Can Radical Transparency Overcome Resistance to COVID-19 Vaccines?

Secretive panels of independent experts called Data Safety and Monitoring Boards examine clinical trials' data for safety and efficacy.
When historians look back on the COVID-19 pandemic, they may mark November 9, 2020 as the day the tide began to turn. That's when the New York-based pharmaceutical giant Pfizer announced that clinical trials showed its experimental vaccine, developed with the German firm BioNTech, to be 90 percent effective in preventing the disease.
A week later, Massachusetts biotech startup Moderna declared its vaccine to be 95 percent effective. By early December, Great Britain had begun mass inoculations, followed—once the Food and Drug Administration gave the thumbs-up—by the United States. In this scenario, the worst global health crisis in a century was on the cusp of resolution.
Yet future chroniclers may instead peg November 9 as the day false hope dawned. That could happen if serious safety issues, undetected so far, arise after millions of doses are administered. Experts consider it unlikely, however, that such problems alone (as opposed to the panic they might spark) would affect enough people to thwart a victory over the coronavirus. A more immediate obstacle is vaccine hesitancy—the prospect that much of the populace will refuse to roll up their sleeves.
To achieve "herd immunity" for COVID-19 (the point at which a vaccine reduces transmission rates enough to protect those who can't or won't take it, or for whom it doesn't work), epidemiologists estimate that up to 85 percent of the population will have to be vaccinated. Alarmingly, polls suggest that 40 to 50 percent of Americans intend to decline, judging the risks to be more worrisome than those posed by the coronavirus itself.
COVID vaccine skeptics occupy various positions on a spectrum of doubt. Some are committed anti-vaxxers, or devotees of conspiracy theories that view the pandemic as a hoax. Others belong to minority groups that have historically been used as guinea pigs in unethical medical research (for horrific examples, Google "Tuskegee syphilis experiment" or "Henrietta Lacks"). Still others simply mistrust Big Pharma and/or Big Government. A common fear is that the scramble to find a vaccine—intensified by partisan and profit motives—has led to corner-cutting in the testing and approval process. "They really rushed," an Iowa trucker told The Washington Post. "I'll probably wait a couple of months after they start to see how everyone else is handling it."
The COVID crisis has spurred calls for secretive Data Safety and Monitoring Boards to come out of the shadows.
The consensus among scientists, by contrast, is that the process has been rigorous enough, given the exigency of the situation, that the public can feel reasonably confident in any vaccine that has earned the imprimatur of the FDA. For those of us who share that assessment, finding ways to reassure the hesitant-but-persuadable is an urgent matter.
Vax-positive public health messaging is one obvious tactic, but a growing number of experts say it's not enough. They prescribe a regimen of radical transparency throughout the system that regulates research—in particular, regarding the secretive panels that oversee vaccine trials.
The Crucial Role of the Little-Known Panels
Like other large clinical trials involving potentially high-demand or controversial products, studies of COVID-19 vaccines in most countries are supervised by groups of independent observers. Known in the United States as data safety and monitoring boards (DSMBs), and elsewhere as data monitoring committees, these panels consist of scientists, clinicians, statisticians, and other authorities with no ties to the sponsor of the study.
The six trials funded by the federal program known as Operation Warp Speed (including those of newly approved Moderna and frontrunner AstraZeneca) share a DSMB, whose members are selected by the National Institutes of Health; other companies (including Pfizer) appoint their own. The panel's job is to monitor the safety and efficacy of a treatment while the trial is ongoing, and to ensure that data is being collected and analyzed correctly.
Vaccine studies are "double-blinded," which means neither the participants nor the doctors running the trial know who's getting the real thing and who's getting a placebo. But the DSMB can access that information if a study volunteer has what might be a serious side effect—and if the participant was in the vaccine group, the board can ask that the trial be paused for further investigation.
The DSMB also checks for efficacy at pre-determined intervals. If it finds that the vaccine group and the placebo group are getting sick at similar rates, the panel can recommend stopping the trial due to "futility." And if the results look overwhelmingly positive, the DSMB can recommend that the study sponsor apply for FDA approval before the scheduled end of the trial, in order to hurry the product to market.
With this kind of inside dope and high-level influence, DSMBs could easily become targets for outside pressure. That's why, since the 1980s, their membership has typically been kept secret.
During the early days of the AIDS crisis, researchers working on HIV drugs feared for the safety of the experts on their boards. "They didn't want them to be besieged and harassed by members of the community," explains Susan Ellenberg, a professor of biostatistics, medical ethics and health policy at the University of Pennsylvania, and co-author of Data Monitoring Committees in Clinical Trials, the DSMB bible. "You can understand why people would very much want to know how things were looking in a given trial. They wanted to save their own lives; they wanted to save their friends' lives." Ellenberg, who was founding director of the biostatistics branch of the AIDS division at the National Institute of Allergy and Infectious Diseases (NIAID), helped shape a range of policies designed to ensure that DSMBs made decisions based on data and nothing else.
Confidentiality also shields DSMB members from badgering by patient advocacy groups, who might urge that a drug be presented for approval before trial results are conclusive, or by profit-hungry investors. "It prevents people from trying to pry out information to get an edge in the stock market," says Art Caplan, a bioethicist at New York University.
Yet the COVID crisis has spurred calls for DSMBs to come out of the shadows. One triggering event came in March 2020, when the FDA approved hydroxychloroquine for COVID-19—a therapy that President Donald J. Trump touted, despite scant evidence for its efficacy. (Approval was rescinded in June.) If the agency could bow to political pressure on these medications, critics warned, it might do so with vaccines as well. In the end, that didn't happen; the Pfizer approval was issued well after Election Day, despite Trump's goading, and most experts agree that it was based on solid science. Still, public suspicion lingers.
