Researchers Get Closer to Gene Editing Treatment for Cardiovascular Disease

Scientists are making progress to create a one-time therapy that would permanently lower LDL cholesterol to prevent heart attacks caused by high LDL.
Later this year, Verve Therapeutics of Cambridge, Ma., will initiate Phase 1 clinical trials to test VERVE-101, a new medication that, if successful, will employ gene editing to significantly reduce low-density lipoprotein cholesterol, or LDL.
LDL is sometimes referred to as the “bad” cholesterol because it collects in the walls of blood vessels, and high levels can increase chances of a heart attack, cardiovascular disease or stroke. There are approximately 600,000 heart attacks per year due to blood cholesterol damage in the United States, and heart disease is the number one cause of death in the world. According to the CDC, a 10 percent decrease in total blood cholesterol levels can reduce the incidence of heart disease by as much as 30 percent.
Verve’s Founder and CEO, Sekar Kathiresan, spent two decades studying the genetic basis for heart attacks while serving as a professor of medicine at Harvard Medical School. His research led to two critical insights.
“One is that there are some people that are naturally resistant to heart attack and have lifelong, low levels of LDL,” the cardiologist says. “Second, there are some genes that can be switched off that lead to very low LDL cholesterol, and individuals with those genes switched off are resistant to heart attacks.”
Kathiresan and his team formed a hypothesis in 2016 that if they could develop a medicine that mimics the natural protection that some people enjoy, then they might identify a powerful new way to treat and ultimately prevent heart attacks. They launched Verve in 2018 with the goal of creating a one-time therapy that would permanently lower LDL and eliminate heart attacks caused by high LDL.
"Imagine a future where somebody gets a one-time treatment at the time of their heart attack or before as a preventive measure," says Kathiresan.
The medication is targeted specifically for patients who have a genetic form of high cholesterol known as heterozygous familial hypercholesterolemia, or FH, caused by expression of a gene called PCSK9. Verve also plans to develop a program to silence a gene called ANGPTL3 for patients with FH and possibly those with or at risk of atherosclerotic cardiovascular disease.
FH causes cholesterol to be high from birth, reaching levels of 200 to 300 milligrams per deciliter. Suggested normal levels are around 100 to 129 mg/dl, and anything above 130 mg/dl is considered high. Patients with cardiovascular disease usually are asked to aim for under 70 mg/dl, but many still have unacceptably high LDL despite taking oral medications such as statins. They are more likely to have heart attacks in their 30s, 40s and 50s, and require lifelong LDL control.
The goal for drug treatments for high LDL, Kathiresan says, is to reduce LDL as low as possible for as long as possible. Physicians and researchers also know that a sizeable portion of these patients eventually start to lose their commitment to taking their statins and other LDL-controlling medications regularly.
“If you ask 100 patients one year after their heart attack what fraction are still taking their cholesterol-lowering medications, it’s less than half,” says Kathiresan. “So imagine a future where somebody gets a one-time treatment at the time of their heart attack or before as a preventive measure. It’s right in front of us, and it’s something that Verve is looking to do.”
In late 2020, Verve completed primate testing with monkeys that had genetically high cholesterol, using a one-time intravenous injection of VERVE-101. It reduced the monkeys’ LDL by 60 percent and, 18 months later, remains at that level. Kathiresan expects the LDL to stay low for the rest of their lives.
Verve’s gene editing medication is packaged in a lipid nanoparticle to serve as the delivery mechanism into the liver when infused intravenously. The drug is absorbed and makes its way into the nucleus of the liver cells.
Verve’s program targeting PCSK9 uses precise, single base, pair base editing, Kathiresan says, meaning it doesn't cut DNA like CRISPR gene editing systems do. Instead, it changes one base, or letter, in the genome to a different one without affecting the letters around it. Comparing it to a pencil and eraser, he explains that the medication erases out a letter A and makes it a letter G in the A, C, G and T code in DNA.
