Researchers advance drugs that treat pain without addiction
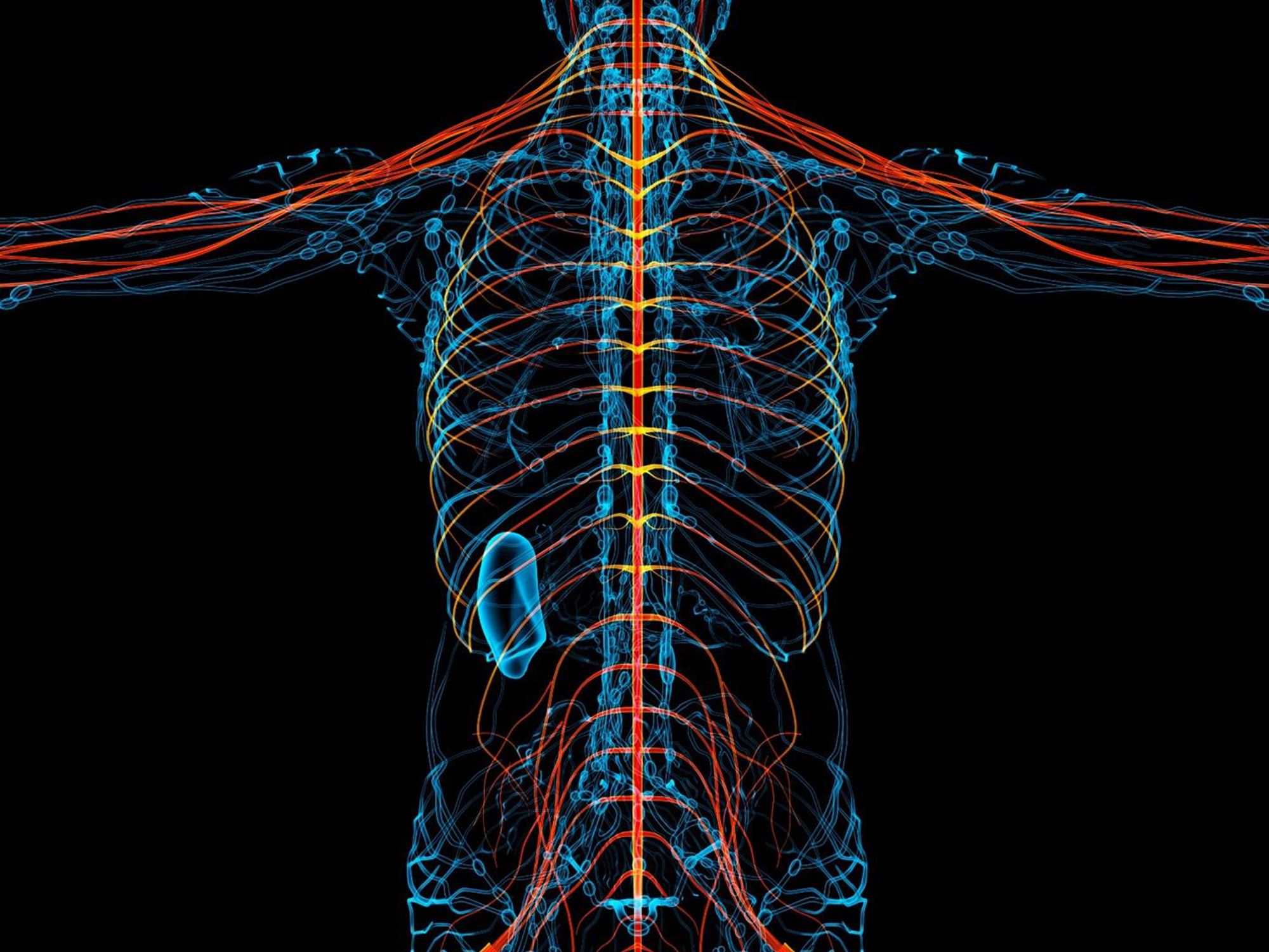
New therapies are using creative approaches that target the body’s sensory neurons, which send pain signals to the brain.
