After a Diagnosis, Patients Are Finding Solace—and Empowerment—in a Sensitive Corner of Social Media

Katherine Leon and her dog enjoy nice weather in their backyard in Virginia. Leon went from feeling like she was "wandering in the woods" with doctors who hadn't experienced her spontaneous coronary artery dissection, or SCAD, to starting the world's largest registry for research on the condition.
When Kimberly Richardson of Chicago underwent chemotherapy in 2013 for ovarian cancer, her hip began to hurt. Her doctor assigned six months of physical therapy, but the pain persisted.
She took the mystery to Facebook, where she got 200 comments from cancer survivors all pointing to the same solution: Claritin. Two days after starting the antihistamine, her hip felt fine. Claritin, it turns out, reduces bone marrow swelling, a side effect of a stimulant given after chemo.
Richardson isn't alone in using social media for health. Thirty-six percent of adults with chronic diseases have benefited from health advice on the internet, or know others who have. The trend has likely accelerated during COVID-19. "With increases in anxiety and loneliness, patients find comfort in peer support," said Chris Renfro-Wallace, the chief operating officer of PatientsLikeMe, a popular online community.
Sites like PatientsLikeMe and several others are giving rise to a patient-centered view of healthcare, challenging the idea that MD stands for medical deity. They're engaging people in new ways, such as virtual clinical trials. But with misinformation spreading online about health issues, including COVID-19, there's also reason for caution.
Engaged by Design
Following her diagnosis at age 50, Richardson searched the Web. "All I saw were infographics saying in five years I'd be dead."
Eventually, she found her Facebook groups and a site called Inspire, where she met others with her rare granulosa cell tumor. "You get 15 minutes with your doctor, but on social media you can keep posting until you satisfy your question."
Virtual communities may be especially helpful for people with rarely diagnosed diseases, who wouldn't otherwise meet. When Katherine Leon of Virginia suffered chest pain after the birth of her second son, doctors said it was spontaneous coronary artery dissection, or SCAD, involving a torn artery. But she had no risk factors for heart disease. Feeling like she was "wandering in the woods" with doctors who hadn't experienced her situation, she searched online and stumbled on communities like Inspire with members who had. The experience led her to start her own Alliance and the world's largest registry for advancing research on SCAD.
"Inspire is really an extension of yourself," she said. If designed well, online sites can foster what psychologist Keith Sawyer called group mind, a dynamic where participants balance their own voices with listening to others, maximizing community engagement in health. To achieve it, participants must have what Sawyer called a "blending of egos," which may be fostered when sites let users post anonymously. They must also share goals and open communication. The latter priority has driven Brian Loew, Inspire's CEO, to safeguard the privacy of health information exchanged on the site, often asking himself, "Would I be okay if a family member had this experience?"
The vibe isn't so familial on some of Facebook's health-focused groups. There, people might sense marketers and insurers peering over their shoulders. In 2018, a researcher discovered that companies could exploit personal information on a private Facebook community for BRCA-positive women. Members of the group started a nonprofit, the Light Collective, to help peer-to-peer support platforms improve their transparency.
PatientsLikeMe and Inspire nurture the shared experience by hosting pages on scores of diseases, allowing people to better understand treatment options for multiple conditions—and find others facing the same set of issues. Four in ten American adults have more than one chronic disease.
Sawyer observed that groups are further engaged when there's a baseline of common knowledge. To that end, some platforms take care in structuring dialogues among members to promote high-quality information, stepping in to moderate when necessary. On Inspire, members get emails when others reply to their posts, instead of instant messaging. The communication lag allows staff to notice misinformation and correct it. Facebook conversations occur in real-time among many more people; "moderation is almost impossible," said Leon.
Even on PatientsLikeMe and Inspire, deciding which content to police can be tough, as variations across individuals may result in conflicting but equally valid posts. Leon's left main artery was 90 percent blocked, requiring open heart surgery, whereas others with SCAD have angina, warranting a different approach. "It's a real range of experience," she explained. "That's probably the biggest challenge: supporting everyone where they are."
Critically, these sites don't treat illnesses. "If a member asks a medical question, we typically tell them to go to their doctor," said Loew, the Inspire CEO.
Increasingly, it may be the other way around.
The Patient Will See You Now
"Some doctors embrace the idea of an educated patient," said Loew. "The more information, the better." Others, he said, aren't thrilled about patients learning on their own.
