Study Shows “Living Drug” Can Provide a Lasting Cure for Cancer

A recent study by researchers at the University of Pennsylvania examined how CAR-T therapy helped Doug Olson beat a cancer death sentence for over a decade - and how it could work for more people.
Doug Olson was 49 when he was diagnosed with chronic lymphocytic leukemia, a blood cancer that strikes 21,000 Americans annually. Although the disease kills most patients within a decade, Olson’s case progressed more slowly, and courses of mild chemotherapy kept him healthy for 13 years. Then, when he was 62, the medication stopped working. The cancer had mutated, his doctor explained, becoming resistant to standard remedies. Harsher forms of chemo might buy him a few months, but their side effects would be debilitating. It was time to consider the treatment of last resort: a bone-marrow transplant.
Olson, a scientist who developed blood-testing instruments, knew the odds. There was only a 50 percent chance that a transplant would cure him. There was a 20 percent chance that the agonizing procedure—which involves destroying the patient’s marrow with chemo and radiation, then infusing his blood with donated stem cells—would kill him. If he survived, he would face the danger of graft-versus-host disease, in which the donor’s cells attack the recipient’s tissues. To prevent it, he would have to take immunosuppressant drugs, increasing the risk of infections. He could end up with pneumonia if one of his three grandchildren caught a sniffle. “I was being pushed into a corner,” Olson recalls, “with very little room to move.”
Soon afterward, however, his doctor revealed a possible escape route. He and some colleagues at the University of Pennsylvania’s Abramson Cancer Center were starting a clinical trial, he said, and Olson—still mostly symptom-free—might be a good candidate. The experimental treatment, known as CAR-T therapy, would use genetic engineering to turn his T lymphocytes (immune cells that guard against viruses and other pathogens) into a weapon against cancer.
In September 2010, technicians took some of Olson’s T cells to a laboratory, where they were programmed with new molecular marching orders and coaxed to multiply into an army of millions. When they were ready, a nurse inserted a catheter into his neck. At the turn of a valve, his soldiers returned home, ready to do battle.
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
Three weeks later, Olson was slammed with a 102-degree fever, nausea, and chills. The treatment had triggered two dangerous complications: cytokine release syndrome, in which immune chemicals inflame the patient’s tissues, and tumor lysis syndrome, in which toxins from dying cancer cells overwhelm the kidneys. But the crisis passed quickly, and the CAR-T cells fought on. A month after the infusion, the doctor delivered astounding news: “We can’t find any cancer in your body.”
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
An Unexpected Cure
In February 2022, the same cancer researchers reported a remarkable milestone: the trial’s first two patients had survived for more than a decade. Although Olson’s predecessor—a retired corrections officer named Bill Ludwig—died of COVID-19 complications in early 2021, both men had remained cancer-free. And the modified immune cells continued to patrol their territory, ready to kill suspected tumor cells the moment they arose.
“We can now conclude that CAR-T cells can actually cure patients with leukemia,” University of Pennsylvania immunologist Carl June, who spearheaded the development of the technique, told reporters. “We thought the cells would be gone in a month or two. The fact that they’ve survived 10 years is a major surprise.”
Even before the announcement, it was clear that CAR-T therapy could win a lasting reprieve for many patients with cancers that were once a death sentence. Since the Food and Drug Administration approved June’s version (marketed as Kymriah) in 2017, the agency has greenlighted five more such treatments for various types of leukemia, lymphoma, and myeloma. “Every single day, I take care of patients who would previously have been told they had no options,” says Rayne Rouce, a pediatric hematologist/oncologist at Texas Children’s Cancer Center. “Now we not only have a treatment option for those patients, but one that could potentially be the last therapy for their cancer that they’ll ever have to receive.”

Immunologist Carl June, middle, spearheaded development of the CAR-T therapy that gave patients Bill Ludwig, left, and Doug Olson, right, a lengthy reprieve on their terminal cancer diagnoses.
Penn Medicine
Yet the CAR-T approach doesn’t help everyone. So far, it has only shown success for blood cancers—and for those, the overall remission rate is 30 to 40 percent. “When it works, it works extraordinarily well,” says Olson’s former doctor, David Porter, director of Penn’s blood and bone marrow transplant program. “It’s important to know why it works, but it’s equally important to know why it doesn’t—and how we can fix that.”
The team’s study, published in the journal Nature, offers a wealth of data on what worked for these two patients. It may also hold clues for how to make the therapy effective for more people.
