets.
“It’s being done almost blindly, without really being guided by structure, so it fails very often,” says Olivier Elemento, associate director of the Institute for Computational Biomedicine at Cornell. “The issue is that they are not sampling enough molecules to cover some of the chemical space that would be specific to the target of interest and not specific to others.”
Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
Some scientists have tried to use X-rays of crystallized proteins to look at the structure of proteins and design better drugs. But they have failed to account for an important factor: proteins are moving and constantly folding into different shapes.
David Shaw, a hedge fund billionaire, wanted to help improve drug discovery and understood that a key obstacle was that computer models of molecular dynamics were limited; they simulated motion for less than 10 millionths of a second.
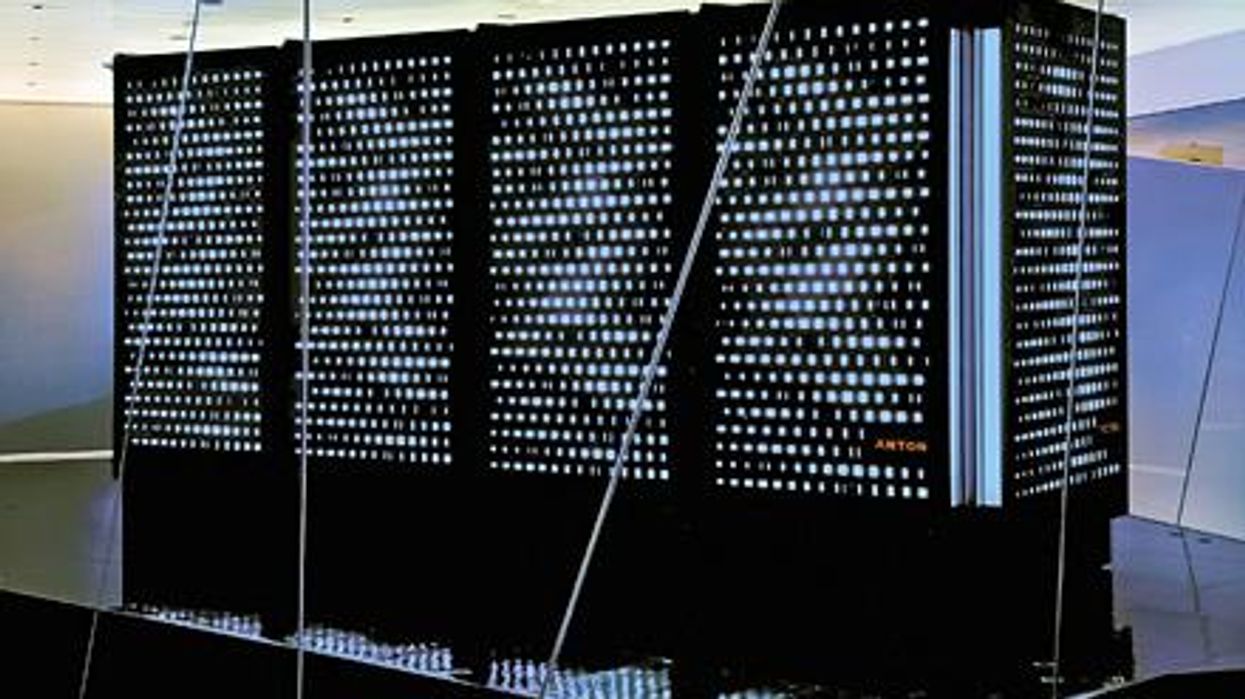
In 2001, Shaw set up his own research facility, D.E. Shaw Research, to create a supercomputer that would be specifically designed to simulate protein motion. Seven years later, he succeeded in firing up a supercomputer that can now conduct high speed simulations roughly 100 times faster than others. Called Anton, it has special computer chips to enable this speed, and its software is powered by AI to conduct many simulations.
After creating the supercomputer, Shaw teamed up with leading scientists who were interested in molecular motion, and they founded Relay Therapeutics.
