Can You Trust Your Gut for Food Advice?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Which foods are actually healthy for your individual gut microbiome? Several companies are offering personalized dietary guidance based on your test results, but their answers in one experiment turned up with some conflicting advice.
I recently got on the scale to weigh myself, thinking I've got to eat better. With so many trendy diets today claiming to improve health, from Keto to Paleo to Whole30, it can be confusing to figure out what we should and shouldn't eat for optimal nutrition.
A number of companies are now selling the concept of "personalized" nutrition based on the genetic makeup of your individual gut bugs.
My next thought was: I've got to lose a few pounds.
Consider a weird factoid: In addition to my fat, skin, bone and muscle, I'm carrying around two or three pounds of straight-up bacteria. Like you, I am the host to trillions of micro-organisms that live in my gut and are collectively known as my microbiome. An explosion of research has occurred in the last decade to try to understand exactly how these microbial populations, which are unique to each of us, may influence our overall health and potentially even our brains and behavior.
Lots of mysteries still remain, but it is established that these "bugs" are crucial to keeping our body running smoothly, performing functions like stimulating the immune system, synthesizing important vitamins, and aiding digestion. The field of microbiome science is evolving rapidly, and a number of companies are now selling the concept of "personalized" nutrition based on the genetic makeup of your individual gut bugs. The two leading players are Viome and DayTwo, but the landscape includes the newly launched startup Onegevity Health and others like Thryve, which offers customized probiotic supplements in addition to dietary recommendations.
The idea has immediate appeal – if science could tell you exactly what to make for lunch and what to avoid, you could forget about the fad diets and go with your own bespoke food pyramid. Wondering if the promise might be too good to be true, I decided to perform my own experiment.
Last fall, I sent the identical fecal sample to both Viome (I paid $425, but the price has since dropped to $299) and DayTwo ($349). A couple of months later, both reports finally arrived, and I eagerly opened each app to compare their recommendations.
First, I examined my results from Viome, which was founded in 2016 in Cupertino, Calif., and declares without irony on its website that "conflicting food advice is now obsolete."
I learned I have "average" metabolic fitness and "average" inflammatory activity in my gut, which are scores that the company defines based on a proprietary algorithm. But I have "low" microbial richness, with only 62 active species of bacteria identified in my sample, compared with the mean of 157 in their test population. I also received a list of the specific species in my gut, with names like Lactococcus and Romboutsia.