Building a Better T Cell
Carl June didn’t set out to cure cancer, but his serendipitous career path—and a personal tragedy—helped him achieve insights that had eluded other researchers. In 1971, hoping to avoid combat in Vietnam, he applied to the U.S. Naval Academy in Annapolis, Maryland. June showed a knack for biology, so the Navy sent him on to Baylor College of Medicine. He fell in love with immunology during a fellowship researching malaria vaccines in Switzerland. Later, the Navy deployed him to the Fred Hutchinson Cancer Research Center in Seattle to study bone marrow transplantation.
There, June became part of the first research team to learn how to culture T cells efficiently in a lab. After moving on to the National Naval Medical Center in the ’80s, he used that knowledge to combat the newly emerging AIDS epidemic. HIV, the virus that causes the disease, invades T cells and eventually destroys them. June and his post-doc Bruce Levine developed a method to restore patients’ depleted cell populations, using tiny magnetic beads to deliver growth-stimulating proteins. Infused into the body, the new T cells effectively boosted immune function.
In 1999, after leaving the Navy, June joined the University of Pennsylvania. His wife, who’d been diagnosed with ovarian cancer, died two years later, leaving three young children. “I had not known what it was like to be on the other side of the bed,” he recalls. Watching her suffer through grueling but futile chemotherapy, followed by an unsuccessful bone-marrow transplant, he resolved to focus on finding better cancer treatments. He started with leukemia—a family of diseases in which mutant white blood cells proliferate in the marrow.
Cancer is highly skilled at slipping through the immune system’s defenses. T cells, for example, detect pathogens by latching onto them with receptors designed to recognize foreign proteins. Leukemia cells evade detection, in part, by masquerading as normal white blood cells—that is, as part of the immune system itself.
June planned to use a viral vector no one had tried before: HIV.
To June, chimeric antigen receptor (CAR) T cells looked like a promising tool for unmasking and destroying the impostors. Developed in the early ’90s, these cells could be programmed to identify a target protein, and to kill any pathogen that displayed it. To do the programming, you spliced together snippets of DNA and inserted them into a disabled virus. Next, you removed some of the patient’s T cells and infected them with the virus, which genetically hijacked its new hosts—instructing them to find and slay the patient’s particular type of cancer cells. When the T cells multiplied, their descendants carried the new genetic code. You then infused those modified cells into the patient, where they went to war against their designated enemy.
Or that’s what happened in theory. Many scientists had tried to develop therapies using CAR-T cells, but none had succeeded. Although the technique worked in lab animals, the cells either died out or lost their potency in humans.
But June had the advantage of his years nurturing T cells for AIDS patients, as well as the technology he’d developed with Levine (who’d followed him to Penn with other team members). He also planned to use a viral vector no one had tried before: HIV, which had evolved to thrive in human T cells and could be altered to avoid causing disease. By the summer of 2010, he was ready to test CAR-T therapy against chronic lymphocytic leukemia (CLL), the most common form of the disease in adults.
Three patients signed up for the trial, including Doug Olson and Bill Ludwig. A portion of each man’s T cells were reprogrammed to detect a protein found only on B lymphocytes, the type of white blood cells affected by CLL. Their genetic instructions ordered them to destroy any cell carrying the protein, known as CD19, and to multiply whenever they encountered one. This meant the patients would forfeit all their B cells, not just cancerous ones—but regular injections of gamma globulins (a cocktail of antibodies) would make up for the loss.
After being infused with the CAR-T cells, all three men suffered high fevers and potentially life-threatening inflammation, but all pulled through without lasting damage. The third patient experienced a partial remission and survived for eight months. Olson and Ludwig were cured.
Learning What Works
Since those first infusions, researchers have developed reliable ways to prevent or treat the side effects of CAR-T therapy, greatly reducing its risks. They’ve also been experimenting with combination therapies—pairing CAR-T with chemo, cancer vaccines, and immunotherapy drugs called checkpoint inhibitors—to improve its success rate. But CAR-T cells are still ineffective for at least 60 percent of blood cancer patients. And they remain in the experimental stage for solid tumors (including pancreatic cancer, mesothelioma, and glioblastoma), whose greater complexity make them harder to attack.
The new Nature study offers clues that could fuel further advances. The Penn team “profiled these cells at a level where we can almost say, ‘These are the characteristics that a T cell would need to survive 10 years,’” says Rouce, the physician at Texas Children’s Cancer Center.
