Staying well in the 21st century is like playing a game of chess
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

The control of infectious diseases was considered to be one of the “10 Great Public Health Achievements.” What we didn’t take into account was the very concept of evolution: as we built better protections, our enemies eventually boosted their attacking prowess, so soon enough we found ourselves on the defensive once again.
This article originally appeared in One Health/One Planet, a single-issue magazine that explores how climate change and other environmental shifts are increasing vulnerabilities to infectious diseases by land and by sea. The magazine probes how scientists are making progress with leaders in other fields toward solutions that embrace diverse perspectives and the interconnectedness of all lifeforms and the planet.
On July 30, 1999, the Centers for Disease Control and Prevention published a report comparing data on the control of infectious disease from the beginning of the 20th century to the end. The data showed that deaths from infectious diseases declined markedly. In the early 1900s, pneumonia, tuberculosis and diarrheal diseases were the three leading killers, accounting for one-third of total deaths in the U.S.—with 40 percent being children under five.
Mass vaccinations, the discovery of antibiotics and overall sanitation and hygiene measures eventually eradicated smallpox, beat down polio, cured cholera, nearly rid the world of tuberculosis and extended the U.S. life expectancy by 25 years. By 1997, there was a shift in population health in the U.S. such that cancer, diabetes and heart disease were now the leading causes of death.
The control of infectious diseases is considered to be one of the “10 Great Public Health Achievements.” Yet on the brink of the 21st century, new trouble was already brewing. Hospitals were seeing periodic cases of antibiotic-resistant infections. Novel viruses, or those that previously didn’t afflict humans, began to emerge, causing outbreaks of West Nile, SARS, MERS or swine flu.In the years that followed, tuberculosis made a comeback, at least in certain parts of the world. What we didn’t take into account was the very concept of evolution: as we built better protections, our enemies eventually boosted their attacking prowess, so soon enough we found ourselves on the defensive once again.
At the same time, new, previously unknown or extremely rare disorders began to rise, such as autoimmune or genetic conditions. Two decades later, scientists began thinking about health differently—not as a static achievement guaranteed to last, but as something dynamic and constantly changing—and sometimes, for the worse.
What emerged since then is a different paradigm that makes our interactions with the microbial world more like a biological chess match, says Victoria McGovern, a biochemist and program officer for the Burroughs Wellcome Fund’s Infectious Disease and Population Sciences Program. In this chess game, humans may make a clever strategic move, which could involve creating a new vaccine or a potent antibiotic, but that advantage is fleeting. At some point, the organisms we are up against could respond with a move of their own—such as developing resistance to medication or genetic mutations that attack our bodies. Simply eradicating the “opponent,” or the pathogenic microbes, as efficiently as possible isn’t enough to keep humans healthy long-term.
Instead, scientists should focus on studying the complexity of interactions between humans and their pathogens. “We need to better understand the lifestyles of things that afflict us,” McGovern says. “The solutions are going to be in understanding various parts of their biology so we can influence how they behave around our systems.”
Genetics and cell biology, combined with imaging techniques that allow one to see tissues and individual cells in actions, will enable scientists to define and quantify what it means to be healthy at the molecular level.
What is being proposed will require a pivot to basic biology and other disciplines that have suffered from lack of research funding in recent years. Yet, according to McGovern, the research teams of funded proposals are answering bigger questions. “We look for people exploring questions about hosts and pathogens, and what happens when they touch, but we’re also looking for people with big ideas,” she says. For example, if one specific infection causes a chain of pathological events in the body, can other infections cause them too? And if we find a way to break that chain for one pathogen, can we play the same trick on another? “We really want to see people thinking of not just one experiment but about big implications of their work,” McGovern says.