Opioids are one of the most common ways to treat pain. They can be effective but are also highly addictive, an issue that has fueled the ongoing opioid crisis. In 2020, an estimated 2.3 million Americans were dependent on prescription opioids.
Opioids bind to receptors at the end of nerve cells in the brain and body to prevent pain signals. In the process, they trigger endorphins, so the brain constantly craves more. There is a huge risk of addiction in patients using opioids for chronic long-term pain. Even patients using the drugs for acute short-term pain can become dependent on them.
Scientists have been looking for non-addictive drugs to target pain for over 30 years, but their attempts have been largely ineffective. “We desperately need alternatives for pain management,” says Stephen E. Nadeau, a professor of neurology at the University of Florida.
A “dimmer switch” for pain
Paul Blum is a professor of biological sciences at the University of Nebraska. He and his team at Neurocarrus have created a drug called N-001 for acute short-term pain. N-001 is made up of specially engineered bacterial proteins that target the body’s sensory neurons, which send pain signals to the brain. The proteins in N-001 turn down pain signals, but they’re too large to cross the blood-brain barrier, so they don’t trigger the release of endorphins. There is no chance of addiction.
When sensory neurons detect pain, they become overactive and send pain signals to the brain. “We wanted a way to tone down sensory neurons but not turn them off completely,” Blum reveals. The proteins in N-001 act “like a dimmer switch, and that's key because pain is sensation overstimulated.”
Blum spent six years developing the drug. He finally managed to identify two proteins that form what’s called a C2C complex that changes the structure of a subunit of axons, the parts of neurons that transmit electrical signals of pain. Changing the structure reduces pain signaling.
“It will be a long path to get to a successful clinical trial in humans," says Stephen E. Nadeau, professor of neurology at the University of Florida. "But it presents a very novel approach to pain reduction.”
Blum is currently focusing on pain after knee and ankle surgery. Typically, patients are treated with anesthetics for a short time after surgery. But anesthetics usually only last for 4 to 6 hours, and long-term use is toxic. For some, the pain subsides. Others continue to suffer after the anesthetics have worn off and start taking opioids.
N-001 numbs sensation. It lasts for up to 7 days, much longer than any anesthetic. “Our goal is to prolong the time before patients have to start opioids,” Blum says. “The hope is that they can switch from an anesthetic to our drug and thereby decrease the likelihood they're going to take the opioid in the first place.”
Their latest animal trial showed promising results. In mice, N-001 reduced pain-like behaviour by 90 percent compared to the control group. One dose became effective in two hours and lasted a week. A high dose had pain-relieving effects similar to an opioid.
Professor Stephen P. Cohen, director of pain operations at John Hopkins, believes the Neurocarrus approach has potential but highlights the need to go beyond animal testing. “While I think it's promising, it's an uphill battle,” he says. “They have shown some efficacy comparable to opioids, but animal studies don't translate well to people.”
Nadeau, the University of Florida neurologist, agrees. “It will be a long path to get to a successful clinical trial in humans. But it presents a very novel approach to pain reduction.”
Blum is now awaiting approval for phase I clinical trials for acute pain. He also hopes to start testing the drug's effect on chronic pain.
Learning from people who feel no pain
Like Blum, a pharmaceutical company called Vertex is focusing on treating acute pain after surgery. But they’re doing this in a different way, by targeting a sodium channel that plays a critical role in transmitting pain signals.
In 2004, Stephen Waxman, a neurology professor at Yale, led a search for genetic pain anomalies and found that biologically related people who felt no pain despite fractures, burns and even childbirth had mutations in the Nav1.7 sodium channel. Further studies in other families who experienced no pain showed similar mutations in the Nav1.8 sodium channel.