One surprising finding involves how CAR-T cells change in the body over time. At first, those that Olson and Ludwig received showed the hallmarks of “killer” T-cells (also known as CD8 cells)—highly active lymphocytes bent on exterminating every tumor cell in sight. After several months, however, the population shifted toward “helper” T-cells (or CD4s), which aid in forming long-term immune memory but are normally incapable of direct aggression. Over the years, the numbers swung back and forth, until only helper cells remained. Those cells showed markers suggesting they were too exhausted to function—but in the lab, they were able not only to recognize but to destroy cancer cells.
June and his team suspect that those tired-looking helper cells had enough oomph to kill off any B cells Olson and Ludwig made, keeping the pair’s cancers permanently at bay. If so, that could prompt new approaches to selecting cells for CAR-T therapy. Maybe starting with a mix of cell types—not only CD8s, but CD4s and other varieties—would work better than using CD8s alone. Or perhaps inducing changes in cell populations at different times would help.
Another potential avenue for improvement is starting with healthier cells. Evidence from this and other trials hints that patients whose T cells are more robust to begin with respond better when their cells are used in CAR-T therapy. The Penn team recently completed a clinical trial in which CLL patients were treated with ibrutinib—a drug that enhances T-cell function—before their CAR-T cells were manufactured. The response rate, says David Porter, was “very high,” with most patients remaining cancer-free a year after being infused with the souped-up cells.
Such approaches, he adds, are essential to achieving the next phase in CAR-T therapy: “Getting it to work not just in more people, but in everybody.”

Doug Olson enjoys nature - and having a future.
Penn Medicine
To grasp what that could mean, it helps to talk with Doug Olson, who’s now 75. In the years since his infusion, he has watched his four children forge careers, and his grandkids reach their teens. He has built a business and enjoyed the rewards of semi-retirement. He’s done volunteer and advocacy work for cancer patients, run half-marathons, sailed the Caribbean, and ridden his bike along the sun-dappled roads of Silicon Valley, his current home.
And in his spare moments, he has just sat there feeling grateful. “You don’t really appreciate the effect of having a lethal disease until it’s not there anymore,” he says. “The world looks different when you have a future.”
This article was first published on Leaps.org on March 24, 2022.
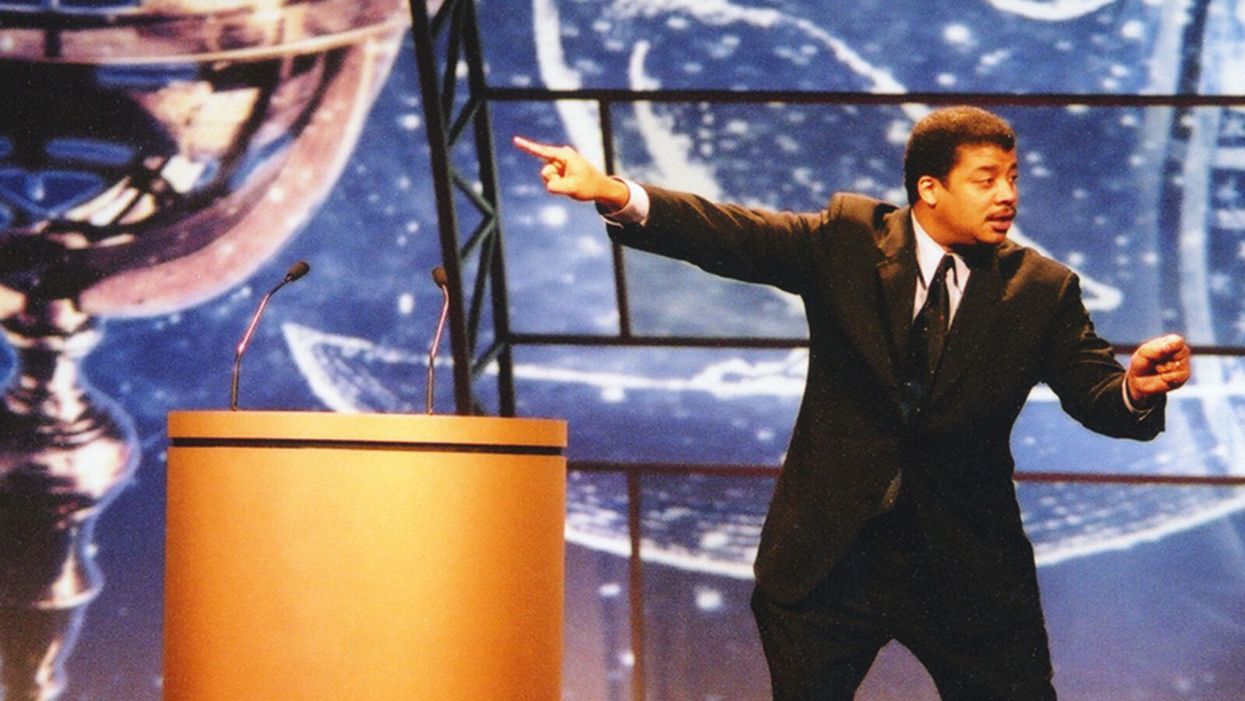
Neil deGrasse Tyson Wants Celebrities to Promote Scientists
Neil de Grasse Tyson wants fellow celebrities to point their followers to experts and organizations who know what they're talking about.