Jonah Cool, a cell biologist, geneticist and science officer at the Chan Zuckerberg Initiative, says that it’s necessary to define what constitutes a healthy organism and how it overcomes infections or environmental assaults, such as pollution from forest fires or toxins from industrial smokestacks. An organism that catches a disease isn’t necessarily an unhealthy one, as long as it fights it off successfully—an ability that arises from the complex interplay of its genes, the immune system, age, stress levels and other factors. Modern science allows many of these factors to be measured, recorded and compared. “We need a data-driven, deep-phenotyping approach to defining healthy biological systems and their responses to insults—which can be infectious disease or environmental exposures—and their ability to navigate their way through that space,” Cool says.
Genetics and cell biology, combined with imaging techniques that allow one to see tissues and individual cells in actions, will enable scientists to define and quantify what it means to be healthy at the molecular level. “As a geneticist and cell biologist, I believe in all these molecular underpinnings and how they arise in phenotypic differences in cells, genes, proteins—and how their combinations form complex cellular states,” Cool says.
Julie Graves, a physician, public health consultant, former adjunct professor of management, policy and community health at the University of Texas Health Science Center in Houston, stresses the necessity of nutritious diets. According to the Rockefeller Food Initiative, “poor diet is the leading risk factor for disease, disability and premature death in the majority of countries around the world.” Adequate nutrition is critical for maintaining human health and life. Yet, Western diets are often low in essential nutrients, high in calories and heavy on processed foods. Overconsumption of these foods has contributed to high rates of obesity and chronic disease in the U.S. In fact, more than half of American adults have at least one chronic disease, and 27 percent have more than one—which increases vulnerability to COVID-19 infections, according to the 2018 National Health Interview Survey.
Further, the contamination of our food supply with various agricultural and industrial toxins—petrochemicals, pesticides, PFAS and others—has implications for morbidity, mortality, and overall quality of life. “These chemicals are insidiously in everything, including our bodies,” Graves says—and they are interfering with our normal biological functions. “We need to stop how we manufacture food,” she adds, and rid our sustenance of these contaminants.
According to the Humane Society of the United States, factory farms result in nearly 40 percent of emissions of methane. Concentrated animal feeding operations or CAFOs may serve as breeding grounds for pandemics, scientists warn, so humans should research better ways to raise and treat livestock. Diego Rose, a professor of food and nutrition policy at Tulane University School of Public Health & Tropical Medicine, and his colleagues found that “20 percent of Americans’ diets account for about 45 percent of the environmental impacts [that come from food].” A subsequent study explored the impacts of specific foods and found that substituting beef for chicken lowers an individual’s carbon footprint by nearly 50 percent, with water usage decreased by 30 percent. Notably, however, eating too much red meat has been associated with a variety of illnesses.
In some communities, the option to swap food types is limited or impossible. For example, “many populations live in relative food deserts where there’s not a local grocery store that has any fresh produce,” says Louis Muglia, the president and CEO of Burroughs Wellcome. Individuals in these communities suffer from an insufficient intake of beneficial macronutrients, and they’re “probably being exposed to phenols and other toxins that are in the packaging.” An equitable, sustainable and nutritious food supply will be vital to humanity’s wellbeing in the era of climate change, unpredictable weather and spillover events.
A recent report by See Change Institute and the Climate Mental Health Network showed that people who are experiencing socioeconomic inequalities, including many people of color, contribute the least to climate change, yet they are impacted the most. For example, people in low-income communities are disproportionately exposed to vehicle emissions, Muglia says. Through its Climate Change and Human Health Seed Grants program, Burroughs Wellcome funds research that aims to understand how various factors related to climate change and environmental chemicals contribute to premature births, associated with health vulnerabilities over the course of a person’s life—and map such hot spots.
“It’s very complex, the combinations of socio-economic environment, race, ethnicity and environmental exposure, whether that’s heat or toxic chemicals,” Muglia explains. “Disentangling those things really requires a very sophisticated, multidisciplinary team. That’s what we’ve put together to describe where these hotspots are and see how they correlate with different toxin exposure levels.”
