An Investigational Drug Offers Hope to Patients with a Disabling Neuromuscular Disease

Robert Thomas was a devoted runner, gym goer, and crew member on a sailing team in San Diego when, in his 40s, he noticed that his range of movement was becoming more limited.
He thought he was just getting older, but when he was hiking an uphill trail in Lake Tahoe, he kept tripping over rocks. "I'd never had this happen before," Robert says. "I knew something was wrong but didn't know what it was."
It wasn't until age 50 when he was diagnosed with Charcot-Marie-Tooth disease. The genetic disorder damages the peripheral nerves, which connect the brain and spinal cord to the rest of the body. This network of nerves is responsible for relaying information and signals about sensation, movement, and motor coordination. Over time, the disease causes debilitating muscle weakness and the loss of limb control.
Charcot-Marie-Tooth usually presents itself in childhood or in a person's teens, but in some patients, like Robert, onset can be later in life. Symptoms may include muscle cramping, tingling, or burning. Many patients also have high foot arches or hammer toes — toes that curl from the middle joint instead of pointing forward. Those affected often have difficulty walking and may lose sensation in their lower legs, feet, hands, or forearms. One of the most common rare diseases, it affects around 130,000 people in the United States and 2.8 million worldwide.
Like many people with Charcot-Marie-Tooth, or CMT, Robert wears corrective braces on his legs to help with walking. Now 61, he can't run or sail anymore because of the disease, but he still works out regularly and can hike occasionally. CMT also affects his grip, so he has to use special straps while doing some exercises.
For the past few years, Robert has been participating in a clinical trial for an investigational CMT drug. He takes the liquid formulation every morning and evening using an oral syringe. Scientists are following patients like Robert to learn if their symptoms stabilize or improve while on the drug. Dubbed PXT300, the drug was designed by French biopharmaceutical company Pharnext and is the farthest along in development for CMT. If approved, it would be the first drug for the disease.
Currently, there's no cure for CMT, only supportive treatments like pain medication. Some individuals receive physical and occupational therapy. A drug for CMT could be a game-changer for patients whose quality of life is severely affected by the disease.
Genetic Underpinnings
CMT arises from mutations in genes that are responsible for creating and maintaining the myelin sheath — the insulating layer around nerves. Pharnext's drug is meant to treat patients with CMT1A, the most common form of the disease, which represents about half of CMT cases. Around 5% of those with CMT1A become severely disabled and end up in wheelchairs. People with CMT1A have an extra copy of the gene PMP22, which makes a protein that's needed to maintain the myelin sheath around peripheral nerves.
Typically, an individual inherits one copy of PMP22 from each parent. But a person with CMT1A receives a copy of PMP22 from one parent and two copies from a parent with the disease. This extra copy of the gene results in excess protein production, which damages the cells responsible for preserving and regenerating the myelin sheath, called Schwann cells.
The myelin sheath helps ensure that a signal from the brain gets carried to nerves in the muscles so that a part of the body can carry out a particular action or movement. This sheath is like the insulation on an electrical cord and the action is like a light bulb. If the insulation is fine, the light bulb turns on. But if the insulation is frayed, the light will flicker.
"The same happens to these patients," says David Horn Solomon, CEO of Pharnext. "The signal to their muscle is weak and flickers." Over time, their muscles become weaker and thinner.
The PMP22 gene has proven difficult to target with a drug because it's located in a protected space — the Schwann cells that make up the insulation around nerves. "There's not an easy way to tamp it down," Solomon says.
Another company, Acceleron Pharma of Cambridge, Massachusetts, was developing an injectable CMT drug meant to increase the strength of leg muscles. But the company halted development last year after the experimental drug failed in a mid-stage trial. While the drug led to a statistically significant increase in muscle volume, it didn't translate to improvements in muscle function or quality of life for trial participants.
