Scientists and Religious Leaders Need to Be More Transparent

A steeple cross at sunset.
[Editor's Note: This essay is in response to our current Big Question series: "How can the religious and scientific communities work together to foster a culture that is equipped to face humanity's biggest challenges?"]
As a Jesuit Catholic priest, and a molecular geneticist, this question has been a fundamental part of my adult life. But first, let me address an issue that our American culture continues to struggle with: how do science and religion actually relate to each other? Is science about the "real" world, and religion just about individual or group beliefs about how the world should be?
Or are science and religion in direct competition with both trying to construct explanations of reality that are "better" or more real than the other's approach? These questions have generated much discussion among scientists, philosophers, and theologians.
The recent advances in our understanding of genetics show how combining the insights of science and religion can be beneficial.
First, we need to be clear that science and religion are two different ways human beings use to understand reality. Science focuses on observable, quantifiable, physical aspects of our universe, whereas, religion, while taking physical reality into consideration, also includes the immaterial, non-quantifiable, human experiences and concepts which relate to the meaning and purpose of existence. While scientific discoveries also often stimulate such profound reflections, these reflections are not technically a part of scientific methodology.
Second, though different in both method and focus, neither way of understanding reality produces a more "real" or accurate comprehension of our human existence. In fact, most often both science and religion add valuable insights into any particular situation, providing a more complete understanding of it as well as how it might be improved.
The recent advances in our understanding of genetics show how combining the insights of science and religion can be beneficial. For instance, the study of genetic differences among people around the world has shown us that the idea that we could accurately classify people as belonging to different races—e.g. African, Caucasian, Asian, etc.—is actually quite incorrect on a biological level. In fact, in many ways two people who appear to be of different races, perhaps African and Caucasian, could be more similar genetically than two people who appear to be of the same African race.
This scientific finding, then, challenges us to critically review the social categories some use to classify people as different from us, and, therefore, somehow of less worth to society. From this perspective, one could argue that this scientific insight synergizes well with some common fundamental religious beliefs regarding the fundamental equality all people have in their relationship to the Divine.
However, this synergy between science and religion is not what we encounter most often in the mass media or public policy debates. In part, this is due to the fact that science and religion working well together is not normally considered newsworthy. What does get attention is when science appears to conflict with religion, or, perhaps more accurately, when the scientific community conflicts with religious communities regarding how a particular scientific advance should be applied. These disagreements usually are not due to a conflict between scientific findings and religious beliefs, but rather between differing moral, social or political agendas.
One way that the two sides can work together is to prioritize honesty and accuracy in public debates instead of crafting informational campaigns to promote political advantage.
For example, genetically modified foods have been a source of controversy for the past several decades. While the various techniques used to create targeted genetic changes in plants—e.g. drought or pest resistance—are scientifically intricate and complex, explaining these techniques to the public is similar to explaining complex medical treatments to patients. Hence, the science alone is not the issue.
The controversy arises from the differing goals various stakeholders have for this technology. Obviously, companies employing this technology want it to be used around the world both for its significantly improved food production, and for improved revenue. Opponents, which have included religious communities, focus more on the social and cultural disruption this technology can create. Since a public debate between a complex technology on one side, and a complex social situation on the other side, is difficult to undertake well, the controversy has too often been reduced to sound bites such as "Frankenfoods." While such phrases may be an effective way to influence public opinion, ultimately, they work against sensible decision-making.
One way that the two sides can work together is to prioritize honesty and accuracy in public debates instead of crafting informational campaigns to promote political advantage. I recognize that presenting a thorough and honest explanation of an organization's position does not fit easily into our 24-hour-a-day-sound-bite system, but this is necessary to make the best decisions we can if we want to foster a healthier and happier world.
Climate change and human genome editing are good examples of this problem. These are both complex issues with impacts that extend well beyond just science and religious beliefs—including economics, societal disruption, and an exacerbation of social inequalities. To achieve solutions that result in significant benefits for the vast majority of people, we must work to create a knowledgeable public that is encouraged to consider the good of both one's own community as well as that of all others. This goal is actually one that both scientific and religious organizations claim to value and pursue.