“We need to continue to advance our approach and tools to make sure that we have the absolute maximum ability to detect off-target effects,” says Euan Ashley, professor of medicine and genetics at Stanford University.
By making that simple change from A to G, the medication switches off the PCSK9 gene, automatically lowering LDL cholesterol.
“Once the DNA change is made, all the cells in the liver will have that single A to G change made,” Kathiresan says. “Then the liver cells divide and give rise to future liver cells, but every time the cell divides that change, the new G is carried forward.”
Additionally, Verve is pursuing its second gene editing program to eliminate ANGPTL3, a gene that raises both LDL and blood triglycerides. In 2010, Kathiresan's research team learned that people who had that gene completely switched off had LDL and triglyceride levels of about 20 and were very healthy with no heart attacks. The goal of Verve’s medication will be to switch off that gene, too, as an option for additional LDL or triglyceride lowering.
“Success with our first drug, VERVE-101, will give us more confidence to move forward with our second drug,” Kathiresan says. “And it opens up this general idea of making [genomic] spelling changes in the liver to treat other diseases.”
The approach is less ethically concerning than other gene editing technologies because it applies somatic editing that affects only the individual patient, whereas germline editing in the patient’s sperm or egg, or in an embryo, gets passed on to children. Additionally, gene editing therapies receive the same comprehensive amount of testing for side effects as any other medicine.
“We need to continue to advance our approach and tools to make sure that we have the absolute maximum ability to detect off-target effects,” says Euan Ashley, professor of medicine and genetics at Stanford University and founding director of its Center for Inherited Cardiovascular Disease. Ashley and his colleagues at Stanford’s Clinical Genomics Program and beyond are increasingly excited about the promise of gene editing.
“We can offer precision diagnostics, so increasingly we’re able to define the disease at a much deeper level using molecular tools and sequencing,” he continues. “We also have this immense power of reading the genome, but we’re really on the verge of taking advantage of the power that we now have to potentially correct some of the variants that we find on a genome that contribute to disease.”
He adds that while the gene editing medicines in development to correct genomes are ahead of the delivery mechanisms needed to get them into the body, particularly the heart and brain, he’s optimistic that those aren’t too far behind.
“It will probably take a few more years before those next generation tools start to get into clinical trials,” says Ashley, whose book, The Genome Odyssey, was published last year. “The medications might be the sexier part of the research, but if you can’t get it into the right place at the right time in the right dose and not get it to the places you don’t want it to go, then that tool is not of much use.”
Medical experts consider knocking out the PCSK9 gene in patients with the fairly common genetic disorder of familial hypercholesterolemia – roughly one in 250 people – a potentially safe approach to gene editing and an effective means of significantly lowering their LDL cholesterol.

Nurse Erin McGlennon has an Implantable Cardioverter Defibrillator and takes medications, but she is also hopeful that a gene editing medication will be developed in the near future.
Erin McGlennon
Mary McGowan, MD, chief medical officer for The Family Heart Foundation in Pasadena, CA, sees the tremendous potential for VERVE-101 and believes patients should be encouraged by the fact that this kind of research is occurring and how much Verve has accomplished in a relatively short time. However, she offers one caveat, since even a 60 percent reduction in LDL won’t completely eliminate the need to reduce the remaining amount of LDL.
“This technology is very exciting,” she said, “but we want to stress to our patients with familial hypercholesterolemia that we know from our published research that most people require several therapies to get their LDL down., whether that be in primary prevention less than 100 mg/dl or secondary prevention less than 70 mg/dl, So Verve’s medication would be an add-on therapy for most patients.”
Dr. Kathiresan concurs: “We expect our medicine to lower LDL cholesterol by about 60 percent and that our patients will be on background oral medications, including statins that lower LDL cholesterol.”