Scientists set out to modify these channels. Many unsuccessful efforts followed, but Vertex has now developed VX-548, a medicine to inhibit Nav1.8. Typically, sodium ions flow through sodium channels to generate rapid changes in voltage which create electrical pulses. When pain is detected, these pulses in the Nav1.8 channel transmit pain signals. VX-548 uses small molecules to inhibit the channel from opening. This blocks the flow of sodium ions and the pain signal. Because Nav1.8 operates only in peripheral nerves, located outside the brain, VX-548 can relieve pain without any risk of addiction.
"Frankly we need drugs for chronic pain more than acute pain," says Waxman.
The team just finished phase II clinical trials for patients following abdominoplasty surgery and bunionectomy surgery.
After abdominoplasty surgery, 76 patients were treated with a high dose of VX-548. Researchers then measured its effectiveness in reducing pain over 48 hours, using the SPID48 scale, in which higher scores are desirable. The score for Vertex’s drug was 110.5 compared to 72.7 in the placebo group, whereas the score for patients taking an opioid was 85.2. The study involving bunionectomy surgery showed positive results as well.
Waxman, who has been at the forefront of studies into Nav1.7 and Nav1.8, believes that Vertex's results are promising, though he highlights the need for further clinical trials.
“Blocking Nav1.8 is an attractive target,” he says. “[Vertex is] studying pain that is relatively simple and uniform, and that's key to having a drug trial that is informative. But the study needs to be replicated and frankly we need drugs for chronic pain more than acute pain. If this is borne out by additional studies, it's one important step in a journey.”
Vertex will be launching phase III trials later this year.
Finding just the right amount of Nerve Growth Factor
Whereas Neurocarrus and Vertex are targeting short-term pain, a company called Levicept is concentrating on relieving chronic osteoarthritis pain. Around 32.5 million Americans suffer from osteoarthritis. Patients commonly take NSAIDs, or non-steroidal anti-inflammatory drugs, but they cannot be taken long-term. Some take opioids but they aren't very effective.
Levicept’s drug, Levi-04, is designed to modify a signaling pathway associated with pain. Nerve Growth Factor (NGF) is a neurotrophin: it’s involved in nerve growth and function. NGF signals by attaching to receptors. In pain there are excess neurotrophins attaching to receptors and activating pain signals.
“What Levi-04 does is it returns the natural equilibrium of neurotrophins,” says Simon Westbrook, the CEO and founder of Levicept. It stabilizes excess neurotrophins so that the NGF pathway does not signal pain. Levi-04 isn't addictive since it works within joints and in nerves outside the brain.
Westbrook was initially involved in creating an anti-NGF molecule for Pfizer called Tanezumab. At first, Tanezumab seemed effective in clinical trials and other companies even started developing their own versions. However, a problem emerged. Tanezumab caused rapidly progressive osteoarthritis, or RPOA, in some patients because it completely removed NGF from the system. NGF is not just involved in pain signalling, it’s also involved in bone growth and maintenance.
Levicept has found a way to modify the NGF pathway without completely removing NGF. They have now finished a small-scale phase I trial mainly designed to test safety rather than efficacy. “We demonstrated that Levi-04 is safe and that it bound to its target, NGF,” says Westbrook. It has not caused RPOA.
Professor Philip Conaghan, director of the Leeds Institute of Rheumatic and Musculoskeletal Medicine, believes that Levi-04 has potential but urges the need for caution. “At this early stage of development, their molecule looks promising for osteoarthritis pain,” he says. “They will have to watch out for RPOA which is a potential problem.”
Westbrook starts phase II trials with 500 patients this summer to check for potential side effects and test the drug’s efficacy.
There is a real push to find an effective alternative to opioids. “We have a lot of work to do,” says Professor Waxman. “But I am confident that we will be able to develop new, much more effective pain therapies.”
Scientists are making progress to create a one-time therapy that would permanently lower LDL cholesterol to prevent heart attacks caused by high LDL.