Made by Design
Pharnext's drug, PXT3003, is a combination of three existing drugs — baclofen, a muscle relaxant; naltrexone, a drug that decreases the desire for alcohol and opioids; and sorbitol, a type of sugar alcohol.
The company designed the drug using its artificial intelligence platform, which screened 20,000 existing drugs to predict combinations that could inhibit the PMP22 gene and thereby lower protein production. The AI system narrowed the search to several hundreds of combinations and Pharnext tested around 75 of them in the lab before landing on baclofen, naltrexone, and sorbitol. Individually, the drugs don't have much effect on the PMP22 gene. But combined, they work to lower how much protein the gene makes.
"How the drug inside the cell reduces expression isn't quite clear yet," says Florian Thomas, director of the Hereditary Neuropathy Center, and founding chair and professor in the department of neurology at Hackensack University Medical Center and Hackensack Meridian School of Medicine in New Jersey (no relation to Robert Thomas, the CMT patient). "By reducing the amount of protein being produced, we hopefully can stabilize the nerves."
In rodents genetically engineered to have the PMP22 gene, the drug reduced protein levels and delayed onset of muscle weakness when given to rats. In another animal study, the drug increased the size of the myelin sheath around nerves in rats.
"Like humans with CMT, one of the problems the animals have is they can't grip things, their grip strength is poor," Solomon says. But when treated with Pharnext's drug, "the grip strength of these animals improves dramatically even over 12 weeks."
Human trials look encouraging, too. But the company ran into a manufacturing issue during a late-stage trial. The drug requires refrigeration, and as a result of temperature changes, crystals formed inside vials containing the high dose of the drug. The study was a double-blind trial, meaning neither the trial participants nor investigators were supposed to know who received the high dose of the drug, who received the low dose, and who received a placebo. In these types of studies, the placebo and experimental drug should look the same so that investigators can't tell them apart. But because only the high dose contained crystals, not the low dose or placebo, regulators said the trial data could be biased.
Pharnext is now conducting a new randomized, double-blind trial to prove that its drug works. The study is recruiting individuals aged 16 through 65 years old with mild to moderate CMT. The company hopes to show that the drug can stop patients' symptoms from worsening, or in the best case scenario, possibly even improve them. The company doesn't think the drug will be able to help people with severe forms of the disease.
"In neurologic disease, you're looking for plasticity, where there's still the possibility of stabilization or reversal," Solomon says. Plasticity refers to the ability of the nervous system to change and adapt in response to stimuli.
Preventing Disability
Allison Moore, a CMT patient and founder and CEO of the Hereditary Neuropathy Foundation, has been following drug development for CMT since she founded the organization in 2001. She says many investigational drugs haven't moved forward because they've shown little success in animals. The fact that Pharnext's drug has made it to a late-stage human trial is promising, she says.
"It's really exciting," Moore says. "There's a chance that if you take the drug early before you're very severe, you'll end up not developing the disease to a level that's super disabling."
CMT has damaged Moore's peroneal nerve, a main nerve in the foot. As a result, she has foot drop, the inability to lift the front part of her foot, and needs to wear leg braces to help her walk. "The idea that you could take this early on and that it could stop progression, that's the hope that we have."
Thomas, the neurologist, says a drug doesn't have to be a cure to have a significant impact on patients. "If I have a CMT patient who's 50 years old, that patient will be more disabled by age 60," he says. "If I can treat that person with a drug, and that person is just as disabled at age 60 as they were at age 50, that's transformative in my mind."
While Robert Thomas says he hasn't noticed a dramatic improvement since he's been on the drug, he does think it's helping. Robert is now in an open-label study, which means he and his health provider are aware that he's receiving the drug.
When the COVID-19 pandemic hit, manufacturing and supply chain disruptions meant that Robert was without the trial drug for two months. When his medication ran out, his legs felt unstable again and walking was harder. "There was a clear distinction between being on and off that medication," he says.