In addition to mapping the risks, researchers are developing novel therapeutics that will be crucial to our armor arsenal, but we will have to be smarter at designing and using them. We will need more potent, better-working monoclonal antibodies. Instead of directly attacking a pathogen, we may have to learn to stimulate the immune system—training it to fight the disease-causing microbes on its own. And rather than indiscriminately killing all bacteria with broad-scope drugs, we would need more targeted medications. “Instead of wiping out the entire gut flora, we will need to come up with ways that kill harmful bacteria but not healthy ones,” Graves says. Training our immune systems to recognize and react to pathogens by way of vaccination will keep us ahead of our biological opponents, too. “Continued development of vaccines against infectious diseases is critical,” says Graves.
With all of the unpredictable events that lie ahead, it is difficult to foresee what achievements in public health will be reported at the end of the 21st century. Yet, technological advances, better modeling and pursuing bigger questions in science, along with education and working closely with communities will help overcome the challenges. The Chan Zuckerberg Initiative displays an optimistic message on its website: “Is it possible to cure, prevent, or manage all diseases by the end of this century? We think so.” Cool shares the view of his employer—and believes that science can get us there. Just give it some time and a chance. “It’s a big, bold statement,” he says, “but the end of the century is a long way away.”Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
New approach to brain health is sparking memories
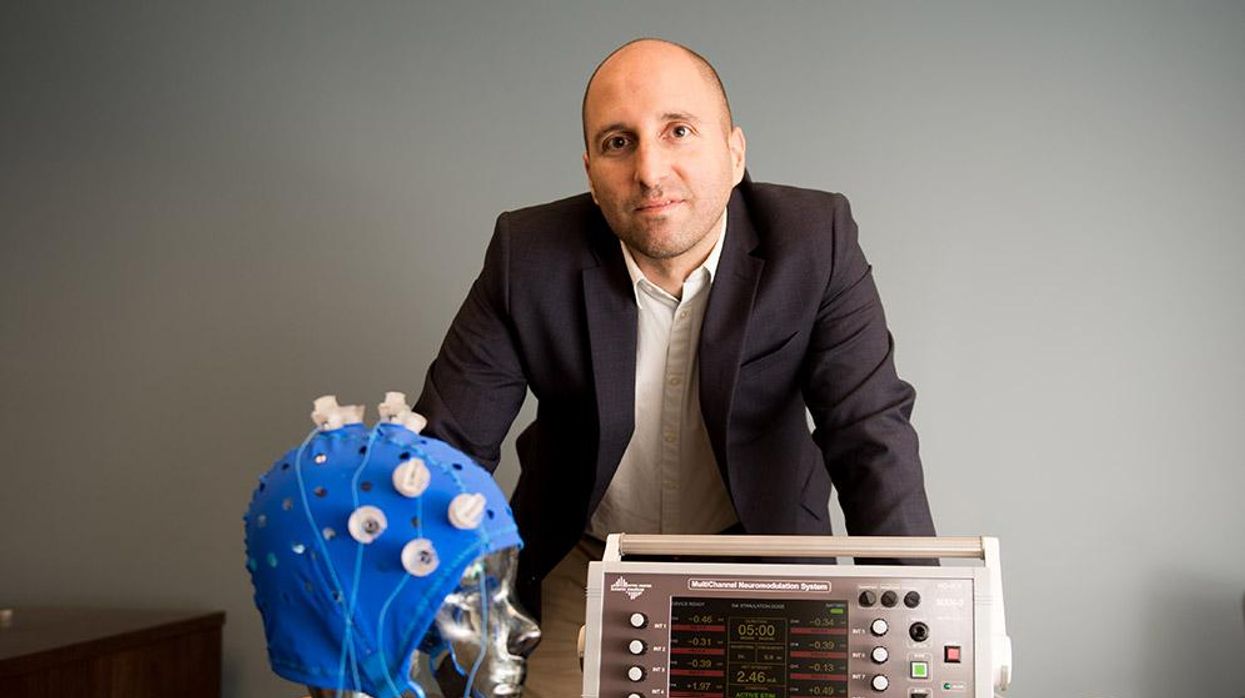
This fall, Robert Reinhart of Boston University published a study finding that electrical stimulation can boost memory - and Reinhart was surprised to discover the effects lasted a full month.