Later this year, Verve Therapeutics of Cambridge, Ma., will initiate Phase 1 clinical trials to test VERVE-101, a new medication that, if successful, will employ gene editing to significantly reduce low-density lipoprotein cholesterol, or LDL.
LDL is sometimes referred to as the “bad” cholesterol because it collects in the walls of blood vessels, and high levels can increase chances of a heart attack, cardiovascular disease or stroke. There are approximately 600,000 heart attacks per year due to blood cholesterol damage in the United States, and heart disease is the number one cause of death in the world. According to the CDC, a 10 percent decrease in total blood cholesterol levels can reduce the incidence of heart disease by as much as 30 percent.
Verve’s Founder and CEO, Sekar Kathiresan, spent two decades studying the genetic basis for heart attacks while serving as a professor of medicine at Harvard Medical School. His research led to two critical insights.
“One is that there are some people that are naturally resistant to heart attack and have lifelong, low levels of LDL,” the cardiologist says. “Second, there are some genes that can be switched off that lead to very low LDL cholesterol, and individuals with those genes switched off are resistant to heart attacks.”
Kathiresan and his team formed a hypothesis in 2016 that if they could develop a medicine that mimics the natural protection that some people enjoy, then they might identify a powerful new way to treat and ultimately prevent heart attacks. They launched Verve in 2018 with the goal of creating a one-time therapy that would permanently lower LDL and eliminate heart attacks caused by high LDL.
"Imagine a future where somebody gets a one-time treatment at the time of their heart attack or before as a preventive measure," says Kathiresan.
The medication is targeted specifically for patients who have a genetic form of high cholesterol known as heterozygous familial hypercholesterolemia, or FH, caused by expression of a gene called PCSK9. Verve also plans to develop a program to silence a gene called ANGPTL3 for patients with FH and possibly those with or at risk of atherosclerotic cardiovascular disease.
FH causes cholesterol to be high from birth, reaching levels of 200 to 300 milligrams per deciliter. Suggested normal levels are around 100 to 129 mg/dl, and anything above 130 mg/dl is considered high. Patients with cardiovascular disease usually are asked to aim for under 70 mg/dl, but many still have unacceptably high LDL despite taking oral medications such as statins. They are more likely to have heart attacks in their 30s, 40s and 50s, and require lifelong LDL control.
The goal for drug treatments for high LDL, Kathiresan says, is to reduce LDL as low as possible for as long as possible. Physicians and researchers also know that a sizeable portion of these patients eventually start to lose their commitment to taking their statins and other LDL-controlling medications regularly.
“If you ask 100 patients one year after their heart attack what fraction are still taking their cholesterol-lowering medications, it’s less than half,” says Kathiresan. “So imagine a future where somebody gets a one-time treatment at the time of their heart attack or before as a preventive measure. It’s right in front of us, and it’s something that Verve is looking to do.”
In late 2020, Verve completed primate testing with monkeys that had genetically high cholesterol, using a one-time intravenous injection of VERVE-101. It reduced the monkeys’ LDL by 60 percent and, 18 months later, remains at that level. Kathiresan expects the LDL to stay low for the rest of their lives.
Verve’s gene editing medication is packaged in a lipid nanoparticle to serve as the delivery mechanism into the liver when infused intravenously. The drug is absorbed and makes its way into the nucleus of the liver cells.
Verve’s program targeting PCSK9 uses precise, single base, pair base editing, Kathiresan says, meaning it doesn't cut DNA like CRISPR gene editing systems do. Instead, it changes one base, or letter, in the genome to a different one without affecting the letters around it. Comparing it to a pencil and eraser, he explains that the medication erases out a letter A and makes it a letter G in the A, C, G and T code in DNA.
“We need to continue to advance our approach and tools to make sure that we have the absolute maximum ability to detect off-target effects,” says Euan Ashley, professor of medicine and genetics at Stanford University.