"President Kennedy was the first president to not wear a hat. Have you seen men wearing hats since then?" Neil deGrasse Tyson, one of the world's few astrophysicists with a household name, asks on the phone from his car. Well, no. "If I wear some cowboy hats, it's because it's the outfit, it's not because that's my standard equipment when I leave the home."
"We have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
But Tyson, who speaks in methodically reasoned paragraphs with lots of semi-rhetorical questions to make sure we're all still listening, isn't really making a point about Mad Men-era men's clothing trends. "Should a president influence fashion?" he says. "I think people sometimes don't know the full power they have over other people. So, that's the first prong in this comment. My second prong is, why would anyone take medical advice from a politician?"
Days before our conversation, news broke that President Trump said he was taking hydroxychloroquine, which he had hyped for months as a surefire magical cure for COVID-19 — the science just hadn't caught up to his predictions. But the science never did catch up; instead, it went the opposite direction, showing that hydroxychloroquine, when used to treat COVID-19 patients, actually led to an increased risk of death.
Alarm spread swiftly around the globe as experts cast the president's professed self-medicating as illogical and dangerous. However, it was just one of a series of wild pieces of medical advice espoused by Trump from his mighty pulpit, like that, hey, maybe disinfectants could cure people when injected into their bodies. (That also leads to death.)
But people do take medical advice from politicians. An Arizona man afraid of COVID-19 died after consuming chloroquine phosphate, which he and his wife had sitting on the back of a shelf after using it to treat koi fish for parasites. The pandemic has exposed many weaknesses in the feedback loop of society, government, the media, and science, including the difficulty of seeding accurate medical information with the masses. Many on the left and right decry a broken political and news media system, but Tyson believes the problem isn't mega-influencers like Trump. Rather it's the general public's desire to take their advice on complex topics – like the science of virology – that such influencers know nothing about.
Tyson's not upset with the public, who follow Trump's advice. "As an educator, I can't get angry with you," he says. Or even Trump himself. "Trump was elected by 60 million people, right? So, you could say all you want about Trump, kick him out of office, whatever. [There's] still the 60 million fellow Americans who walk among us who voted for him. So, what are you going to do with them?"
Tyson also isn't upset with Facebook, Twitter, and other social platforms that serve as today's biggest conduits for misinformation. After all, in the realm of modern media's history, these networks are tadpoles. "As an educator and as a scientist, I'm leaning towards, let's figure out a way to train people in school to not fall victim to false information, and how to judge what is likely to be false relative to what is likely to be true. And that's hard, but you and I have never had a class in that, have we? We've had biology classes, we've had English lit, we've had classes on Shakespeare — we have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
This is why Tyson himself doesn't engage in Trump bashing on his social feeds, but does try to get people to differentiate factual science from fake news. "I feel responsibility to participate in the enlightenment of culture and of civilization, because I have that access," says Tyson, who has 13.9M followers on Twitter, 1.2M on Instagram, and 4.2M on Facebook. He doesn't tell his followers not to inject themselves with Clorox ("no one likes being told what to do"), but tries to get them to visualize a pandemic's impact by comparing it to, say, a throng of rabbits.
"Left unchecked, 1,000 rabbits in 5 years, become 7-billion, the human population of the World. After 15 years, a 'land-ocean' of rabbits fills to one-kilometer depth across all of Earth's continents. Viruses can reproduce waaaay faster than Rabbits," he tweeted on April 6, after much of the nation had locked down to slow the pandemic's spread. For added viral impact, he attached a photo of an adorable, perhaps appropriately scared-looking, white bunny.
Of course, not all celebrities message responsibly.