What if a few painless electrical zaps to your brain could help you recall names, perform better on Wordle or even ward off dementia?
This is where neuroscientists are going in efforts to stave off age-related memory loss as well as Alzheimer’s disease. Medications have shown limited effectiveness in reversing or managing loss of brain function so far. But new studies suggest that firing up an aging neural network with electrical or magnetic current might keep brains spry as we age.
Welcome to non-invasive brain stimulation (NIBS). No surgery or anesthesia is required. One day, a jolt in the morning with your own battery-operated kit could replace your wake-up coffee.
Scientists believe brain circuits tend to uncouple as we age. Since brain neurons communicate by exchanging electrical impulses with each other, the breakdown of these links and associations could be what causes the “senior moment”—when you can’t remember the name of the movie you just watched.
In 2019, Boston University researchers led by Robert Reinhart, director of the Cognitive and Clinical Neuroscience Laboratory, showed that memory loss in healthy older adults is likely caused by these disconnected brain networks. When Reinhart and his team stimulated two key areas of the brain with mild electrical current, they were able to bring the brains of older adult subjects back into sync — enough so that their ability to remember small differences between two images matched that of much younger subjects for at least 50 minutes after the testing stopped.
Reinhart wowed the neuroscience community once again this fall. His newer study in Nature Neuroscience presented 150 healthy participants, ages 65 to 88, who were able to recall more words on a given list after 20 minutes of low-intensity electrical stimulation sessions over four consecutive days. This amounted to a 50 to 65 percent boost in their recall.
Even Reinhart was surprised to discover the enhanced performance of his subjects lasted a full month when they were tested again later. Those who benefited most were the participants who were the most forgetful at the start.

An older person participates in Robert Reinhart's research on brain stimulation.
Robert Reinhart
Reinhart’s subjects only suffered normal age-related memory deficits, but NIBS has great potential to help people with cognitive impairment and dementia, too, says Krista Lanctôt, the Bernick Chair of Geriatric Psychopharmacology at Sunnybrook Health Sciences Center in Toronto. Plus, “it is remarkably safe,” she says.
Lanctôt was the senior author on a meta-analysis of brain stimulation studies published last year on people with mild cognitive impairment or later stages of Alzheimer’s disease. The review concluded that magnetic stimulation to the brain significantly improved the research participants’ neuropsychiatric symptoms, such as apathy and depression. The stimulation also enhanced global cognition, which includes memory, attention, executive function and more.
This is the frontier of neuroscience.
The two main forms of NIBS – and many questions surrounding them
There are two types of NIBS. They differ based on whether electrical or magnetic stimulation is used to create the electric field, the type of device that delivers the electrical current and the strength of the current.
Transcranial Current Brain Stimulation (tES) is an umbrella term for a group of techniques using low-wattage electrical currents to manipulate activity in the brain. The current is delivered to the scalp or forehead via electrodes attached to a nylon elastic cap or rubber headband.
Variations include how the current is delivered—in an alternating pattern or in a constant, direct mode, for instance. Tweaking frequency, potency or target brain area can produce different effects as well. Reinhart’s 2022 study demonstrated that low or high frequencies and alternating currents were uniquely tied to either short-term or long-term memory improvements.
Sessions may be 20 minutes per day over the course of several days or two weeks. “[The subject] may feel a tingling, warming, poking or itching sensation,” says Reinhart, which typically goes away within a minute.