Several leading research centers are investigating gene editing treatments for other types of cardiovascular diseases. Elizabeth McNally, Elizabeth Ward Professor and Director at the Center for Genetic Medicine at Northwestern University’s Feinberg School of Medicine, pursues advanced genetic correction in neuromuscular diseases such as Duchenne muscular dystrophy and spinal muscular atrophy. A cardiologist, she and her colleagues know these diseases frequently have cardiac complications.
“Even though the field is driven by neuromuscular specialists, it’s the first therapies in patients with neuromuscular diseases that are also expected to make genetic corrections in the heart,” she says. “It’s almost like an afterthought that we’re potentially fixing the heart, too.”
Another limitation McGowan sees is that too many healthcare providers are not yet familiar with how to test patients to determine whether or not they carry genetic mutations that need to be corrected. “We need to get more genetic testing done,” she says. “For example, that’s the case with hypertrophic cardiomyopathy, where a lot of the people who probably carry that diagnosis and have never been genetically identified at a time when genetic testing has never been easier.”
One patient who has been diagnosed with hypertrophic cardiomyopathy also happens to be a nurse working in research at Genentech Pharmaceutical, now a member of the Roche Group, in South San Francisco. To treat the disease, Erin McGlennon, RN, has an Implantable Cardioverter Defibrillator and takes medications, but she is also hopeful that a gene editing medication will be developed in the near future.
“With my condition, the septum muscles are just growing thicker, so I’m on medicine to keep my heart from having dangerous rhythms,” says McGlennon of the disease that carries a low risk of sudden cardiac death. “So, the possibility of having a treatment option that can significantly improve my day-to-day functioning would be a major breakthrough.”
McGlennon has some control over cardiovascular destiny through at least one currently available technology: in vitro fertilization. She’s going through it to ensure that her children won't express the gene for hypertrophic cardiomyopathy.
Researchers are looking to engineer chocolate with less oil, which could reduce some of its detriments to health.
Creamy milk with velvety texture. Dark with sprinkles of sea salt. Crunchy hazelnut-studded chunks. Chocolate is a treat that appeals to billions of people worldwide, no matter the age. And it’s not only the taste, but the feel of a chocolate morsel slowly melting in our mouths—the smoothness and slipperiness—that’s part of the overwhelming satisfaction. Why is it so enjoyable?
That’s what an interdisciplinary research team of chocolate lovers from the University of Leeds School of Food Science and Nutrition and School of Mechanical Engineering in the U.K. resolved to study in 2021. They wanted to know, “What is making chocolate that desirable?” says Siavash Soltanahmadi, one of the lead authors of a new study about chocolates hedonistic quality.
Besides addressing the researchers’ general curiosity, their answers might help chocolate manufacturers make the delicacy even more enjoyable and potentially healthier. After all, chocolate is a billion-dollar industry. Revenue from chocolate sales, whether milk or dark, is forecasted to grow 13 percent by 2027 in the U.K. In the U.S., chocolate and candy sales increased by 11 percent from 2020 to 2021, on track to reach $44.9 billion by 2026. Figuring out how chocolate affects the human palate could up the ante even more.
Building a 3D tongue
The team began by building a 3D tongue to analyze the physical process by which chocolate breaks down inside the mouth.
As part of the effort, reported earlier this year in the scientific journal ACS Applied Materials and Interfaces, the team studied a large variety of human tongues with the intention to build an “average” 3D model, says Soltanahmadi, a lubrication scientist. When it comes to edible substances, lubrication science looks at how food feels in the mouth and can help design foods that taste better and have more satisfying texture or health benefits.
There are variations in how people enjoy chocolate; some chew it while others “lick it” inside their mouths.