Tyson is a rare scientist-turned-celebrity. His appeal isn't acting in movies or singing dance-pop anthems (if only). Rather, his life's work is making science fun and interesting to as many people as possible through his best-selling books on astrophysics and his directorship of the planetarium at the American Museum of Natural History in New York. His longstanding place in popular culture is an exception, not the rule.
And he believes his fellow celebrities, actors and pop music stars and internet influencers, should aid the public's quest for accurate scientific information. And in order to do that, they must point their followers to experts and organizations who know what they're talking about. "It could be to a website, it could be to a talk that was given. I would say that that's where the responsibility lies if you control the interests of a million people," he says.
One example of this is Lady Gaga's March 14 Instagram of herself on her couch with her three dogs with the caption, "So I talked to some doctors and scientists. It's not the easiest for everyone right now but the kindest/healthiest thing we can do is self-quarantine and not hang out with people over 65 and in large groups. I wish I could see my parents and grandmas right now but it's much safer to not so I don't get them sick in case I have it. I'm hanging at home with my dogs." (All the celebrities here in this article are my references, not Tyson's, who does not call out specific people.)
Of course, not all celebrities message responsibly. Jessica Biel and Jenny McCarthy have faced scorn for public stances against vaccines. Gwyneth Paltrow and her media brand GOOP have faced backlash for promoting homeopathic treatments with no basis in science.
"The New Age Movement is a cultural idea, it has nothing to do with religion, has nothing to do with politics, and it's people who were rejecting objectively established science in part or in total because they have a belief system that they want to attach to it, okay? This is how you get the homeopathic remedies," says Tyson. "That's why science exists, so that we don't have to base decisions on belief systems."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Masks and Distancing Won't Be Enough to Prevent School Outbreaks, Latest Science Suggests
The likely dominant mode of aerosol transmission cannot be ignored in school settings.
Never has the prospect of "back to school" seemed so ominous as it does in 2020. As the number of COVID-19 cases climb steadily in nearly every state, the prospect of in-person classes are filling students, parents, and faculty alike with a corresponding sense of dread.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue.
The decision to resume classes at primary, secondary, and collegiate levels is not one that should be regarded lightly, particularly as coronavirus cases skyrocket across the United States.
What should be a measured, data-driven discussion that weighs risks and benefits has been derailed by political talking points. President Trump has been steadily advocating for an unfettered return to the classroom, often through imperative "OPEN THE SCHOOLS!!!" tweets. In July, Secretary of Education Betsy DeVos threatened to withhold funding from schools that did not reopen for full-time, in-person classes, despite not having the authority to do so. Like so many public health issues, opening schools in the midst of a generational pandemic has been politicized to the point that the question of whether it is safe to do so has been obscured and confounded. However, this question still deserves to be examined based on evidence.
What We Know About Kids and COVID-19
Some arguments for returning to in-person education have focused on the fact that children and young adults are less susceptible to severe disease. In some cases, people have stated that children cannot be infected, pointing to countries that have resumed in-person education with no associated outbreaks. However, those countries had extremely low community transmission and robust testing and surveillance.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue: children can be infected, they can become sick, and, in rare cases, they can die. Children can also transmit the virus to others, especially if they are in prolonged proximity to them. A Georgia sleepaway camp was the site of at least 260 cases among mostly children and teenagers, some as young as 6 years old. Children have been shown to shed infectious virus in their nasal secretions and have viral loads comparable to adults. Children can unquestionably be infected with SARS-CoV-2 and spread it to others.
The more data emerges, the more it appears that both primary and secondary schools and universities alike are conducive environments for super-spreading. Mitigating these risks depends heavily on individual schools' ability to enforce reduction measures. So far, the evidence demonstrates that in most cases, schools are unable to adequately protect students or staff. A school superintendent from a small district in Arizona recently described an outbreak that occurred among staff prior to in-person classes resuming. Schools that have opened so far have almost immediately reported new clusters of cases among students or staff.
This is because it is impossible to completely eliminate risk even with the most thoughtful mitigation measures when community transmission is high. Risk can be reduced, but the greater the likelihood that someone will be exposed in the community, the greater the risk they might pass the virus to others on campus or in the classroom.
There are still many unknowns about SARS-CoV-2 transmission, but some environments are known risks for virus transmission: enclosed spaces with crowds of people in close proximity over extended durations. Transmission is thought to occur predominantly through inhaled aerosols or droplets containing SARS-CoV-2, which are produced through common school activities such as breathing, speaking, or singing. Masks reduce but do not eliminate the production of these aerosols. Implementing universal mask-wearing and physical distancing guidelines will furthermore be extraordinarily challenging for very young children.