The other main approach to NIBS is Transcranial Magnetic Simulation (TMS). It involves the use of an electromagnetic coil that is held or placed against the forehead or scalp to activate nerve cells in the brain through short pulses. The stimulation is stronger than tES but similar to a magnetic resonance imaging (MRI) scan.
The subject may feel a slight knocking or tapping on the head during a 20-to-60-minute session. Scalp discomfort and headaches are reported by some; in very rare cases, a seizure can occur.
No head-to-head trials have been conducted yet to evaluate the differences and effectiveness between electrical and magnetic current stimulation, notes Lanctôt, who is also a professor of psychiatry and pharmacology at the University of Toronto. Although TMS was approved by the FDA in 2008 to treat major depression, both techniques are considered experimental for the purpose of cognitive enhancement.
“One attractive feature of tES is that it’s inexpensive—one-fifth the price of magnetic stimulation,” Reinhart notes.
Don’t confuse either of these procedures with the horrors of electroconvulsive therapy (ECT) in the 1950s and ‘60s. ECT is a more powerful, riskier procedure used only as a last resort in treating severe mental illness today.
Clinical studies on NIBS remain scarce. Standardized parameters and measures for testing have not been developed. The high heterogeneity among the many existing small NIBS studies makes it difficult to draw general conclusions. Few of the studies have been replicated and inconsistencies abound.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Lanctôt’s meta-analysis showed improvements in global cognition from delivering the magnetic form of the stimulation to people with Alzheimer’s, and this finding was replicated inan analysis in the Journal of Prevention of Alzheimer’s Disease this fall. Neither meta-analysis found clear evidence that applying the electrical currents, was helpful for Alzheimer’s subjects, but Lanctôt suggests this might be merely because the sample size for tES was smaller compared to the groups that received TMS.
At the same time, London neuroscientist Marco Sandrini, senior lecturer in psychology at the University of Roehampton, critically reviewed a series of studies on the effects of tES on episodic memory. Often declining with age, episodic memory relates to recalling a person’s own experiences from the past. Sandrini’s review concluded that delivering tES to the prefrontal or temporoparietal cortices of the brain might enhance episodic memory in older adults with Alzheimer’s disease and amnesiac mild cognitive impairment (the predementia phase of Alzheimer’s when people start to have symptoms).
Researchers readily tick off studies needed to explore, clarify and validate existing NIBS data. What is the optimal stimulus session frequency, spacing and duration? How intense should the stimulus be and where should it be targeted for what effect? How might genetics or degree of brain impairment affect responsiveness? Would adjunct medication or cognitive training boost positive results? Could administering the stimulus while someone sleeps expedite memory consolidation?
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain.
While Sandrini’s review reported improvements induced by tES in the recall or recognition of words and images, there is no evidence it will translate into improvements in daily activities. This is another question that will require more research and testing, Sandrini notes.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Where the science is headed
Learning how to apply precision medicine to NIBS is the next focus in advancing this technology, says Shankar Tumati, a post-doctoral fellow working with Lanctôt.
There is great variability in each person’s brain anatomy—the thickness of the skull, the brain’s unique folds, the amount of cerebrospinal fluid. All of these structural differences impact how electrical or magnetic stimulation is distributed in the brain and ultimately the effects.
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain, from where to put the electrodes to determining the exact dose and duration of stimulation needed to achieve lasting results, Sandrini says.
Above all, most neuroscientists say that largescale research studies over long periods of time are necessary to confirm the safety and durability of this therapy for the purpose of boosting memory. Short of that, there can be no FDA approval or medical regulation for this clinical use.
Lanctôt urges people to seek out clinical NIBS trials in their area if they want to see the science advance. “That is how we’ll find the answers,” she says, predicting it will be 5 to 10 years to develop each additional clinical application of NIBS. Ultimately, she predicts that reigning in Alzheimer’s disease and mild cognitive impairment will require a multi-pronged approach that includes lifestyle and medications, too.
