Blood Donated from Recovered Coronavirus Patients May Soon Yield a Stopgap Treatment

Antibodies from the blood of recovered patients is being tested as a stopgap treatment.
In October 1918, Lieutenant L.W. McGuire of the United States Navy sent a report to the American Journal of Public Health detailing a promising therapy that had already saved the lives of a number of officers suffering from pneumonia complications due to the Spanish influenza outbreak.
"These antibodies then become essentially drugs."
McGuire described how transfusions of blood from recovered patients – an idea which had first been trialed during a polio epidemic in 1916 – had led to rapid recovery in a series of severe pneumonia cases at a Naval Hospital in Massachusetts. "It is believed the serum has a decided influence in shortening the course of the disease, and lowering the mortality," he wrote.
Now more than a century on, this treatment – long forgotten in the western world - is once again coming to the fore during the current COVID-19 pandemic. With fatalities continuing to rise, and no vaccine expected for many months, experts are urging medical centers across the U.S. and Europe to initiate collaborations between critical care and transfusion services to offer this as an emergency treatment for those who need it most.
As of March 20, there are more than 90,000 individuals globally who have recovered from the disease. Some scientists believe that the blood of many of these people contains high levels of neutralizing antibodies that can kill the virus.
"These antibodies then become essentially drugs," said Arturo Casadevall, professor of Molecular Microbiology & Immunology at John Hopkins Bloomberg School of Public Health, who is currently co-ordinating a clinical trial of convalescent serum for COVID-19 involving 20 institutions across the US.
"We're talking about preparing a therapy right out of the serum of those that have recovered. It could also be used in patients who are already sick, but have not progressed to respiratory failure, to treat them before they enter intensive care units. That will provide a lot of support because there's a limited number of respirators and resources."
The first conclusive data on how the blood of recovered patients can help tackle COVID-19 is set to come out of China, where it was also used as an emergency treatment during the SARS and MERS outbreaks. On February 9, a severely ill patient in Wuhan was treated with convalescent serum and since then, hospitals across China have used the therapy on a total of 245 patients, with 91 reportedly showing an improvement in symptoms.
In China alone, more than 58,000 patients have now recovered from COVID-19. Casadevall said that last week the country shipped 90 tons of serum and plasma from these patients to Italy – the center of the pandemic in Europe – for emergency use.
Some of the first people to be treated are likely to be doctors and nurses in hospitals who are most at risk of exposure.
A current challenge, however, is that the blood donation from the recovered patients must be precisely timed in order to maximize the number of antibodies a future patient receives. Doctors in China say that obtaining the necessary blood samples at the right time is one of the major barriers to applying the treatment on a larger scale.
"It's difficult to get the donations," said Dr. Yuan Shi of Chongqing Medical University. "When patients have recovered from the disease, we would like to collect their blood two to four weeks afterwards. We try our best to call back the patients, but it's sometimes difficult to get them to come back within that time period."
Because of such hurdles, Japan's largest drugmaker, Takeda Pharmaceuticals, is now working to turn neutralizing antibodies from recovered COVID-19 patients into a standardized drug product. They hope to launch a clinical trial for this in the next few months.
In the U.S., Casadevall hopes blood transfusions from recovered patients can become clinically available as a therapy within the next four weeks, once regulatory approval has been received. Some of the first people to be treated are likely to be doctors and nurses in hospitals who are most at risk of exposure, to provide a protective boost in their immunity.
"A lot of healthcare workers in the U.S. have already been asked to quarantine, and you can imagine what effect that's going to have on the healthcare system," he said. "It can't take large numbers of people staying home; there's not the capacity."
But not all medical experts are convinced it's the way to go, especially when it comes to the most severe cases of COVID-19. "There's no knowing whether that treatment would be useful or not," warned Dr. Andrew Freedman, head of Cardiff University's School of Medicine in the U.K.
"There are going to be better things available in a few months, but we are facing, 'What do you do now?'"
However, Casadevall says that the treatment is not envisioned as a panacea to treating coronavirus, but simply a temporary measure which could give doctors some options until stronger options such as vaccines or new drugs are available.
"This is a stopgap option," he said. "There are going to be better things available in a few months, but we are facing, 'What do you do now?' The only thing we can offer severely ill people at the moment is respiratory support and oxygen, and we don't have anything to prevent those exposed from going on and getting ill."
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
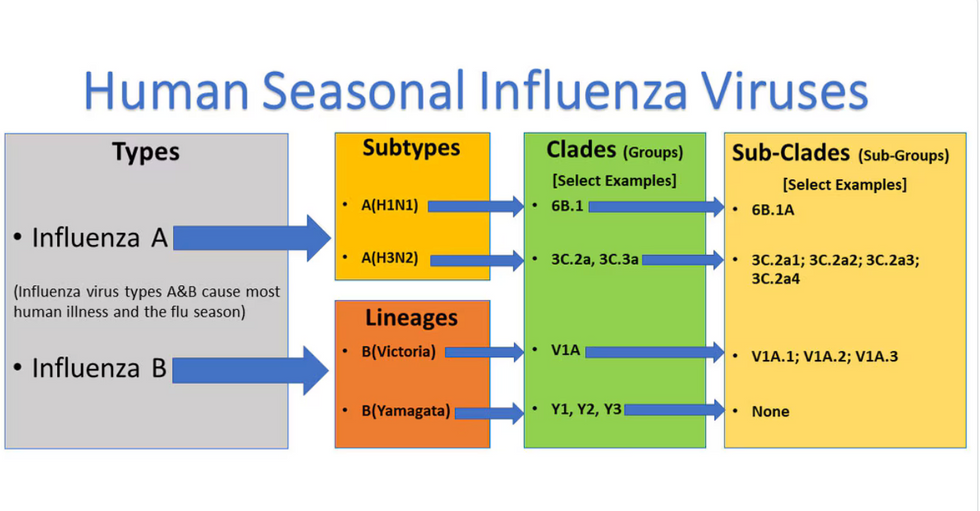
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