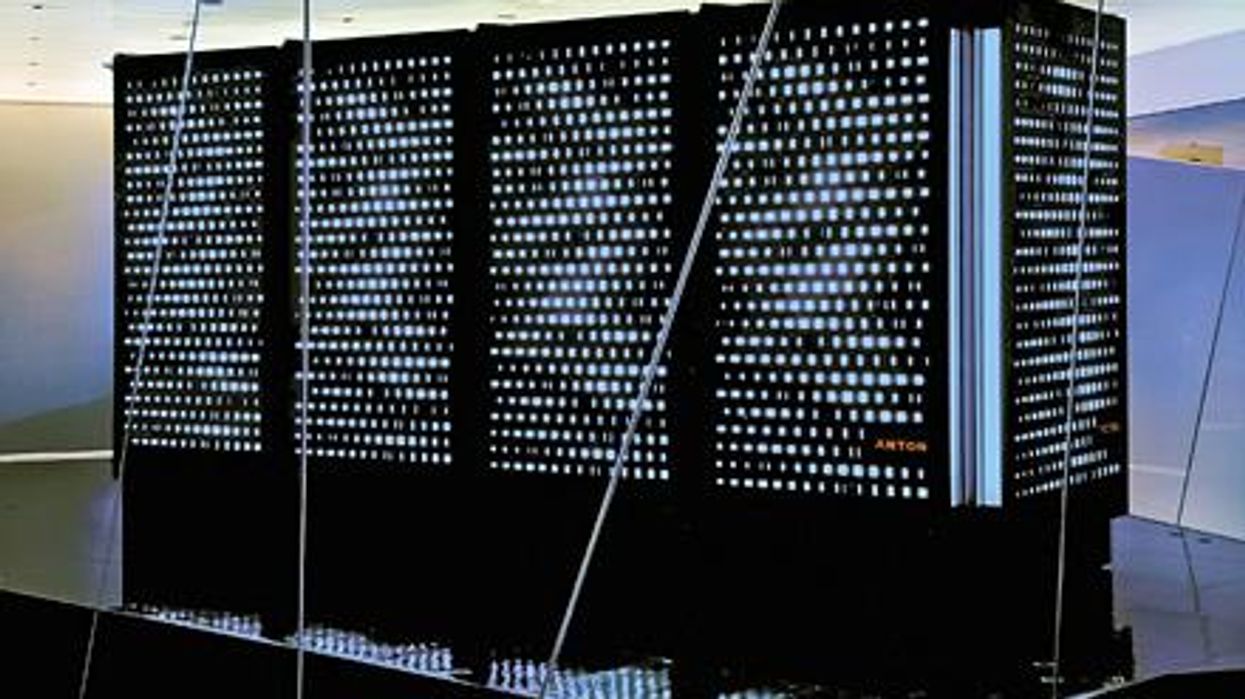
But none of it meant anything to me without actionable food advice, so I clicked through to the Recommendations page and found a list of My Superfoods (cranberry, garlic, kale, salmon, turmeric, watermelon, and bone broth) and My Foods to Avoid (chickpeas, kombucha, lentils, and rice noodles). There was also a searchable database of many foods that had been categorized for me, like "bell pepper; minimize" and "beef; enjoy."
"I just don't think sufficient data is yet available to make reliable personalized dietary recommendations based on one's microbiome."
Next, I looked at my results from DayTwo, which was founded in 2015 from research out of the Weizmann Institute of Science in Israel, and whose pitch to consumers is, "Blood sugar made easy. The algorithm diet personalized to you."
This app had some notable differences. There was no result about my metabolic fitness, microbial richness, or list of the species in my sample. There was also no list of superfoods or foods to avoid. Instead, the app encouraged me to build a meal by searching for foods in their database and combining them in beneficial ways for my blood sugar. Two slices of whole wheat bread received a score of 2.7 out of 10 ("Avoid"), but if combined with one cup of large curd cottage cheese, the score improved to 6.8 ("Limit"), and if I added two hard-boiled eggs, the score went up to 7.5 ("Good").
Perusing my list of foods with "Excellent" scores, I noticed some troubling conflicts with the other app. Lentils, which had been a no-no according to Viome, received high marks from DayTwo. Ditto for Kombucha. My purported superfood of cranberry received low marks. Almonds got an almost perfect score (9.7) while Viome told me to minimize them. I found similarly contradictory advice for foods I regularly eat, including navel oranges, peanuts, pork, and beets.
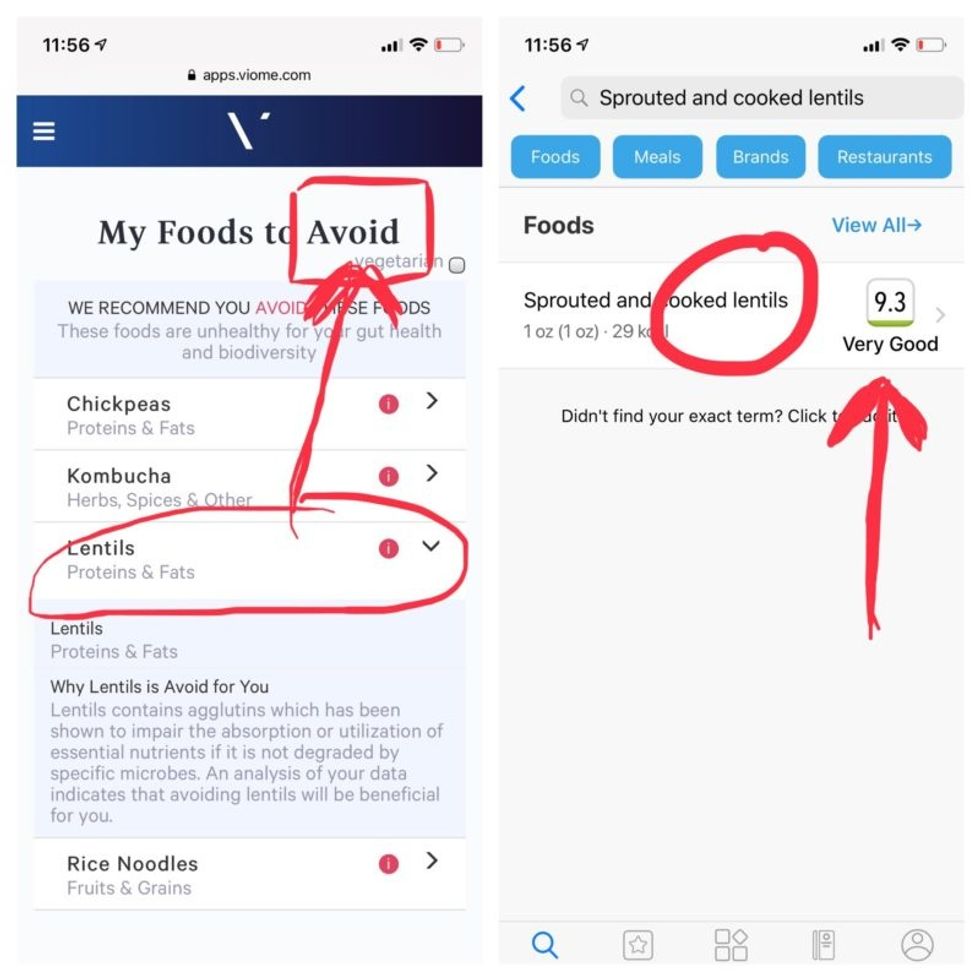
Contradictory dietary guidance that Kira Peikoff received from Viome (left) and DayTwo from an identical sample.
To be sure, there was some overlap. Both apps agreed on rice noodles (bad), chickpeas (bad), honey (bad), carrots (good), and avocado (good), among other foods.
But still, I was left scratching my head. Which set of recommendations should I trust, if either? And what did my results mean for the accuracy of this nascent field?
I called a couple of experts to find out.
"I have worked on the microbiome and nutrition for the last 20 years and I would be absolutely incapable of finding you evidence in the scientific literature that lentils have a detrimental effect based on the microbiome," said Dr. Jens Walter, an Associate Professor and chair for Nutrition, Microbes, and Gastrointestinal Health at the University of Alberta. "I just don't think sufficient data is yet available to make reliable personalized dietary recommendations based on one's microbiome. And even if they would have proprietary algorithms, at least one of them is not doing it right."