By making that simple change from A to G, the medication switches off the PCSK9 gene, automatically lowering LDL cholesterol.
“Once the DNA change is made, all the cells in the liver will have that single A to G change made,” Kathiresan says. “Then the liver cells divide and give rise to future liver cells, but every time the cell divides that change, the new G is carried forward.”
Additionally, Verve is pursuing its second gene editing program to eliminate ANGPTL3, a gene that raises both LDL and blood triglycerides. In 2010, Kathiresan's research team learned that people who had that gene completely switched off had LDL and triglyceride levels of about 20 and were very healthy with no heart attacks. The goal of Verve’s medication will be to switch off that gene, too, as an option for additional LDL or triglyceride lowering.
“Success with our first drug, VERVE-101, will give us more confidence to move forward with our second drug,” Kathiresan says. “And it opens up this general idea of making [genomic] spelling changes in the liver to treat other diseases.”
The approach is less ethically concerning than other gene editing technologies because it applies somatic editing that affects only the individual patient, whereas germline editing in the patient’s sperm or egg, or in an embryo, gets passed on to children. Additionally, gene editing therapies receive the same comprehensive amount of testing for side effects as any other medicine.
“We need to continue to advance our approach and tools to make sure that we have the absolute maximum ability to detect off-target effects,” says Euan Ashley, professor of medicine and genetics at Stanford University and founding director of its Center for Inherited Cardiovascular Disease. Ashley and his colleagues at Stanford’s Clinical Genomics Program and beyond are increasingly excited about the promise of gene editing.
“We can offer precision diagnostics, so increasingly we’re able to define the disease at a much deeper level using molecular tools and sequencing,” he continues. “We also have this immense power of reading the genome, but we’re really on the verge of taking advantage of the power that we now have to potentially correct some of the variants that we find on a genome that contribute to disease.”
He adds that while the gene editing medicines in development to correct genomes are ahead of the delivery mechanisms needed to get them into the body, particularly the heart and brain, he’s optimistic that those aren’t too far behind.
“It will probably take a few more years before those next generation tools start to get into clinical trials,” says Ashley, whose book, The Genome Odyssey, was published last year. “The medications might be the sexier part of the research, but if you can’t get it into the right place at the right time in the right dose and not get it to the places you don’t want it to go, then that tool is not of much use.”
Medical experts consider knocking out the PCSK9 gene in patients with the fairly common genetic disorder of familial hypercholesterolemia – roughly one in 250 people – a potentially safe approach to gene editing and an effective means of significantly lowering their LDL cholesterol.

Nurse Erin McGlennon has an Implantable Cardioverter Defibrillator and takes medications, but she is also hopeful that a gene editing medication will be developed in the near future.
Erin McGlennon
Mary McGowan, MD, chief medical officer for The Family Heart Foundation in Pasadena, CA, sees the tremendous potential for VERVE-101 and believes patients should be encouraged by the fact that this kind of research is occurring and how much Verve has accomplished in a relatively short time. However, she offers one caveat, since even a 60 percent reduction in LDL won’t completely eliminate the need to reduce the remaining amount of LDL.
“This technology is very exciting,” she said, “but we want to stress to our patients with familial hypercholesterolemia that we know from our published research that most people require several therapies to get their LDL down., whether that be in primary prevention less than 100 mg/dl or secondary prevention less than 70 mg/dl, So Verve’s medication would be an add-on therapy for most patients.”
Dr. Kathiresan concurs: “We expect our medicine to lower LDL cholesterol by about 60 percent and that our patients will be on background oral medications, including statins that lower LDL cholesterol.”
Several leading research centers are investigating gene editing treatments for other types of cardiovascular diseases. Elizabeth McNally, Elizabeth Ward Professor and Director at the Center for Genetic Medicine at Northwestern University’s Feinberg School of Medicine, pursues advanced genetic correction in neuromuscular diseases such as Duchenne muscular dystrophy and spinal muscular atrophy. A cardiologist, she and her colleagues know these diseases frequently have cardiac complications.