Pharnext's current trial will take about a year and a half to complete. After that, the FDA will decide on whether to approve the drug for CMT patients.
As scientists learn more about the PMP22 gene and the more than 100 other genes that when mutated cause CMT, more precise treatments could be possible. For instance, scientists have used the gene-editing tool CRISPR to correct a CMT-causing mutation in human cells in the lab. The results were published August 16 in the journal Frontiers in Cell and Developmental Biology.
Pharnext is also interested in pursuing genetic treatments for CMT, but in the meantime, repurposed drugs may be the best shot at helping patients until more advanced treatments are available.
The Friday Five: How to exercise for cancer prevention
How to exercise for cancer prevention. Plus, a device that brings relief to back pain, ingredients for reducing Alzheimer's risk, the world's oldest disease could make you young again, and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- How to exercise for cancer prevention
- A device that brings relief to back pain
- Ingredients for reducing Alzheimer's risk
- Is the world's oldest disease the fountain of youth?
- Scared of crossing bridges? Your phone can help
New approach to brain health is sparking memories
This fall, Robert Reinhart of Boston University published a study finding that electrical stimulation can boost memory - and Reinhart was surprised to discover the effects lasted a full month.
What if a few painless electrical zaps to your brain could help you recall names, perform better on Wordle or even ward off dementia?
This is where neuroscientists are going in efforts to stave off age-related memory loss as well as Alzheimer’s disease. Medications have shown limited effectiveness in reversing or managing loss of brain function so far. But new studies suggest that firing up an aging neural network with electrical or magnetic current might keep brains spry as we age.
Welcome to non-invasive brain stimulation (NIBS). No surgery or anesthesia is required. One day, a jolt in the morning with your own battery-operated kit could replace your wake-up coffee.
Scientists believe brain circuits tend to uncouple as we age. Since brain neurons communicate by exchanging electrical impulses with each other, the breakdown of these links and associations could be what causes the “senior moment”—when you can’t remember the name of the movie you just watched.
In 2019, Boston University researchers led by Robert Reinhart, director of the Cognitive and Clinical Neuroscience Laboratory, showed that memory loss in healthy older adults is likely caused by these disconnected brain networks. When Reinhart and his team stimulated two key areas of the brain with mild electrical current, they were able to bring the brains of older adult subjects back into sync — enough so that their ability to remember small differences between two images matched that of much younger subjects for at least 50 minutes after the testing stopped.
Reinhart wowed the neuroscience community once again this fall. His newer study in Nature Neuroscience presented 150 healthy participants, ages 65 to 88, who were able to recall more words on a given list after 20 minutes of low-intensity electrical stimulation sessions over four consecutive days. This amounted to a 50 to 65 percent boost in their recall.
Even Reinhart was surprised to discover the enhanced performance of his subjects lasted a full month when they were tested again later. Those who benefited most were the participants who were the most forgetful at the start.