Tongue impressions from human participants studied using optical imaging helped the team build a tongue with key characteristics. “Our tongue is not a smooth muscle, it’s got some texture, it has got some roughness,” Soltanahmadi says. From those images, the team came up with a digital design of an average tongue and, using 3D printed molds, built a “mimic tongue.” They also added elastomers—such as silicone or polyurethane—to mimic the roughness, the texture and the mechanical properties of a real tongue. “Wettability" was another key component of the 3D tongue, Soltanahmadi says, referring to whether a surface mixes with water (hydrophilic) or, in the case of oil, resists it (hydrophobic).
Notably, the resulting artificial 3D-tongues looked nothing like the human version, but they were good mimics. The scientists also created “testing kits” that produced data on various physical parameters. One such parameter was viscosity, the measure of how gooey a food or liquid is — honey is more viscous compared to water, for example. Another was tribology, which defines how slippery something is — high fat yogurt is more slippery than low fat yogurt; milk can be more slippery than water. The researchers then mixed chocolate with artificial saliva and spread it on the 3D tongue to measure the tribology and the viscosity. From there they were able to study what happens inside the mouth when we eat chocolate.
The team focused on the stages of lubrication and the location of the fat in the chocolate, a process that has rarely been researched.
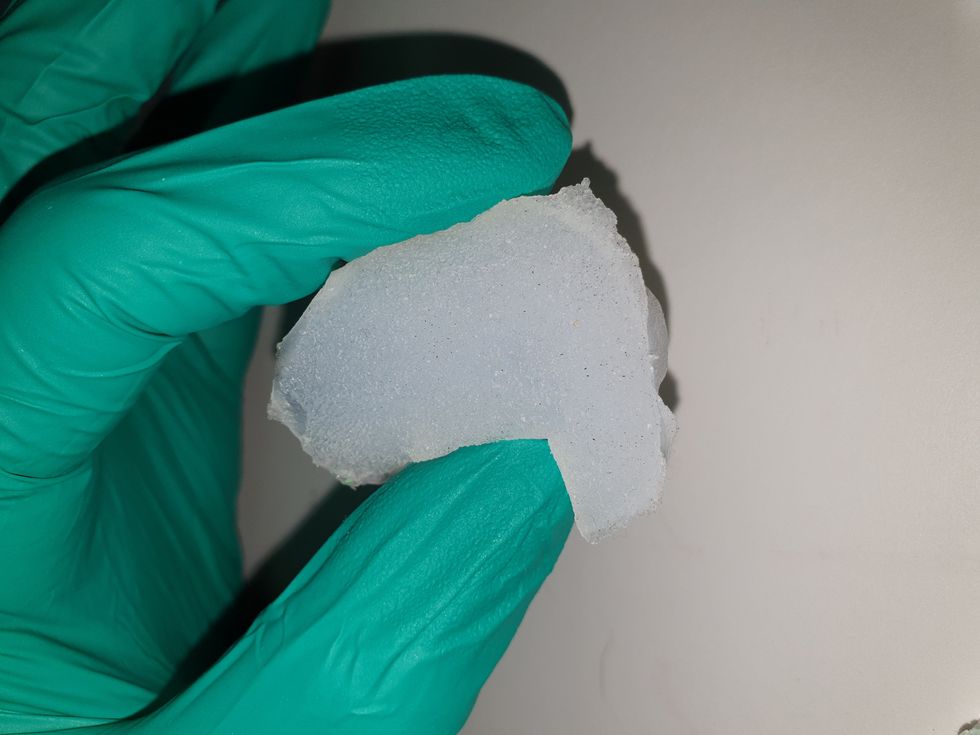
The artificial 3D-tongues look nothing like human tongues, but they function well enough to do the job.
Courtesy Anwesha Sarkar and University of Leeds
The oral processing of chocolate
We process food in our mouths in several stages, Soltanahmadi says. And there is variation in these stages depending on the type of food. So, the oral processing of a piece of meat would be different from, say, the processing of jelly or popcorn.