There is definite potential for personalized nutrition based on the microbiome, he said, but first, predictive models must be built and standardized, then linked to clinical endpoints, and tested in a large sample of healthy volunteers in order to enable extrapolations for the general population.
"It is mindboggling what you would need to do to make this work," he observed. "There are probably hundreds of relevant dietary compounds, then the microbiome has at least a hundred relevant species with a hundred or more relevant genes each, then you'd have to put all this together with relevant clinical outcomes. And there's a hundred-fold variation in that information between individuals."
However, Walter did acknowledge that the companies might be basing their algorithms on proprietary data that could potentially connect all the dots. I reached out to them to find out.
Amir Golan, the Chief Commercial Officer of DayTwo, told me, "It's important to emphasize this is a prediction, as the microbiome field is in a very early stage of research." But he added, "I believe we are the only company that has very solid science published in top journals and we can bring very actionable evidence and benefit to our uses."
He was referring to pioneering work out of the Weizmann Institute that was published in 2015 in the journal Cell, which logged the glycemic responses of 800 people in response to nearly 50,000 meals; adding information about the subjects' microbiomes enabled more accurate glycemic response predictions. Since then, Golan said, additional trials have been conducted, most recently with the Mayo Clinic, to duplicate the results, and other studies are ongoing whose results have not yet been published.
He also pointed out that the microbiome was merely one component that goes into building a client's profile, in addition to medical records, including blood glucose levels. (I provided my HbA1c levels, a measure of average blood sugar over the previous several months.)
"We are not saying we want to improve your gut microbiome. We provide a dynamic tool to help guide what you should eat to control your blood sugar and think about combinations," he said. "If you eat one thing, or with another, it will affect you in a different way."
Viome acknowledged that the two companies are taking very different approaches.
"DayTwo is primarily focused on the glycemic response," Naveen Jain, the CEO, told me. "If you can only eat butter for rest of your life, you will have no glycemic response but will probably die of a heart attack." He laughed. "Whereas we came from very different angle – what is happening inside the gut at a microbial level? When you eat food like spinach, how will that be metabolized in the gut? Will it produce the nutrients you need or cause inflammation?"