Elemento believes that Relay’s approach is highly beneficial in designing a better drug for bile duct cancer. “Relay Therapeutics has a cutting-edge approach for molecular dynamics that I don’t believe any other companies have, at least not as advanced.” Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
How it works
Relay used both experimental and computational approaches to design RLY-4008. The team started out by taking X-rays of crystallized versions of both their intended target, FGFR2, and the almost identical FGFR1. This enabled them to get a 3D snapshot of each of their structures. They then fed the X-rays into the Anton supercomputer to simulate how the proteins were likely to move.
Anton’s simulations showed that the FGFR1 protein had a flap that moved more frequently than FGFR2. Based on this distinct motion, the team tried to design a compound that would recognize this flap shifting around and bind to FGFR2 while steering away from its more active lookalike.
For that, they went back Anton, using the supercomputer to simulate the behavior of thousands of potential molecules for over a year, looking at what made a particular molecule selective to the target versus another molecule that wasn’t. These insights led them to determine the best compounds to make and test in the lab and, ultimately, they found that RLY-4008 was the most effective.
Promising results so far
Relay began phase 1-2 trials in 2020 and will continue until 2024. Preliminary results showed that, in the 17 patients taking a 70 mg dose of RLY-4008, the drug worked to shrink tumors in 88 percent of patients. This was a significant increase compared to other FGFR inhibitors. For instance, Futibatinib, which recently got FDA approval, had a response rate of only 42 percent.
Across all dose levels, RLY-4008 shrank tumors by 63 percent in 38 patients. In more good news, the drug didn’t elevate their phosphate levels, which suggests that it could be taken without increasing patients’ risk for kidney disease.
“Objectively, this is pretty remarkable,” says Elemento. “In a small patient study, you have a molecule that is able to shrink tumors in such a high fraction of patients. It is unusual to see such good results in a phase 1-2 trial.”
A simulated future
The research team is continuing to use molecular dynamic simulations to develop other new drug, such as one that is being studied in patients with solid tumors and breast cancer.
As for their bile duct cancer drug, RLY-4008, Relay plans by 2024 to have tested it in around 440 patients. “The mature results of the phase 1-2 trial are highly anticipated,” says Goyal, the principal investigator of the trial.
Sameek Roychowdhury, an oncologist and associate professor of internal medicine at Ohio State University, highlights the need for caution. “This has early signs of benefit, but we will look forward to seeing longer term results for benefit and side effect profiles. We need to think a few more steps ahead - these treatments are like the ’Whack-a-Mole game’ where cancer finds a way to become resistant to each subsequent drug.”
“I think the issue is going to be how durable are the responses to the drug and what are the mechanisms of resistance,” says Raymond Wadlow, an oncologist at the Inova Medical Group who specializes in gastrointestinal and haematological cancer. “But the results look promising. It is a much more selective inhibitor of the FGFR protein and less toxic. It’s been an exciting development.”
Urinary tract infections account for more than 8 million trips to the doctor each year.
Few things are more painful than a urinary tract infection (UTI). Common in men and women, these infections account for more than 8 million trips to the doctor each year and can cause an array of uncomfortable symptoms, from a burning feeling during urination to fever, vomiting, and chills. For an unlucky few, UTIs can be chronic—meaning that, despite treatment, they just keep coming back.
But new research, presented at the European Association of Urology (EAU) Congress in Paris this week, brings some hope to people who suffer from UTIs.
Clinicians from the Royal Berkshire Hospital presented the results of a long-term, nine-year clinical trial where 89 men and women who suffered from recurrent UTIs were given an oral vaccine called MV140, designed to prevent the infections. Every day for three months, the participants were given two sprays of the vaccine (flavored to taste like pineapple) and then followed over the course of nine years. Clinicians analyzed medical records and asked the study participants about symptoms to check whether any experienced UTIs or had any adverse reactions from taking the vaccine.
The results showed that across nine years, 48 of the participants (about 54%) remained completely infection-free. On average, the study participants remained infection free for 54.7 months—four and a half years.