“Even though the field is driven by neuromuscular specialists, it’s the first therapies in patients with neuromuscular diseases that are also expected to make genetic corrections in the heart,” she says. “It’s almost like an afterthought that we’re potentially fixing the heart, too.”
Another limitation McGowan sees is that too many healthcare providers are not yet familiar with how to test patients to determine whether or not they carry genetic mutations that need to be corrected. “We need to get more genetic testing done,” she says. “For example, that’s the case with hypertrophic cardiomyopathy, where a lot of the people who probably carry that diagnosis and have never been genetically identified at a time when genetic testing has never been easier.”
One patient who has been diagnosed with hypertrophic cardiomyopathy also happens to be a nurse working in research at Genentech Pharmaceutical, now a member of the Roche Group, in South San Francisco. To treat the disease, Erin McGlennon, RN, has an Implantable Cardioverter Defibrillator and takes medications, but she is also hopeful that a gene editing medication will be developed in the near future.
“With my condition, the septum muscles are just growing thicker, so I’m on medicine to keep my heart from having dangerous rhythms,” says McGlennon of the disease that carries a low risk of sudden cardiac death. “So, the possibility of having a treatment option that can significantly improve my day-to-day functioning would be a major breakthrough.”
McGlennon has some control over cardiovascular destiny through at least one currently available technology: in vitro fertilization. She’s going through it to ensure that her children won't express the gene for hypertrophic cardiomyopathy.
Researchers have found that a mindfulness-based therapy, including savoring natural rewards, can help patients with chronic pain and opioid addiction.
More than 20 percent of American adults suffer from chronic pain. And as many as one in four of those prescribed opioids to manage that pain go on to misuse – or abuse – them, often with devastating consequences. Patients afflicted by both chronic pain and opioid addiction are especially difficult to treat, according to Eric Garland, PhD, Director of the University of Utah’s Center on Mindfulness and Integrative Health Intervention Development, because opioid overuse increases pain sensitivity, and pain promotes relapse among those being treated for addiction.
A new study, however, shows that a mindfulness-based therapy can successfully tackle both problems at once, pointing to a tool that could potentially help in fighting the opioid crisis. “This is the first large-scale clinical trial to show that any psychological intervention can reduce opioid misuse and chronic pain for the long term,” says Garland, lead author of the study, published February 28th in JAMA Internal Medicine.
Garland’s study focused on 250 adults who had received opioid therapy for chronic pain for 90 days or longer, randomly assigning them to eight weeks of either a standard psychotherapy support group or Mindfulness-Oriented Recovery Enhancement (MORE) therapy, which combines mindfulness training, cognitive-behavioral therapy (CBT) and positive psychology. Nine months after getting these treatments in primary care settings, 45 percent of patients in the MORE group were no longer misusing opioids, compared to 24 percent of those in group therapy. In fact, about a third of the patients in the MORE group were able to cut their opioid dose in half or reduce it even further.
Patients treated with MORE also experienced more significant pain relief than those in support groups, according to Garland. Conventional approaches to treating opioid addiction include 12-step programs and medically-assisted treatment using drugs like methadone and Suboxone, sometimes coupled with support groups. But patients with Opioid Use Disorder (OUD) – the official diagnosis for opioid addiction – have high relapse rates following treatment, especially if they have chronic pain.
While medically-assisted treatments help to control drug cravings, they do nothing to control chronic pain, which is where psychological therapies like MORE come in.
“For patients suffering from moderate pain and OUD, the relapse rate is three times higher than in patients without chronic pain; for those with severe chronic pain, the relapse rate is five times higher,” says Amy Wachholtz, PhD, Director of Clinical Health Psychology and associate professor at University of Colorado in Denver. “So if we don’t treat the chronic pain along with the OUD addiction simultaneously, we are setting patients up for failure.”