"Doctors were behind the eight ball," said Shikha Jain, an oncologist in Chicago. "We were encouraged for years to avoid social media due to patient privacy issues. There's been a drastic shift in the last few years."
Jain recently co-founded IMPACT, a grassroots organization that networks with healthcare workers across Illinois for greater awareness of health issues. She thinks doctors must meet patients where they are—increasingly, online—and learn about the various platforms where patients connect. Doctors can then suggest credible online sources for their patients' conditions. Learning about different sites takes time, Jain said, "but that's the nature of being a physician in this day and age."
At stake is the efficiency of doctor-patient interactions. "I like when patients bring in research," Jain said. "It opens up the dialogue and lets them inform the decision-making process." Richardson, the cancer survivor, agreed. "We shouldn't make the physician the villain in this conversation." Interviewed over Zoom, she was engaging but quick to challenge the assumptions behind some questions; her toughness was palpable, molded by years of fighting disease—and the healthcare system. Many doctors are forced by that system into faster office visits, she said. "If patients help their doctor get to the heart of the issue in a shorter time, now we're going down a narrower road of tests."
These conversations could be enhanced by PatientsLikeMe's Doctor Visit Guide. It uses algorithms to consolidate health data that members track on the site into a short report they can share with their physicians. "It gives the doctor a richer data set to really see how a person has been doing," said Renfro-Wallace.
Doctors aren't the only ones benefiting from these sites.
Who Profits?
A few platforms like Inspire make money by connecting their members to drug companies, so they can participate in the companies' clinical trials to test out new therapies. A cynic might say the sites are just fronts for promoting the pharmaceuticals.
The need is real, though, as many clinical trials suffer from low participation, and the experimental treatments can improve health. The key for Loew, Inspire's CEO, is being transparent about his revenue model. "When you sign up, we assume you didn't read the fine print [in the terms of agreement]." So, when Inspire tells members about openings in trials, it's a reminder the site works with pharma.
"When I was first on Inspire, all of that was invisible to me," said Leon. "It didn't dawn on me for years." Richardson believes many don't notice pharma's involvement because they're preoccupied by their medical issues.
One way Inspire builds trust is by partnering with patient advocacy groups, which tend to be nonprofit and science-oriented, said Craig Lipset, the former head of clinical innovation for Pfizer. When he developed a rare lung disease, he joined the board of a foundation that partners with Inspire's platform. The section dedicated to his disease is emblazoned with his foundation's logo and colors. Contrast that with other sites that build communities at the direct behest of drug companies, he said.
Insurance companies are also eyeing these communities. Last month, PatientsLikeMe raised $26 million in financing from investors including Optum Ventures, which belongs to the same health care company that owns a leading health insurance company, UnitedHealthcare. PatientsLikeMe is an independent company, though, and data is shared with UnitedHealth only if patients provide consent. The site is using the influx of resources to gamify improvements in health, resembling programs run by UnitedHealth that assign nutrition and fitness "missions," with apps for tracking progress. Soon, PatientsLikeMe will roll out a smarter data tracking system that gives members actionable insights and prompts them to take actions based on their conditions, as well as competitions to motivate healthier behaviors.
Such as a race to vaccinate, perhaps.
Dealing with Misinformation
An advantage of health-focused communities is the intimacy of their gatherings, compared to behemoths like Facebook. Loew, Inspire's head, is mindful of Dunbar's rule: humans can manage only about 150 friends. Inspire's social network mapping suggests many connections among members, but of different strength; Loew hopes to keep his site's familial ambiance even while expanding membership. Renfro-Wallace is exploring video and voice-only meetings to enrich the shared experiences on PatientsLikeMe, while respecting members' privacy.
But a main driver of growth and engagement online is appealing to emotion rather than reason; witness Facebook during the pandemic. "We know that misinformation and scary things spread far more rapidly than something positive," said Ann Lewandowski, the executive director of Wisconsin Immunization Neighborhood, a coalition of health providers and associations countering vaccine hesitancy across the state.
"Facebook's moderation mechanism is terrible," she said. Vaccine advocates in her region who try to flag misinformation on Facebook often have their content removed because the site's algorithm associates their posts with the distortions they're trying to warn people about.
In the realm of health, where accessing facts can mean life or death—and where ad-based revenue models conflict with privacy needs—there's probably a ceiling on how large social media sites should scale. Loew views Inspire as co-existing, not competing with Facebook.