Sandrini believes that scientific efforts should focus on preventing or delaying Alzheimer’s. “We need to start intervention earlier—as soon as people start to complain about forgetting things,” he says. “Changes in the brain start 10 years before [there is a problem]. Once Alzheimer’s develops, it is too late.”
Will religious people reject organ transplants from pigs?
Scientists are getting better at transplanting pig organs into humans. But religious followers of prohibitions on consuming pork may reject these organs, even if their bodies could accept them.
The first successful recipient of a human heart transplant lived 18 days. The first artificial heart recipient lived just over 100.
Their brief post-transplant lives paved the way toward vastly greater successes. Former Vice President Dick Cheney relied on an artificial heart for nearly two years before receiving a human heart transplant. It still beats in his chest more than a decade later.
Organ transplantation recently reached its next phase with David Bennett. He survived for two months after becoming the first recipient of a pig’s heart genetically modified to function in a human body in February. Known as a xenotransplant, the procedure could pave the way for greatly expanding the use of transplanted vital organs to extend human lives.
Clinical trials would have to be held in the U.S. before xenotransplants become widespread; Bennett’s surgery was authorized under a special Food and Drug Administration program that addresses patients with life-threatening medical conditions.
German researchers plan to perform eight pig-to-human heart transplants as part of a clinical trial beginning in 2024. According to an email sent to Leaps.org by three scholars working on the German project, these procedures will focus on one of the reasons David Bennett did not survive longer: A porcine infection from his new heart.
The transplant team will conduct more sensitive testing of the donor organs, “which in all likelihood will be able to detect even low levels of virus in the xenograft,” note the scientists, Katharina Ebner, Jochen Ostheimer and Jochen Sautermeister. They are confident that the risk of infection with a porcine virus in the future will be significantly lower.
Moreover, hearts are not the only genetically modified organs that are being xenotransplanted. A team of surgeons at the University of Alabama at Birmingham successfully transplanted genetically modified pig kidneys into a brain-dead human recipient in September. The kidneys functioned normally for more than three days before the experiment ended. The UAB team is now moving forward with clinical trials focusing on transplanting pig kidneys into human patients.
Some experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent of NYU Langone Health.
Douglas Anderson, a surgeon who is part of that kidney xenotransplant team, observes that, “organ shortages have been the major issue facing transplantation since its inception” and that xenotransplantation is a potential solution to that quandary. “It can’t be understated the number of people waiting for a kidney on dialysis, which has a significant mortality rate,” he says. According to the advocacy group Donate Life America, more than 100,000 people in the U.S. alone are waiting for a donated organ, and 85 percent of them need a kidney.
Other experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent, director of transplant ethics and policy at NYU Langone Health, a New York City-based hospital system. Like the UAB team, surgeons at NYU Langone have had success coaxing modified pig kidneys to work in deceased humans.
“There is a genuinely good chance that within a generation, (xenotransplantation) might become very common in reasonably wealthy countries,” says Michael Reiss, professor of science education at University College in London. In addition to his academic position, Reiss sits on the Nuffield Council on Bioethics, a nonprofit that is one of Britain’s most prominent watchdogs regarding medical and scientific issues. Reiss is also an Anglican priest and has studied xenotransplantation from both a scientific and religious point of view.
Moreover, genetic modifications could one day lead to organs being specifically optimized for their recipients. That could ensure issues like donor rejection and the calculated risk of artificially suppressing recipient immune systems become concerns of the past.
Major bioethical, religious concerns
Despite the promise of xenotransplantation, numerous bioethical issues swirl around the procedure. They could be magnified if xenotransplantation evolves from one-off experiments to a routine medical procedure.
One of the biggest is the millennia-long prohibitions Islam and Judaism have had regarding the consumption of pork. Will followers of these religions assume such rules extend to those taboo materials being inserted into a human body?