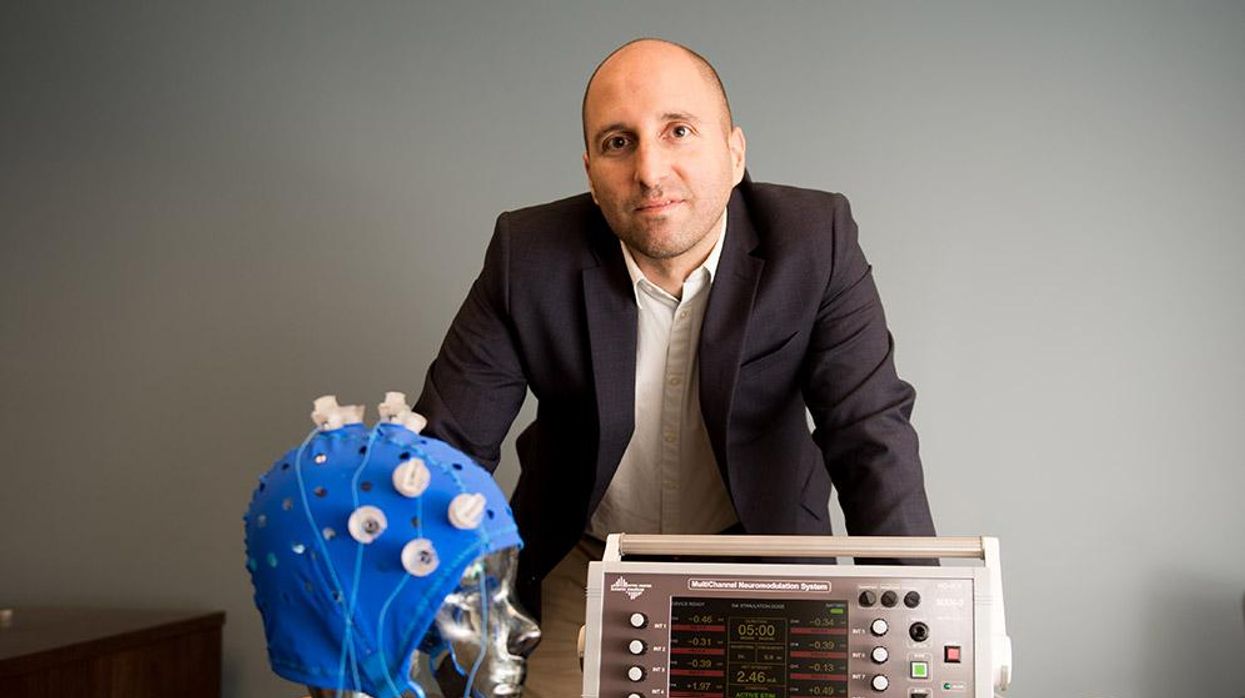
An older person participates in Robert Reinhart's research on brain stimulation.
Robert Reinhart
Reinhart’s subjects only suffered normal age-related memory deficits, but NIBS has great potential to help people with cognitive impairment and dementia, too, says Krista Lanctôt, the Bernick Chair of Geriatric Psychopharmacology at Sunnybrook Health Sciences Center in Toronto. Plus, “it is remarkably safe,” she says.
Lanctôt was the senior author on a meta-analysis of brain stimulation studies published last year on people with mild cognitive impairment or later stages of Alzheimer’s disease. The review concluded that magnetic stimulation to the brain significantly improved the research participants’ neuropsychiatric symptoms, such as apathy and depression. The stimulation also enhanced global cognition, which includes memory, attention, executive function and more.
This is the frontier of neuroscience.
The two main forms of NIBS – and many questions surrounding them
There are two types of NIBS. They differ based on whether electrical or magnetic stimulation is used to create the electric field, the type of device that delivers the electrical current and the strength of the current.
Transcranial Current Brain Stimulation (tES) is an umbrella term for a group of techniques using low-wattage electrical currents to manipulate activity in the brain. The current is delivered to the scalp or forehead via electrodes attached to a nylon elastic cap or rubber headband.
Variations include how the current is delivered—in an alternating pattern or in a constant, direct mode, for instance. Tweaking frequency, potency or target brain area can produce different effects as well. Reinhart’s 2022 study demonstrated that low or high frequencies and alternating currents were uniquely tied to either short-term or long-term memory improvements.
Sessions may be 20 minutes per day over the course of several days or two weeks. “[The subject] may feel a tingling, warming, poking or itching sensation,” says Reinhart, which typically goes away within a minute.
The other main approach to NIBS is Transcranial Magnetic Simulation (TMS). It involves the use of an electromagnetic coil that is held or placed against the forehead or scalp to activate nerve cells in the brain through short pulses. The stimulation is stronger than tES but similar to a magnetic resonance imaging (MRI) scan.