Propagandists had months to perfect campaigns to dissuade people from mRNA vaccines. But even Lewandowski's doctor was misinformed about vaccine side effects for her condition, multiple sclerosis. She sees potential for health-focused sites to convene more virtual forums, in which patient advocacy groups educate doctors and patients on vaccine safety.
Inspire is raising awareness about COVID vaccines through a member survey with an interactive data visualization. Sampling thousands of members, the survey found vaccines are tolerated well among patients with cancer, autoimmune issues, and other serious conditions. Analytics for online groups are evolving quickly, said Lipset. "Think about the acceleration in research when you take the emerging capability for aggregating health data and mash it up with patients engaged in sharing."
Lipset recently co-founded the Decentralized Trials and Research Alliance to accelerate clinical trials and make them more accessible to patients—even from home, without risking the virus. Sites like PatientsLikeMe share this commitment, collaborating with Duke's ALS Clinic to let patients join a trial from home with just two clinic visits. Synthetic control groups were created by PatientsLikeMe's algorithms, eliminating the need for a placebo arm, enabling faster results.
As for Richardson, the ovarian cancer patient, being online has given her another type of access—to experts. She was diagnosed this year with breast cancer. "This time is totally different," she said. On Twitter, she's been direct messaging cancer researchers, whose replies have informed her disease-management strategy. When her oncologists prescribed 33 radiation treatments, she counter-proposed upping the dosage over fewer treatments. Her doctors agreed, cutting unnecessary trips from home. "I'm immuno-compromised," she said. "It's like Russian roulette. You're crossing your finger you won't get the virus."
After years of sticking up for her own health, Richardson is now positioned to look out for others. She collaborated with the University of Illinois Cancer Center on a training module that lets patients take control of their health. She's sharing it online, in a virtual community near you. "It helps you make intelligent decisions," she said. "When you speak your physician's language, it shifts the power in the room."
If approved by the FDA, a new procedure for kidney transplants that doesn't require anti-rejection medication could soon become the standard of care.
Talaris Therapeutics, Inc., a biotech company based in Louisville, Ky., is edging closer to eradicating the need for immunosuppressive drugs for kidney transplant patients.
In a series of research trials, Talaris is infusing patients with immune system stem cells from their kidney donor to create a donor-derived immune system that accepts the organ without the need for anti-rejection medications. That newly generated system does not attack other parts of the recipient’s body and also fights off infections and diseases as a healthy immune system would.
Talaris is now moving into the final clinical trial, phase III, before submitting for FDA approval. Known as Freedom-1, this trial has 17 sites open throughout the U.S., and Talaris will enroll a total of 120 kidney transplant recipients. One day after receiving their donor’s kidney, 80 people will undergo the company’s therapy, involving the donor’s stem cells and other critical cells that are processed at their facility. Forty will have a regular kidney transplant and remain on immunosuppression to provide a control group.
“The beauty of this procedure is that I don’t have to take all of the anti-rejection drugs,” says Robert Waddell, a finance professional. “I forget that I ever had any kidney issues. That’s how impactful it is.”
The procedure was pioneered decades ago by Suzanne Ildstad as a faculty member at the University of Pittsburgh before she became founding CEO of Talaris and then its Chief Scientific Officer. If approved by the FDA, the method could soon become the standard of care for patients in need of a kidney transplant.
“We are working to find a way to reprogram the immune system of transplant recipients so that it sees the donated organ as [belonging to one]self and doesn’t attack it,” explains Scott Requadt, CEO of Talaris. “That obviates the need for lifelong immunosuppression.”
Each year, there are roughly 20,000 kidney transplants, making kidneys the most transplanted organ. About 6,500 of those come from living donors, while deceased donors provide roughly 13,000.
One of the challenges, Requadt points out, is that kidney transplant recipients aren’t always aware of all the implications of immunosuppression. Typically, they will need to take about 20 anti-rejection drugs several times a day to provide immunosuppression as well as treat complications caused by the toxicities of immunosuppression medications. The side effects of chronic immunosuppression include weight gain, high blood pressure, and high cholesterol. These cardiovascular comorbidities, Requadt says, are “often more frequently the cause of death than failure of a transplanted organ.”
Patients who are chronically immunosuppressed generally have much higher rates of infections and cancers that have an immune component to them, such as skin cancers.
For the past couple of years, those patients have experienced heightened anxiety because of the COVID-19 pandemic. Immune-suppressing medicine used to protect their new organ also makes it hard for patients to build immunity to foreign invaders like COVID-19.