There are variations with chocolate, in particular; some people chew it while others use their tongues to explore it (within their mouths), Soltanahmadi explains. “Usually, from a consumer perspective, what we find is that if you have a luxury kind of a chocolate, then people tend to start with licking the chocolate rather than chewing it.” The researchers used a luxury brand of dark chocolate and focused on the process of licking rather than chewing.
As solid cocoa particles and fat are released, the emulsion envelops the tongue and coats the palette creating a smooth feeling of chocolate all over the mouth. That tactile sensation is part of the chocolate’s hedonistic appeal we crave.
Understanding the make-up of the chocolate was also an important step in the study. “Chocolate is a composite material. So, it has cocoa butter, which is oil, it has some particles in it, which is cocoa solid, and it has sugars," Soltanahmadi says. "Dark chocolate has less oil, for example, and less sugar in it, most of the time."
The researchers determined that the oral processing of chocolate begins as soon as it enters a person’s mouth; it starts melting upon exposure to one’s body temperature, even before the tongue starts moving, Soltanahmadi says. Then, lubrication begins. “[Saliva] mixes with the oily chocolate and it makes an emulsion." An emulsion is a fluid with a watery (or aqueous) phase and an oily phase. As chocolate breaks down in the mouth, that solid piece turns into a smooth emulsion with a fatty film. “The oil from the chocolate becomes droplets in a continuous aqueous phase,” says Soltanahmadi. In other words, as solid cocoa particles and fat are released, the emulsion envelops the tongue and coats the palette, creating a smooth feeling of chocolate all over the mouth. That tactile sensation is part of the chocolate’s hedonistic appeal we crave, says Soltanahmadi.
Finding the sweet spot
After determining how chocolate is orally processed, the research team wanted to find the exact sweet spot of the breakdown of solid cocoa particles and fat as they are released into the mouth. They determined that the epicurean pleasure comes only from the chocolate's outer layer of fat; the secondary fatty layers inside the chocolate don’t add to the sensation. It was this final discovery that helped the team determine that it might be possible to produce healthier chocolate that would contain less oil, says Soltanahmadi. And therefore, less fat.
Rongjia Tao, a physicist at Temple University in Philadelphia, thinks the Leeds study and the concept behind it is “very interesting.” Tao, himself, did a study in 2016 and found he could reduce fat in milk chocolate by 20 percent. He believes that the Leeds researchers’ discovery about the first layer of fat being more important for taste than the other layer can inform future chocolate manufacturing. “As a scientist I consider this significant and an important starting point,” he says.
Chocolate is rich in polyphenols, naturally occurring compounds also found in fruits and vegetables, such as grapes, apples and berries. Research found that plant polyphenols can protect against cancer, diabetes and osteoporosis as well as cardiovascular ad neurodegenerative diseases.
Not everyone thinks it’s a good idea, such as chef Michael Antonorsi, founder and owner of Chuao Chocolatier, one of the leading chocolate makers in the U.S. First, he says, “cacao fat is definitely a good fat.” Second, he’s not thrilled that science is trying to interfere with nature. “Every time we've tried to intervene and change nature, we get things out of balance,” says Antonorsi. “There’s a reason cacao is botanically known as food of the gods. The botanical name is the Theobroma cacao: Theobroma in ancient Greek, Theo is God and Brahma is food. So it's a food of the gods,” Antonorsi explains. He’s doubtful that a chocolate made only with a top layer of fat will produce the same epicurean satisfaction. “You're not going to achieve the same sensation because that surface fat is going to dissipate and there is no fat from behind coming to take over,” he says.
Without layers of fat, Antonorsi fears the deeply satisfying experiential part of savoring chocolate will be lost. The University of Leeds team, however, thinks that it may be possible to make chocolate healthier - when consumed in limited amounts - without sacrificing its taste. They believe the concept of less fatty but no less slick chocolate will resonate with at least some chocolate-makers and consumers, too.
