Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.

Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
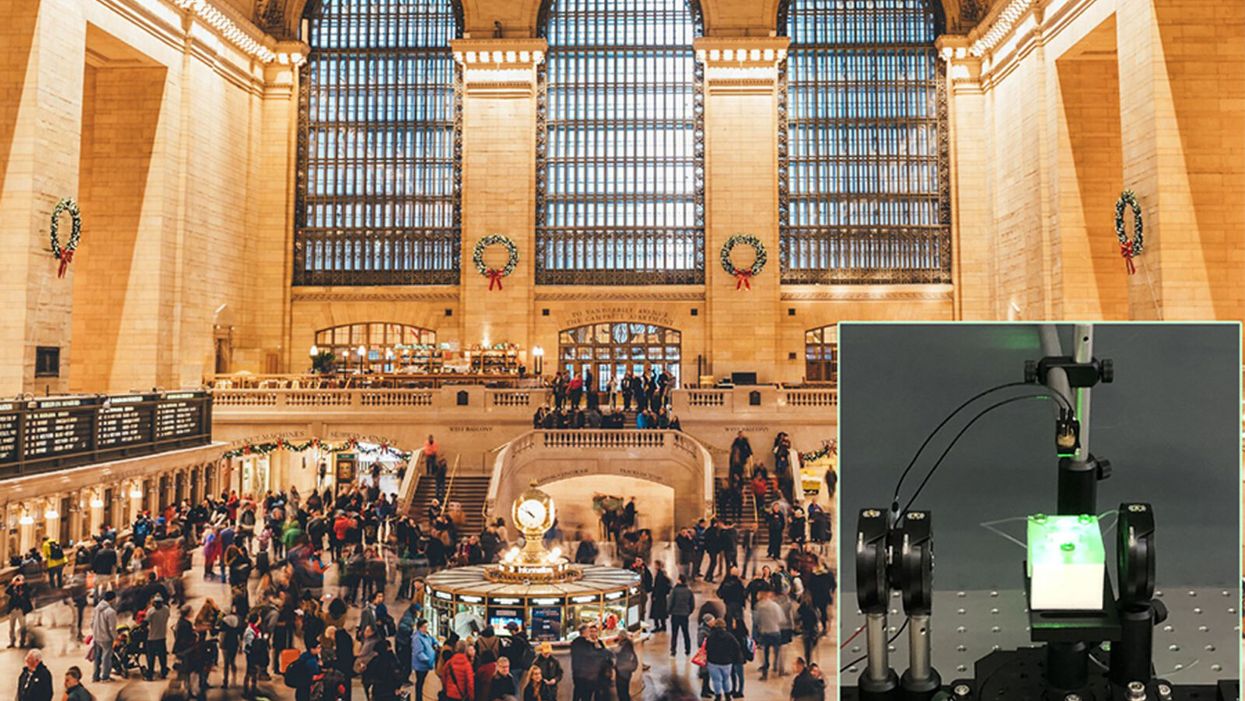
A biosensor in development (inset) could potentially be used to detect novel viruses in transit hubs like Grand Central Station in New York City.
The unprecedented scale and impact of the COVID-19 pandemic has caused scientists and engineers around the world to stop whatever they were working on and shift their research toward understanding a novel virus instead.
"We have confidence that we can use our system in the next pandemic."
For Guangyu Qiu, normally an environmental engineer at the Swiss Federal Laboratories for Materials Science and Technology, that means finding a clever way to take his work on detecting pollution in the air and apply it to living pathogens instead. He's developing a new type of biosensor to make disease diagnostics and detection faster and more accurate than what's currently available.
But even though this pandemic was the impetus for designing a new biosensor, Qiu actually has his eye on future disease outbreaks. He admits that it's unlikely his device will play a role in quelling this virus, but says researchers already need to be thinking about how to make better tools to fight the next one — because there will be a next one.
"In the last 20 years, there [have been] three different coronavirus [outbreaks] ... so we have to prepare for the coming one," Qiu says. "We have confidence that we can use our system in the next pandemic."
"A Really, Really Neat Idea"
His main concern is the diagnostic tool that's currently front and center for testing patients for SARS-Cov-2, the virus causing the novel coronavirus disease. The tool, called PCR (short for reverse transcription polymerase chain reaction), is the gold standard because it excels at detecting viruses in even very small samples of mucus. PCR can amplify genetic material in the limited sample and look for a genetic code matching the virus in question. But in many parts of the world, mucus samples have to be sent out to laboratories for that work, and results can take days to return. PCR is also notoriously prone to false positives and negatives.
"I read a lot of newspapers that report[ed] ... a lot of false negative or false positive results at the very beginning of the outbreak," Qiu says. "It's not good for protecting people to prevent further transmission of the disease."
So he set out to build a more sensitive device—one that's less likely to give you a false result. Qiu's biosensor relies on an idea similar to the dual-factor authentication required of anyone trying to access a secure webpage. Instead of verifying that a virus is really present by using one way of detecting genetic code, as with PCR, this biosensor asks for two forms of ID.
SARS-CoV-2 is what's called an RNA virus, which means it has a single strand of genetic code, unlike double-stranded DNA. Inside Qiu's biosensor are receptors with the complementary code for this particular virus' RNA; if the virus is present, its RNA will bind with the receptors, locking together like velcro. The biosensor also contains a prism and a laser that work together to verify that this RNA really belongs to SARS-CoV-2 by looking for a specific wavelength of light and temperature.