He said his team studied 1000 people who were on continuous glucose monitoring and fed them 45,000 meals, then built a proprietary data prediction model, looking at which microbes existed and how they actively broke down the food.
Jain pointed out that DayTwo sequences the DNA of the microbes, while Viome sequences the RNA – the active expression of DNA. That difference, in his opinion, is key to making accurate predictions.
"DNA is extremely stable, so when you eat any food and measure the DNA [in a fecal sample], you get all these false positives--you get DNA from plant food and meat, and you have no idea if those organisms are dead and simply transient, or actually exist. With RNA, you see what is actually alive in the gut."
More contradictory food advice from Viome (left) and DayTwo.
Note that controversy exists over how it is possible with a fecal sample to effectively measure RNA, which degrades within minutes, though Jain said that his company has the technology to keep RNA stable for fourteen days.
Viome's approach, Jain maintains, is 90 percent accurate, based on as-yet unpublished data; a patent was filed just last week. DayTwo's approach is 66 percent accurate according to the latest published research.
Natasha Haskey, a registered dietician and doctoral student conducting research in the field of microbiome science and nutrition, is skeptical of both companies. "We can make broad statements, like eat more fruits and vegetables and fiber, but when it comes to specific foods, the science is just not there yet," she said. "I think there is a future, and we will be doing that someday, but not yet. Maybe we will be closer in ten years."
Professor Walter wholeheartedly agrees with Haskey, and suggested that if people want to eat a gut-healthy diet, they should focus on beneficial oils, fruits and vegetables, fish, a variety of whole grains, poultry and beans, and limit red meat and cheese, as well as avoid processed meats.
"These services are far over the tips of their science skis," Arthur Caplan, the founding head of New York University's Division of Medical Ethics, said in an email. "We simply don't know enough about the gut microbiome, its fluctuations and variability from person to person to support general [direct-to-consumer] testing. This is simply premature. We need standards for accuracy, specificity, and sensitivity, plus mandatory competent counseling for all such testing. They don't exist. Neither should DTC testing—yet."
Meanwhile, it's time for lunch. I close out my Viome and DayTwo apps and head to the kitchen to prepare a peanut butter sandwich. My gut tells me I'll be just fine.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Working to Decipher the Puzzle of ‘Broken Heart Syndrome’
Elaine Kamil had just returned home after a few days of business meetings in 2013 when she started having chest pains. At first Kamil, then 66, wasn't worried—she had had some chest pain before and recently went to a cardiologist to do a stress test, which was normal.
"I can't be having a heart attack because I just got checked," she thought, attributing the discomfort to stress and high demands of her job. A pediatric nephrologist at Cedars-Sinai Hospital in Los Angeles, she takes care of critically ill children who are on dialysis or are kidney transplant patients. Supporting families through difficult times and answering calls at odd hours is part of her daily routine, and often leaves her exhausted.
She figured the pain would go away. But instead, it intensified that night. Kamil's husband drove her to the Cedars-Sinai hospital, where she was admitted to the coronary care unit. It turned out she wasn't having a heart attack after all. Instead, she was diagnosed with a much less common but nonetheless dangerous heart condition called takotsubo syndrome, or broken heart syndrome.
A heart attack happens when blood flow to the heart is obstructed—such as when an artery is blocked—causing heart muscle tissue to die. In takotsubo syndrome, the blood flow isn't blocked, but the heart doesn't pump it properly. The heart changes its shape and starts to resemble a Japanese fishing device called tako-tsubo, a clay pot with a wider body and narrower mouth, used to catch octopus.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks," explains Noel Bairey Merz, the cardiologist at Cedar Sinai who Kamil went to see after she was discharged.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks."
But even though the heart isn't permanently damaged, mortality rates due to takotsubo syndrome are comparable to those of a heart attack, Merz notes—about 4-5 percent of patients die from the attack, and 20 percent within the next five years. "It's as bad as a heart attack," Merz says—only it's much less known, even to doctors. The condition affects only about 1 percent of people, and there are around 15,000 new cases annually. It's diagnosed using a cardiac ventriculogram, an imaging test that allows doctors to see how the heart pumps blood.