“Initially, one’s instinctual reaction is that, oh, crumbs! – how are Jews and Muslims going to react to that?” Reiss says. But in a world where science and secularism are accepted on an everyday basis, he notes it is not a significant issue. Reiss points out that valves from pig hearts have been used in human patients for decades without any issues. He adds that both Islam and Judaism waive religious dietary restrictions if a human life is at risk.
“While nobody's saying an individual patient is to be forced to have these, the very high proportion of people who identify as Jews or Muslims when given this option are content with it,” he says.
Concurring with Reiss is Michael Gusamano, professor of health policy at Lehigh University and director of its Center for Ethics. He is currently performing research on the ethics of xenotransplantation for the National Institutes of Health.
“Leaders from all major religions have commented on this and have indicated that this is not inconsistent with religious doctrine,” Gusamano says in written remarks to Leaps.org. “Having said that, it is plausible to believe that some people will assume that this is inconsistent with the teaching of their religion and may object to…receiving a xenotransplant as part of routine medical care.”
A history of clashes
Despite those assurances, science has long clashed with theology. Although Galileo proved the planets revolved around the sun, the Catholic Church found him guilty of heresy and rewarded his discovery with house arrest for the last decade of his life. A revolt occurred in mid-19th century India after native-born soldiers believed the ammunition supplied by their British occupiers had been lubricated with pork and beef tallow. Given they had to use their mouths to tear open ammunition pouches, this violated both the tenets of Islam and Hinduism. And one of the conspiracy theories hatched as a result of COVID-19 was that the vaccines developed to fight the disease were the “mark of the beast” – a sign of impending Armageddon under evangelical Christian theology.
The German xenotransplant research team has encountered such potential concerns when the procedure is regarded through a religious lens. “The pastors in our research suspected that many recipients might feel disgust and revulsion,” they write. “Even beyond these special religious reservations, cultural scripts about pigs as inferior living beings are also generally widespread and effective in the western world, so that here too possible disgust reactions cannot be ruled out.”
The German researchers add that “Jewish and Muslim hospital pastoral workers believe possible considerable problems in this respect, which must be dealt with psychosocially, religiously, and pastorally prior to a possible transplantation in order to strengthen the acceptance of the received organ by the patients and their relatives.”
Parent, the director at NYU Langone, shares a concern that xenotransplantation could move “too fast,” although much of his worry is focused on zoonotic disease transmission – pig viruses jumping into humans as a result of such procedures.
Another ethical issue
Moreover, the way pigs and other animals are raised for transplants could pose future ethical dilemmas.
Reiss notes that pigs raised for medical procedures have to be grown and kept in what are known as a designated pathogen-free facility, or DPF. Such facilities are kept painstakingly antiseptic so as to minimize the risk of zoonotic transmissions. But given pigs are fond of outdoor activities such as wallowing in mud and sleeping on hay, they lead “stunningly boring lives” that they probably do not enjoy, Reiss observes.
Ethical concerns with using pigs may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting.
“There’s no doubt that these research pigs have gotten much better veterinary care, et cetera, (compared to farmed pigs). But it’s not a great life,” Reiss says. “And although it hasn’t so far dominated the discussion, I think as the years go by, rather as we’ve seen with the use of apes and now monkeys in medical research, more and more theologians will get uncomfortable about us just assuming we can do this with…pigs.”
The German research team raises the same concerns, but has taken a fairly sanguine view on the topic. “The impairments of the species-typical behavior will certainly provoke criticism and perhaps also public protest. But the number of animals affected is very small in relation to slaughter cattle,” the German researchers note. “Moreover, the conditions there and also in several animal experiments are far worse.”
Observers say that may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting. Anderson, the UAB transplant surgeon, believes such an accomplishment remains decades away.
But other experts believe there is a moral imperative that xenotransplantation remain a temporary solution. “I think we have a duty to go in that direction,” Parent says. “We have to go that way, with the xenotransplantation process (as) a steppingstone and research path that will be useful for bioengineered organs.”