If the biosensor doesn't detect either, or only registers a match for one and not the other, then it can't produce a positive result. This multi-step authentication process helps make sure that the RNA binding with the receptors isn't a genetically similar coronavirus like SARS-CoV, known for its 2003 outbreak, or MERS-CoV, which caused an epidemic in 2012.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
Spina Bifida Claimed My Son's Mobility. Incredible Breakthroughs May Let Future Kids Run Free.
Sarah Watts's son Henry was born with spina bifida and can't stand or walk without assistance.
When our son Henry, now six, was diagnosed with spina bifida at his 20-week ultrasound, my husband and I were in shock. It took us more than a few minutes to understand what the doctor was telling us.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change.
Neither of us had any family history of birth defects. Our fifteen-month-old daughter, June, was in perfect health.
But more than that, spina bifida – a malformation of the neural tube that eventually becomes the baby's spine – is woefully complex. The defect, the doctor explained, was essentially a hole in Henry's lower spine from which his spinal nerves were protruding – and because they were exposed to my amniotic fluid, those nerves were already permanently damaged. After birth, doctors could push the nerves back into his body and sew up the hole, but he would likely experience some level of paralysis, bladder and bowel dysfunction, and a buildup of cerebrospinal fluid that would require a surgical implant called a shunt to correct. The damage was devastating – and irreversible.
We returned home with June and spent the next few days cycling between disbelief and total despair. But within a week, the maternal-fetal medicine specialist who diagnosed Henry called us up and gave us the first real optimism we had felt in days: There was a new, experimental surgery for spina bifida that was available in just a handful of hospitals around the country. Rather than waiting until birth to repair the baby's defect, some doctors were now trying out a prenatal repair, operating on the baby via c-section, closing the defect, and then keeping the mother on strict bedrest until it was time for the baby to be delivered, just before term.
This new surgery carried risks, he told us – but if it went well, there was a chance Henry wouldn't need a shunt. And because repairing the defect during my pregnancy meant the spinal nerves were exposed for a shorter amount of time, that meant we'd be preventing nerve damage – and less nerve damage meant that there was a chance he'd be able to walk.
Did we want in? the doctor asked.
Had I known more about spina bifida and the history of its treatment, this surgery would have seemed even more miraculous. Not too long ago, the standard of care for babies born with spina bifida was to simply let them die without medical treatment. In fact, it wasn't until the early 1950s that doctors even attempted to surgically repair the baby's defect at all, instead of opting to let the more severe cases die of meningitis from their open wound. (Babies who had closed spina bifida – a spinal defect covered by skin – sometimes survived past infancy, but rarely into adulthood).
But in the 1960s and 1970s, as more doctors started repairing defects and the shunting technology improved, patients with spina bifida began to survive past infancy. When catheterization was introduced, spina bifida patients who had urinary dysfunction, as is common, were able to preserve their renal function into adulthood, and they began living even longer. Within a few decades, spina bifida was no longer considered a death sentence; people were living fuller, happier lives.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change. The first major clinical trial for prenatal surgery and spina bifida, called Management of Myelomeningocele (MOMS) had just concluded, and its objective was to see whether repairing the baby's defect in utero would be beneficial. In the trial, doctors assigned eligible women to undergo prenatal surgery in the second trimester of their pregnancies and then followed up with their children throughout the first 30 months of the child's life.
The results were groundbreaking: Not only did the children in the surgery group perform better on motor skills and cognitive tests than did patients in the control group, only 40 percent of patients ended up needing shunts compared to 80 percent of patients who had postnatal surgery. The results were so overwhelmingly positive that the trial was discontinued early (and is now, happily, the medical standard of care). Our doctor relayed this information to us over the phone, breathless, and left my husband and me to make our decision.
After a few days of consideration, and despite the benefits, my husband and I actually ended up opting for the postnatal surgery instead. Prenatal surgery, although miraculous, would have required extensive travel for us, as well as giving birth in a city thousands of miles from home with no one to watch our toddler while my husband worked and I recovered. But other parents I met online throughout our pregnancy did end up choosing prenatal surgery for their children – and the majority of them now walk with little assistance and only a few require shunting.
Even more amazing to me is that now – seven years after Henry's diagnosis, and not quite a decade since the landmark MOMS trial – the standard of care could be about to change yet again.
Regardless of whether they have postnatal or prenatal surgery, most kids with spina bifida still experience some level of paralysis and rely on wheelchairs and walkers to move around. Now, researchers at UC Davis want to augment the fetal surgery with a stem cell treatment, using human placenta-derived mesenchymal stromal cells (PMSCs) and affixing them to a cellular scaffold on the baby's defect, which not only protects the spinal cord from further damage but actually encourages cellular regeneration as well.
The hope is that this treatment will restore gross motor function after the baby is born – and so far, in animal trials, that's exactly what's happening. Fetal sheep, who were induced with spinal cord injuries in utero, were born with complete motor function after receiving prenatal surgery and PMSCs. In 2017, a pair of bulldogs born with spina bifida received the stem cell treatment a few weeks after birth – and two months after surgery, both dogs could run and play freely, whereas before they had dragged their hind legs on the ground behind them. UC Davis researchers hope to bring this treatment into human clinical trials within the next year.
A century ago, a diagnosis of spina bifida meant almost certain death. Today, most children with spina bifida live into adulthood, albeit with significant disabilities. But thanks to research and innovation, it's entirely possible that within my lifetime – and certainly within Henry's – for the first time in human history, the disabilities associated with spina bifida could be a thing of the past.