The subject may feel a slight knocking or tapping on the head during a 20-to-60-minute session. Scalp discomfort and headaches are reported by some; in very rare cases, a seizure can occur.
No head-to-head trials have been conducted yet to evaluate the differences and effectiveness between electrical and magnetic current stimulation, notes Lanctôt, who is also a professor of psychiatry and pharmacology at the University of Toronto. Although TMS was approved by the FDA in 2008 to treat major depression, both techniques are considered experimental for the purpose of cognitive enhancement.
“One attractive feature of tES is that it’s inexpensive—one-fifth the price of magnetic stimulation,” Reinhart notes.
Don’t confuse either of these procedures with the horrors of electroconvulsive therapy (ECT) in the 1950s and ‘60s. ECT is a more powerful, riskier procedure used only as a last resort in treating severe mental illness today.
Clinical studies on NIBS remain scarce. Standardized parameters and measures for testing have not been developed. The high heterogeneity among the many existing small NIBS studies makes it difficult to draw general conclusions. Few of the studies have been replicated and inconsistencies abound.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Lanctôt’s meta-analysis showed improvements in global cognition from delivering the magnetic form of the stimulation to people with Alzheimer’s, and this finding was replicated inan analysis in the Journal of Prevention of Alzheimer’s Disease this fall. Neither meta-analysis found clear evidence that applying the electrical currents, was helpful for Alzheimer’s subjects, but Lanctôt suggests this might be merely because the sample size for tES was smaller compared to the groups that received TMS.
At the same time, London neuroscientist Marco Sandrini, senior lecturer in psychology at the University of Roehampton, critically reviewed a series of studies on the effects of tES on episodic memory. Often declining with age, episodic memory relates to recalling a person’s own experiences from the past. Sandrini’s review concluded that delivering tES to the prefrontal or temporoparietal cortices of the brain might enhance episodic memory in older adults with Alzheimer’s disease and amnesiac mild cognitive impairment (the predementia phase of Alzheimer’s when people start to have symptoms).
Researchers readily tick off studies needed to explore, clarify and validate existing NIBS data. What is the optimal stimulus session frequency, spacing and duration? How intense should the stimulus be and where should it be targeted for what effect? How might genetics or degree of brain impairment affect responsiveness? Would adjunct medication or cognitive training boost positive results? Could administering the stimulus while someone sleeps expedite memory consolidation?
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain.
While Sandrini’s review reported improvements induced by tES in the recall or recognition of words and images, there is no evidence it will translate into improvements in daily activities. This is another question that will require more research and testing, Sandrini notes.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Where the science is headed
Learning how to apply precision medicine to NIBS is the next focus in advancing this technology, says Shankar Tumati, a post-doctoral fellow working with Lanctôt.
There is great variability in each person’s brain anatomy—the thickness of the skull, the brain’s unique folds, the amount of cerebrospinal fluid. All of these structural differences impact how electrical or magnetic stimulation is distributed in the brain and ultimately the effects.
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain, from where to put the electrodes to determining the exact dose and duration of stimulation needed to achieve lasting results, Sandrini says.
Above all, most neuroscientists say that largescale research studies over long periods of time are necessary to confirm the safety and durability of this therapy for the purpose of boosting memory. Short of that, there can be no FDA approval or medical regulation for this clinical use.
Lanctôt urges people to seek out clinical NIBS trials in their area if they want to see the science advance. “That is how we’ll find the answers,” she says, predicting it will be 5 to 10 years to develop each additional clinical application of NIBS. Ultimately, she predicts that reigning in Alzheimer’s disease and mild cognitive impairment will require a multi-pronged approach that includes lifestyle and medications, too.
Sandrini believes that scientific efforts should focus on preventing or delaying Alzheimer’s. “We need to start intervention earlier—as soon as people start to complain about forgetting things,” he says. “Changes in the brain start 10 years before [there is a problem]. Once Alzheimer’s develops, it is too late.”