Scientists don't fully understand what causes Takotsubo syndrome, but it usually occurs after extreme emotional or physical stress. Doctors think it's triggered by a so-called catecholamine storm, a phenomenon in which the body releases too much catecholamines—hormones involved in the fight-or-flight response. Evolutionarily, when early humans lived in savannas or forests and had to either fight off predators or flee from them, these hormones gave our ancestors the needed strength and stamina to take either action. Released by nerve endings and by the adrenal glands that sit on top of the kidneys, these hormones still flood our bodies in moments of stress, but an overabundance of them could sometimes be damaging.

Elaine Kamil
A study by scientists at Harvard Medical School linked increased risk of takotsubo to higher activity in the amygdala, a brain region responsible for emotions that's involved in responses to stress. The scientists believe that chronic stress makes people more susceptible to the syndrome. Notably, one small study suggested that the number of Takotsubo cases increased during the COVID-19 pandemic.
There are no specific drugs to treat takotsubo, so doctors rely on supportive therapies, which include medications typically used for high blood pressure and heart failure. In most cases, the heart returns to its normal shape within a few weeks. "It's a spontaneous recovery—the catecholamine storm is resolved, the injury trigger is removed and the heart heals itself because our bodies have an amazing healing capacity," Merz says. It also helps that tissues remain intact. 'The heart cells don't die, they just aren't functioning properly for some time."
That's the good news. The bad news is that takotsubo is likely to strike again—in 5-20 percent of patients the condition comes back, sometimes more severe than before.
That's exactly what happened to Kamil. After getting her diagnosis in 2013, she realized that she actually had a previous takotsubo episode. In 2010, she experienced similar symptoms after her son died. "The night after he died, I was having severe chest pain at night, but I was too overwhelmed with grief to do anything about it," she recalls. After a while, the pain subsided and didn't return until three years later.
For weeks after her second attack, she felt exhausted, listless and anxious. "You lose confidence in your body," she says. "You have these little twinges on your chest, or if you start having arrhythmia, and you wonder if this is another episode coming up. It's really unnerving because you don't know how to read these cues." And that's very typical, Merz says. Even when the heart muscle appears to recover, patients don't return to normal right away. They have shortens of breath, they can't exercise, and they stay anxious and worried for a while.
Women over the age of 50 are diagnosed with takotsubo more often than other demographics. However, it happens in men too, although it typically strikes after physical stress, such as a triathlon or an exhausting day of cycling. Young people can also get takotsubo. Older patients are hospitalized more often, but younger people tend to have more severe complications. It could be because an older person may go for a jog while younger one may run a marathon, which would take a stronger toll on the body of a person who's predisposed to the condition.
Notably, the emotional stressors don't always have to be negative—the heart muscle can get out of shape from good emotions, too. "There have been case reports of takotsubo at weddings," Merz says. Moreover, one out of three or four takotsubo patients experience no apparent stress, she adds. "So it could be that it's not so much the catecholamine storm itself, but the body's reaction to it—the physiological reaction deeply embedded into out physiology," she explains.
Merz and her team are working to understand what makes people predisposed to takotsubo. They think a person's genetics play a role, but they haven't yet pinpointed genes that seem to be responsible. Genes code for proteins, which affect how the body metabolizes various compounds, which, in turn, affect the body's response to stress. Pinning down the protein involved in takotsubo susceptibility would allow doctors to develop screening tests and identify those prone to severe repeating attacks. It will also help develop medications that can either prevent it or treat it better than just waiting for the body to heal itself.
Researchers at the Imperial College London found that elevated levels of certain types of microRNAs—molecules involved in protein production—increase the chances of developing takotsubo.
In one study, researchers tried treating takotsubo in mice with a drug called suberanilohydroxamic acid, or SAHA, typically used for cancer treatment. The drug improved cardiac health and reversed the broken heart in rodents. It remains to be seen if the drug would have a similar effect on humans. But identifying a drug that shows promise is progress, Merz says. "I'm glad that there's research in this area."