The experts often fail to understand sufficiently what the public hopes, wants, and fears.
Unfortunately, both types of organizations often fall short because they focus only on informing and instructing instead of truly engaging the public in deliberation. Often both scientists and religious leaders believe that the public is not capable of sufficiently understanding the complexities of the issues, so they resort to assuming that the public should just do what the experts tell them.
However, there is significant research that demonstrates the ability of the general public to grasp complex issues in order to make sound decisions. Hence, it is the experts who often fail to understand how their messages are being received and what the public hopes, wants, and fears.
Overall, I remain sanguine about the likelihood of both religious and scientific organizations learning how to work better with each other, and together with the public. Working together for the good of all, we can integrate the insights and the desires of all stakeholders in order to face our challenges with well-informed reason and compassion for all, particularly those most in need.
[Ed. Note: Don't miss the other perspectives in this Big Question series, from a science scholar and a Rabbi/M.D.]
Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.
Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
Last month, a paper published in Cell by Harvard biologist David Sinclair explored root cause of aging, as well as examining whether this process can be controlled. We talked with Dr. Sinclair about this new research.
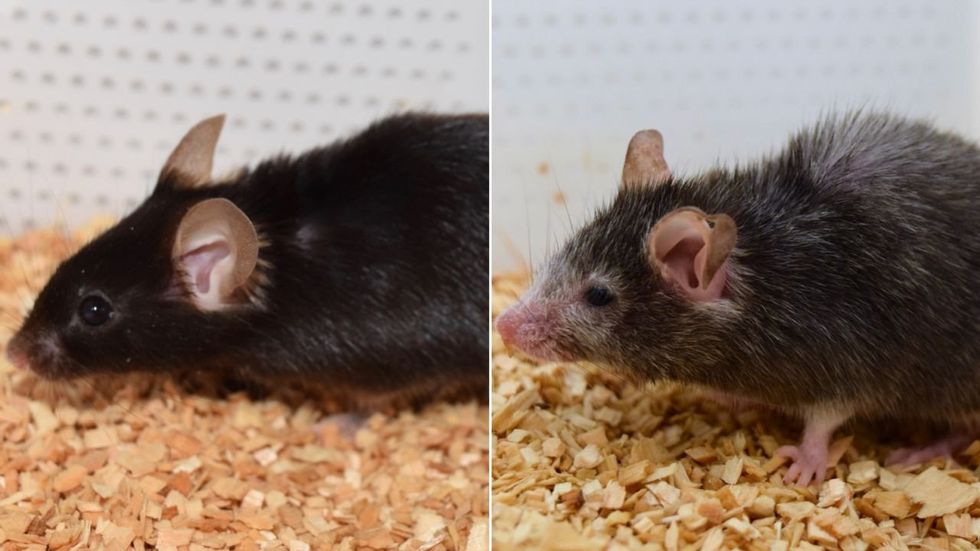
What causes aging? In a paper published last month, Dr. David Sinclair, Professor in the Department of Genetics at Harvard Medical School, reports that he and his co-authors have found the answer. Harnessing this knowledge, Dr. Sinclair was able to reverse this process, making mice younger, according to the study published in the journal Cell.
I talked with Dr. Sinclair about his new study for the latest episode of Making Sense of Science. Turning back the clock on mouse age through what’s called epigenetic reprogramming – and understanding why animals get older in the first place – are key steps toward finding therapies for healthier aging in humans. We also talked about questions that have been raised about the research.
Show links:
Dr. Sinclair's paper, published last month in Cell.
Recent pre-print paper - not yet peer reviewed - showing that mice treated with Yamanaka factors lived longer than the control group.
Dr. Sinclair's podcast.
Previous research on aging and DNA mutations.
Dr. Sinclair's book, Lifespan.

Harvard Medical School