“While we need to be pragmatic, this vaccine is a potential breakthrough in preventing UTIs and could offer a safe and effective alternative to conventional treatments,” said Gernot Bonita, Professor of Urology at the Alta Bro Medical Centre for Urology in Switzerland, who is also the EAU Chairman of Guidelines on Urological Infections.
The news comes as a relief not only for people who suffer chronic UTIs, but also to doctors who have seen an uptick in antibiotic-resistant UTIs in the past several years. Because UTIs usually require antibiotics, patients run the risk of developing a resistance to the antibiotics, making infections more difficult to treat. A preventative vaccine could mean less infections, less antibiotics, and less drug resistance overall.
“Many of our participants told us that having the vaccine restored their quality of life,” said Dr. Bob Yang, Consultant Urologist at the Royal Berkshire NHS Foundation Trust, who helped lead the research. “While we’re yet to look at the effect of this vaccine in different patient groups, this follow-up data suggests it could be a game-changer for UTI prevention if it’s offered widely, reducing the need for antibiotic treatments.”
MILESTONE: Doctors have transplanted a pig organ into a human for the first time in history
A surgeon at Massachusetts General Hospital prepares a pig organ for transplant.
Surgeons at Massachusetts General Hospital made history last week when they successfully transplanted a pig kidney into a human patient for the first time ever.
The recipient was a 62-year-old man named Richard Slayman who had been living with end-stage kidney disease caused by diabetes. While Slayman had received a kidney transplant in 2018 from a human donor, his diabetes ultimately caused the kidney to fail less than five years after the transplant. Slayman had undergone dialysis ever since—a procedure that uses an artificial kidney to remove waste products from a person’s blood when the kidneys are unable to—but the dialysis frequently caused blood clots and other complications that landed him in the hospital multiple times.
As a last resort, Slayman’s kidney specialist suggested a transplant using a pig kidney provided by eGenesis, a pharmaceutical company based in Cambridge, Mass. The highly experimental surgery was made possible with the Food and Drug Administration’s “compassionate use” initiative, which allows patients with life-threatening medical conditions access to experimental treatments.
The new frontier of organ donation
Like Slayman, more than 100,000 people are currently on the national organ transplant waiting list, and roughly 17 people die every day waiting for an available organ. To make up for the shortage of human organs, scientists have been experimenting for the past several decades with using organs from animals such as pigs—a new field of medicine known as xenotransplantation. But putting an animal organ into a human body is much more complicated than it might appear, experts say.
“The human immune system reacts incredibly violently to a pig organ, much more so than a human organ,” said Dr. Joren Madsen, director of the Mass General Transplant Center. Even with immunosuppressant drugs that suppress the body’s ability to reject the transplant organ, Madsen said, a human body would reject an animal organ “within minutes.”
So scientists have had to use gene-editing technology to change the animal organs so that they would work inside a human body. The pig kidney in Slayman’s surgery, for instance, had been genetically altered using CRISPR-Cas9 technology to remove harmful pig genes and add human ones. The kidney was also edited to remove pig viruses that could potentially infect a human after transplant.
With CRISPR technology, scientists have been able to prove that interspecies organ transplants are not only possible, but may be able to successfully work long term, too. In the past several years, scientists were able to transplant a pig kidney into a monkey and have the monkey survive for more than two years. More recently, doctors have transplanted pig hearts into human beings—though each recipient of a pig heart only managed to live a couple of months after the transplant. In one of the patients, researchers noted evidence of a pig virus in the man’s heart that had not been identified before the surgery and could be a possible explanation for his heart failure.
So far, so good
Slayman and his medical team ultimately decided to pursue the surgery—and the risk paid off. When the pig organ started producing urine at the end of the four-hour surgery, the entire operating room erupted in applause.
Slayman is currently receiving an infusion of immunosuppressant drugs to prevent the kidney from being rejected, while his doctors monitor the kidney’s function with frequent ultrasounds. Slayman is reported to be “recovering well” at Massachusetts General Hospital and is expected to be discharged within the next several days.