This article was originally published by Leaps.org on July 28, 2021.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
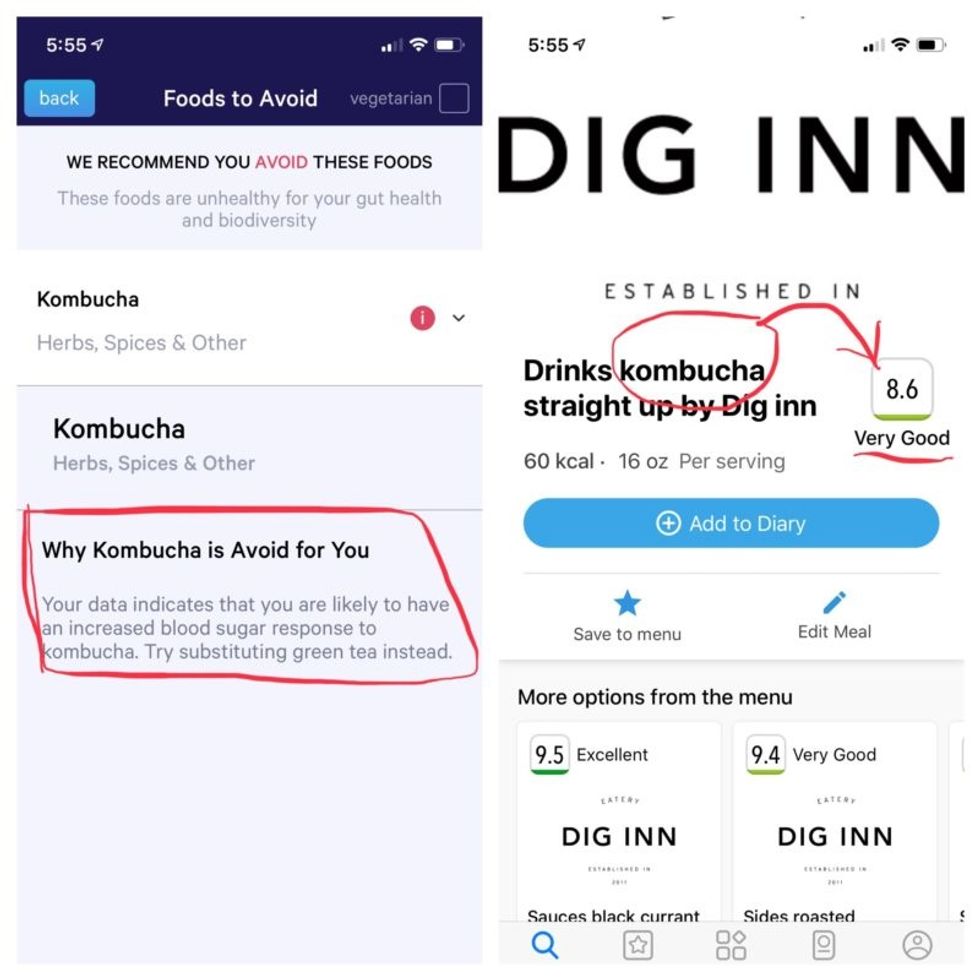
Did Anton the AI find a new treatment for a deadly cancer?
Researchers used a supercomputer to learn about the subtle movement of a cancer-causing molecule, and then they found the precise drug that can recognize that motion.
Bile duct cancer is a rare and aggressive form of cancer that is often difficult to diagnose. Patients with advanced forms of the disease have an average life expectancy of less than two years.
Many patients who get cancer in their bile ducts – the tubes that carry digestive fluid from the liver to the small intestine – have mutations in the protein FGFR2, which leads cells to grow uncontrollably. One treatment option is chemotherapy, but it’s toxic to both cancer cells and healthy cells, failing to distinguish between the two. Increasingly, cancer researchers are focusing on biomarker directed therapy, or making drugs that target a particular molecule that causes the disease – FGFR2, in the case of bile duct cancer.
A problem is that in targeting FGFR2, these drugs inadvertently inhibit the FGFR1 protein, which looks almost identical. This causes elevated phosphate levels, which is a sign of kidney damage, so doses are often limited to prevent complications.
In recent years, though, a company called Relay has taken a unique approach to picking out FGFR2, using a powerful supercomputer to simulate how proteins move and change shape. The team, leveraging this AI capability, discovered that FGFR2 and FGFR1 move differently, which enabled them to create a more precise drug.
Preliminary studies have shown robust activity of this drug, called RLY-4008, in FGFR2 altered tumors, especially in bile duct cancer. The drug did not inhibit FGFR1 or cause significant side effects. “RLY-4008 is a prime example of a precision oncology therapeutic with its highly selective and potent targeting of FGFR2 genetic alterations and resistance mutations,” says Lipika Goyal, assistant professor of medicine at Harvard Medical School. She is a principal investigator of Relay’s phase 1-2 clinical trial.