Another shock came in September, after British-based AstraZeneca announced it was pausing its vaccine trial globally due to a "suspected adverse rection" in a volunteer. The company shared no details with the press. Instead, AstraZeneca's CEO divulged them in a private call with J.P. Morgan investors the next day, confirming that the volunteer was suffering from transverse myelitis, a rare and serious spinal inflammation—and that the study had also been halted in July, when another volunteer displayed neurological symptoms. STAT News broke the story after talking to tipsters.
Although both illnesses were found to be unrelated to the vaccine, and the trial was restarted, the incident had a paradoxical effect: while it confirmed for experts that the oversight system was working, AstraZeneca's initial lack of candor added to many laypeople's sense that it wasn't. "If you were seeking to undermine trust, that's kind of how you would go about doing it," says Charles Weijer, a bioethicist at Western University in Ontario, who has helped develop clinical trial guidelines for the World Health Organization.
Both Caplan and Weijer have served on many DSMBs; they believe the boards are generally trustworthy, and that those overseeing COVID vaccine trials are performing their jobs well. But the secrecy surrounding these groups, they and others argue, has become counterproductive. Shining a light on the statistical sausage-makers would help dispel doubts about the finished product.
"I'm not suggesting that any of these companies are doing things unethically," Weijer explains. "But the circumstances of a global pandemic are sufficiently challenging that perhaps they ought to be doing some things differently. I believe it would be trust-producing for data monitoring committees to be more forthcoming than usual."
Building Trust: More Transparency
Just how forthcoming is a matter of debate. Caplan suggests that each COVID vaccine DSMB reveal the name of its chair; that would enable the scientific community, as well as the media and the general public, to get a sense of the integrity and qualifications of the board as a whole while preserving the anonymity of the other members.
Indeed, when Operation Warp Speed's DSMB chair, Richard Whitley, was outed through a website slip-up, many observers applauded his selection for the role; a professor of pediatrics, microbiology, medicine and neurosurgery at the University of Alabama at Birmingham, he is "an exceptionally experienced and qualified individual," Weijer says. (Reporters with ProPublica later identified two other members: Susan Ellenberg and immunologist William Makgoba, known for his work on the South African AIDS Vaccine Initiative.)
Caplan would also like to see more details of the protocols DSMBs are using to make decisions, such as the statistical threshold for efficacy that would lead them to seek approval from the FDA. And he wishes the NIH would spell out specific responsibilities for these monitoring boards. "They don't really have clear, government-mandated charters," he notes. For example, there's no requirement that DSMBs include an ethicist or patient advocate—both of which Caplan considers essential for vaccine trials. "Rough guidelines," he says, "would be useful."
Weijer, for his part, thinks DSMBs should disclose all their members. "When you only disclose the chair, you leave questions unanswered," he says. "What expertise do [the others] bring to the table? Are they similarly free of relevant conflicts of interest? And it doesn't answer the question that will be foremost on many people's minds: are these people in the pocket of pharma?"
Weijer and Caplan both want to see greater transparency around the trial results themselves. Because the FDA approved the Pfizer and Moderna vaccines with emergency use authorizations rather than full licensure, which requires more extensive safety testing, these products reached the market without the usual paper trail of peer-reviewed publications. The same will likely be true of any future COVID vaccines that the agency greenlights. To add another level of scrutiny, both ethicists suggest, each company should publicly release its data at the end of a trial. "That offers the potential for academic groups to go in and do an analysis," Weijer explains, "to verify the claims about the safety and efficacy of the vaccine." The point, he says, is not only to ensure that the approval was justified, but to provide evidence to counter skeptics' qualms.
Caplan may differ on some of the details, but he endorses the premise. "It's all a matter of trust," he says. "You're always watching that, because a vaccine is only as good as the number of people who take it."
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
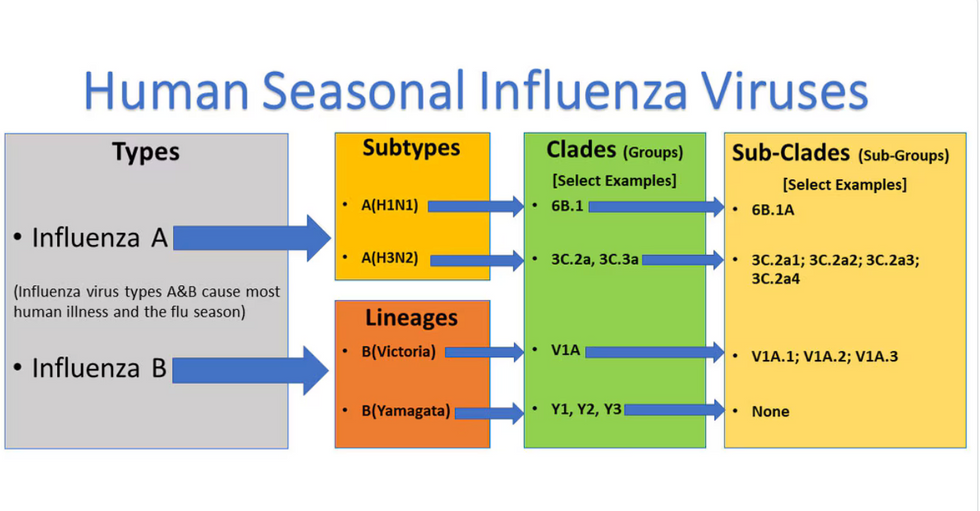
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