Unfortunately, notes Garland, the standard of care for patients with chronic pain who are misusing their prescribed painkillers is “woefully inadequate.” Many patients don’t meet the criteria for OUD, he says, but instead fall into a gray zone somewhere between legitimate opioid use and full-blown addiction. And while medically-assisted treatments help to control drug cravings, they do nothing to control chronic pain, which is where psychological therapies like MORE come in. But behavioral therapies are often not available in primary care settings, and even when clinicians do refer patients to behavioral health providers, they often prescribe CBT. A large scale study last year showed that CBT – without the added components of mindfulness training and positive psychology – reduced pain but not opioid misuse.

Psychotherapist Eric Garland teaches mindfulness.
University of Utah
Reward Circuitry Rewired
Opioids are highly physiologically addictive. Repeated and high-dose drug use causes the brain to become hypersensitive to stress, pain, and drug-related cues, such as the sight of one’s pill bottle, says Garland, while at the same time becoming increasingly insensitive to natural pleasures. “As an individual becomes more and more dependent on the opioids just to feel okay, they feel less able to extract a healthy sense of joy, pleasure and meaning out of everyday life,” he explains. “This drives them to take higher and higher doses of the opioid to maintain a dwindling sense of well-being.”
The changes are not just psychological: Chronic opioid use actually causes changes in the brain’s reward circuitry. “You can see on brain imaging,” says Garland. “The brain’s reward circuitry becomes more responsive when a person is viewing opioid related images than when they are viewing images of smiling babies, lovers holding hands, or sunsets over the beach.” MORE, he says, teaches “savoring” – a tenet of positive psychology – as a means of restructuring the reward processes in the brain so the patient becomes sensitive to pleasure from natural, healthy rewards, decreasing cravings for drug-related rewards.
Mindfulness and Addiction
Mindfulness, a form of meditation that teaches people to observe their feelings and sensations without judgement, has been increasingly applied to the treatment of addiction. By observing their pain and cravings objectively, for example, patients gain increased awareness of their responses to pain and their habits of opioid use. “They learn how to be with discomfort, whether emotional or physical, in a more compassionate way,” says Sarah Bowen, PhD, associate professor of psychology at Pacific University in Oregon. “And if your mind gives you a message like ‘Oh, I can’t handle that,’ to recognize that that’s a thought that might not be true.”
Bowen’s research is focused on Mindfulness-Based Relapse Prevention, which addresses the cravings associated with addiction. She has patients practice what she calls “urge surfing”: riding out a craving or urge rather than relying on a substance for immediate relief. “Craving will happen, so rather than fighting it, we look at understanding it better,” she says.
MORE differs from other forms of mindfulness-based therapy in that it integrates reappraisal and savoring training. Reappraisal is a technique often used in CBT in which patients learn to change negative thought patterns in order to reduce their emotional impact, while savoring helps to restructure the reward processes in the brain.
Mindfulness training not only helps patients to understand and gain control over their behavior in response to cravings and triggers like pain, says Garland, but also provides a means of pain relief. “We use mindfulness to zoom into pain and break it down into its subcomponents – feelings of heat or tightness or tingling – which reduces the impact that negative emotions have on pain processing in the brain.”

Eric Garland examines brain waves.
University of Utah
Powerful interventions
As the dangers of opioid addiction have become increasingly evident, some scientists are developing less addictive, non-opioid painkillers, but more trials are needed. Meanwhile, behavioral approaches to chronic pain relief have continued to gain traction, and researchers like Garland are probing the possibilities of integrative treatments to treat the addiction itself. Given that the number of people suffering from chronic pain and OUD have reached new heights during the COVID-19 pandemic, says Wachholtz, new treatment alternatives for patients caught in the relentless cycle of chronic pain and opioid misuse are sorely needed. “We’re trying to refine the techniques,” she says, “but we’re starting to realize just how powerful some of these mind-body interventions can be.”