Chocolate already contains some healthful compounds. Its cocoa particles have “loads of health benefits,” says Soltanahmadi. Dark chocolate usually has more cocoa than milk chocolate. Some experts recommend that dark chocolate should contain at least 70 percent cocoa in order for it to offer some health benefit. Research has shown that the cocoa in chocolate is rich in polyphenols, naturally occurring compounds also found in fruits and vegetables, such as grapes, apples and berries. Research has shown that consuming plant polyphenols can be protective against cancer, diabetes and osteoporosis as well as cardiovascular and neurodegenerative diseases.
“So keeping the healthy part of it and reducing the oily part of it, which is not healthy, but is giving you that indulgence of it … that was the final aim,” Soltanahmadi says. He adds that the team has been approached by individuals in the chocolate industry about their research. “Everyone wants to have a healthy chocolate, which at the same time tastes brilliant and gives you that self-indulging experience.”
Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
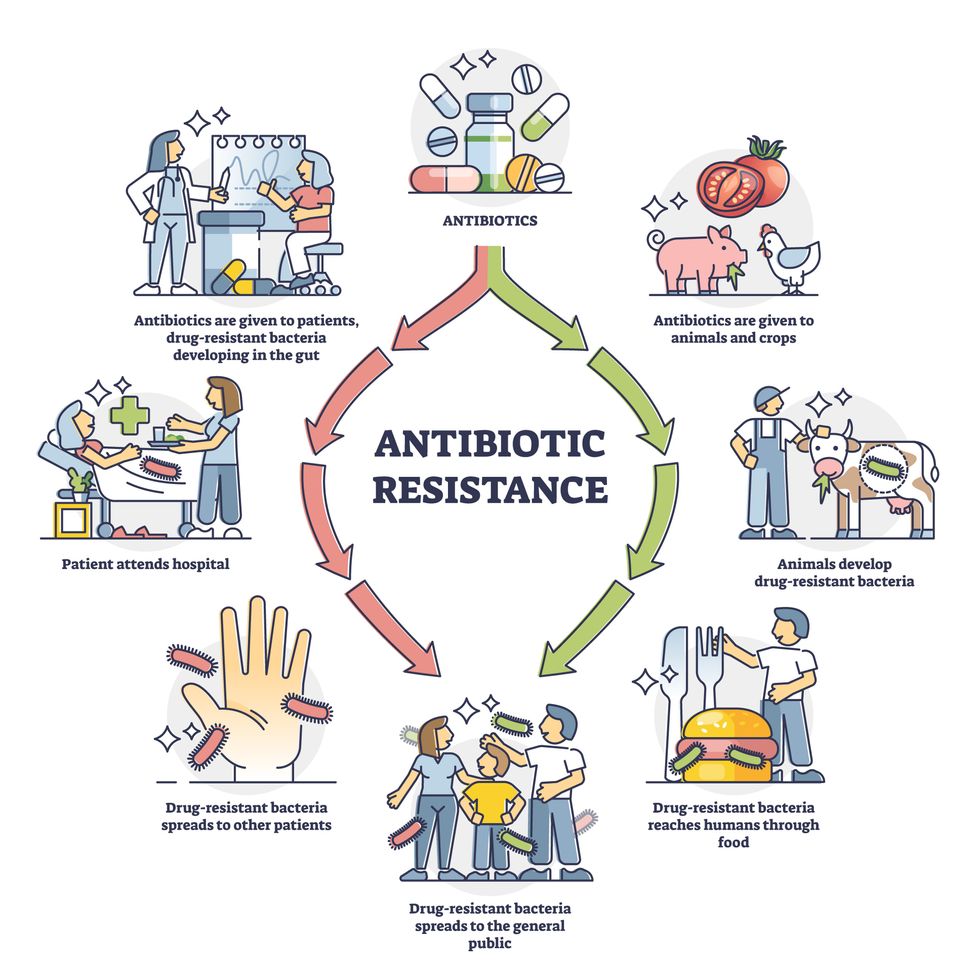
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”