Boosts from AI and a billionaire
Traditional drug design has been very much a case of trial and error, as scientists investigate many molecules to see which ones bind to the intended target and bind less to other targets.
“It’s being done almost blindly, without really being guided by structure, so it fails very often,” says Olivier Elemento, associate director of the Institute for Computational Biomedicine at Cornell. “The issue is that they are not sampling enough molecules to cover some of the chemical space that would be specific to the target of interest and not specific to others.”
Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
Some scientists have tried to use X-rays of crystallized proteins to look at the structure of proteins and design better drugs. But they have failed to account for an important factor: proteins are moving and constantly folding into different shapes.
David Shaw, a hedge fund billionaire, wanted to help improve drug discovery and understood that a key obstacle was that computer models of molecular dynamics were limited; they simulated motion for less than 10 millionths of a second.
In 2001, Shaw set up his own research facility, D.E. Shaw Research, to create a supercomputer that would be specifically designed to simulate protein motion. Seven years later, he succeeded in firing up a supercomputer that can now conduct high speed simulations roughly 100 times faster than others. Called Anton, it has special computer chips to enable this speed, and its software is powered by AI to conduct many simulations.
After creating the supercomputer, Shaw teamed up with leading scientists who were interested in molecular motion, and they founded Relay Therapeutics.
Elemento believes that Relay’s approach is highly beneficial in designing a better drug for bile duct cancer. “Relay Therapeutics has a cutting-edge approach for molecular dynamics that I don’t believe any other companies have, at least not as advanced.” Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
How it works
Relay used both experimental and computational approaches to design RLY-4008. The team started out by taking X-rays of crystallized versions of both their intended target, FGFR2, and the almost identical FGFR1. This enabled them to get a 3D snapshot of each of their structures. They then fed the X-rays into the Anton supercomputer to simulate how the proteins were likely to move.
Anton’s simulations showed that the FGFR1 protein had a flap that moved more frequently than FGFR2. Based on this distinct motion, the team tried to design a compound that would recognize this flap shifting around and bind to FGFR2 while steering away from its more active lookalike.
For that, they went back Anton, using the supercomputer to simulate the behavior of thousands of potential molecules for over a year, looking at what made a particular molecule selective to the target versus another molecule that wasn’t. These insights led them to determine the best compounds to make and test in the lab and, ultimately, they found that RLY-4008 was the most effective.
Promising results so far
Relay began phase 1-2 trials in 2020 and will continue until 2024. Preliminary results showed that, in the 17 patients taking a 70 mg dose of RLY-4008, the drug worked to shrink tumors in 88 percent of patients. This was a significant increase compared to other FGFR inhibitors. For instance, Futibatinib, which recently got FDA approval, had a response rate of only 42 percent.
Across all dose levels, RLY-4008 shrank tumors by 63 percent in 38 patients. In more good news, the drug didn’t elevate their phosphate levels, which suggests that it could be taken without increasing patients’ risk for kidney disease.
“Objectively, this is pretty remarkable,” says Elemento. “In a small patient study, you have a molecule that is able to shrink tumors in such a high fraction of patients. It is unusual to see such good results in a phase 1-2 trial.”
A simulated future
The research team is continuing to use molecular dynamic simulations to develop other new drug, such as one that is being studied in patients with solid tumors and breast cancer.
As for their bile duct cancer drug, RLY-4008, Relay plans by 2024 to have tested it in around 440 patients. “The mature results of the phase 1-2 trial are highly anticipated,” says Goyal, the principal investigator of the trial.
Sameek Roychowdhury, an oncologist and associate professor of internal medicine at Ohio State University, highlights the need for caution. “This has early signs of benefit, but we will look forward to seeing longer term results for benefit and side effect profiles. We need to think a few more steps ahead - these treatments are like the ’Whack-a-Mole game’ where cancer finds a way to become resistant to each subsequent drug.”
“I think the issue is going to be how durable are the responses to the drug and what are the mechanisms of resistance,” says Raymond Wadlow, an oncologist at the Inova Medical Group who specializes in gastrointestinal and haematological cancer. “But the results look promising. It is a much more selective inhibitor of the FGFR protein and less toxic. It’s been an exciting development.”