Smaller particle aerosols can remain suspended in the air and accumulate over time. In an enclosed space where people are gathering, such as a classroom, this renders risk mitigation measures such as physical distancing and masks ineffective. Many classrooms at all levels of education are not conducive to improving ventilation through low-cost measures such as opening windows, much less installing costly air filtration systems.
As a risk reduction measure, ventilation greatly depends on factors like window placement, window type, room size, room occupancy, building HVAC systems, and overall airflow. There isn't much hard data on the specific effects of ventilation on virus transmission, and the models that support ventilation rely on assumptions based on scant experimental evidence that doesn't account for virologic parameters.
There is also no data about how effective air filtration or UV systems would be for SARS-CoV-2 transmission risk reduction, so it's hard to say if this would result in a meaningful risk reduction or not. We don't have enough data outside of a hospital setting to support that ventilation and/or filtration would significantly reduce risk, and it's impractical (and most likely impossible in most schools) to implement hospital ventilation systems, which would likely require massive remodeling of existing HVAC infrastructure. In a close contact situation, the risk reduction might be minimal anyway since it's difficult to avoid exposure to respiratory aerosols and droplets a person is exhaling.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity.
Efforts to resume in-person education depend heavily on school health and safety plans, which often rely on self-reporting of symptoms due to insufficient testing capacity. Self-reporting is notoriously unreliable, and furthermore, SARS-CoV-2 can be readily transmitted by pre-symptomatic individuals who may be unaware that they are sick, making testing an essential component of any such plan. Primary and secondary schools are faced with limited access to testing and no funds to support it. Even in institutions that include a testing component in their reopening plans, this is still too infrequent to support the full student body returning to campus.
Economic Conflicts of Interest
Rebecca Harrison, a PhD candidate at Cornell University serving on the campus reopening committee, is concerned that her institution's plan places too much faith in testing capacity and is over-reliant on untested models. Harrison says that, as a result, students are being implicitly encouraged to return to campus and "very little has been done to actively encourage students who are safe and able to stay home, to actually stay home."
Harrison also is concerned that her institution "presumably hopes to draw students back from the safety of their parents' basements to (re)join the residential campus experience ... and drive revenue." This is a legitimate concern. Some schools may be actively thwarting safety plans in place to protect students based on financial incentives. Student athletes at Colorado State have alleged that football coaches told them not to report COVID-19 symptoms and are manipulating contact tracing reports.
Public primary and secondary schools are not dependent on student athletics for revenue, but nonetheless are susceptible to state and federal policies that tie reopening to budgets. If schools are forced to make decisions based on a balance sheet, rather than the health and safety of students, teachers, and staff, they will implement health and safety plans that are inadequate. Schools will become ground zero for new clusters of cases.
Looking Ahead: When Will Schools Be Able to Open Again?
One crucial measure is the percent positivity rate in the local community, the number of positive tests based on all the tests that are done. Some states, like California, have implemented policies guiding the reopening of schools that depend in part on a local community's percent positivity rate falling under 8 percent, among other benchmarks including the rate of new daily cases. Currently, statewide, test positivity is below 7%, with an average of 3 new daily cases per 1000 people per day. However, the California department of health acknowledges that new cases per day are underreported. There are 6.3 million students in the California public school system, suggesting that at any given time, there could be nearly 20,000 students who might be contagious, without accounting for presymptomatic teachers and staff. In the classroom environment, just one of those positive cases could spread the virus to many people in one day despite masks, distancing, and ventilation.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity. Only with rapid identification and isolation of new cases, followed by contact tracing and quarantine, can we break chains of transmission and prevent further spread in the school and the larger community.
None of these safety concerns diminish the many harms associated with the sudden and haphazard way remote learning has been implemented. Online education has not been effective in many cases and is difficult to implement equitably. Young children, in particular, are deprived of the essential social and intellectual development they would normally get in a classroom with teachers and their peers. Parents of young children are equally unprepared and unable to provide full-time instruction. Our federal leadership's catastrophic failure to contain the pandemic like other countries has put us in this terrible position, where we must choose between learning or spreading a deadly pathogen.
Blame aside, parents, educators, and administrators must decide whether to resume in-person classes this fall. Those decisions should be based on evidence, not on politics or economics. The data clearly shows that community transmission is out of control throughout most of the country. Thus, we ignore the risk of school outbreaks at our peril.
[Editor's Note: Here's the other essay in the Back to School series: 5 Key Questions to Consider Before Sending Your Child Back to School.]