A study appearing in the Proceedings of the National Academy of Sciences found the probability of a pandemic with similar impact to COVID-19 is about 2 percent in any year, and estimated that the probability of novel disease outbreaks will grow three-fold in the next few decades. All the more reason to identify an FDA-approved alternative to harsh immunosuppressive drugs.
Of the 18 patients during the phase II research trial who received the Talaris therapy, didn’t take immunosuppression medication and were vaccinated, only two ended up with a COVID infection, according to a review of the data. Among patients who needed to continue taking immunosuppressants or those who didn’t have them but were unvaccinated, the rates of infection were between 40 and 60 percent.
In the earlier phase II study by Talaris with 37 patients, the combined transplantation approach allowed 70 percent of patients to get off all immunosuppression.
“We’ve followed that whole cohort for more than six and a half years and one of them for 12 years from transplant, and every single patient that we got off immunosuppression has been able to stay off,” Requadt says.
That one patient, Robert Waddell, 55, was especially thankful to be weaned off immunosuppressive drugs approximately one year after his transplant procedure. The Louisville resident had long watched his mother, sister and other family members with polycystic kidney disease, or PKD, suffer the effects of chronic immunosuppression. That became his greatest fear when he was diagnosed with end stage renal failure.
Waddell enrolled in the phase II research taking place in Louisville after learning about it in early 2006. He chose to remain in the study when it relocated its clinical headquarters to Northwestern University’s medical center in Chicago a couple years later.
Before surgery, he underwent an enervating regimen of chemotherapy and radiation. It’s required to clear out a patient’s bone marrow cells so that they can be replaced by the donor’s cells. Waddell says the result was worth it: he had his combined kidney and immune system stem cell transplant in May 2009, without any need for chronic immunosuppression.
“I call it ‘short-term pain, long-term gain,’ because it was difficult to go through the conditioning, but after that, it was great,” he says. “I’ve talked to so many kidney recipients who say, ‘I wish I would have done that,’ because most people don’t think about clinical trials, but I was very fortunate.”
Waddell has every reason to support the success of this research, especially given the genetic disorder, PKD, that has plagued his family. One of his four children has PKD. He is anxious for the procedure to become standard of care, if and when his son needs it.

The Talaris procedure was pioneered decades ago by Suzanne Ildstad, founding CEO of Talaris and the company's Chief Scientific Officer, pictured here with the current CEO, Scott Requadt.
Talaris
“The beauty of this procedure is that I don’t have to take all of the anti-rejection drugs,” says Waddell, a finance professional. “I forget that I ever had any kidney issues. That’s how impactful it is.”
Talaris will continue to follow Waddell and the rest of his cohort to track the effectiveness and safety of the procedure. According to Requadt, the average life of a transplanted kidney is 12 to 15 years, partly because the immunosuppressive drugs worsen the functioning of the organ each year.
“We were the first group to show that we could robustly and fairly reproducibly do this in a clinical setting in humans,” Requadt says. “Most important, we’ve been able to show that we can still get a good engraftment of the stem cells from the donor, even if there is a profound…mismatch between the donor and the recipient’s immune systems.”
In kidney transplantation, it’s important to match for human leukocyte antigens (HLA) because there is a better graft survival in HLA-identical kidney transplants compared with HLA mismatched transplants.
About three months after the transplant, Talaris researchers look for evidence that the donated immune cells and stem cells have engrafted, while making a donor immune system for the patient. If more than 50 percent of the T cells contain the donor’s DNA after six months, patients can start taking fewer immunosuppressants.
“We know from phase II that in our patients who were able to tolerize [accept the organ without rejection] to their donated organ, we saw completely preserved and in fact slightly increased kidney function,” Requadt says. “So, it stands to reason that if you eliminate the drugs that are associated with declining kidney function that you would preserve kidney function, so hopefully the patient will have that one kidney for life.”
Matthew Cooper, director of kidney and pancreas transplantation for MedStar Georgetown Transplant Institute in Washington, DC, states that, “Right now, the Achilles’ heel is we have such a long waiting list and few donors that people die every day waiting for a kidney transplant. Eventually, we will eliminate the organ shortage so that people won’t die from organ failure.”
Cooper, a nationally recognized clinical transplant surgeon for 20 years, says when he started his career, finding a way for patients to forgo immunosuppression was considered “the Holy Grail” of modern transplant medicine.
“Now that we’ve got the protocols in place and some personal examples of how that can happen, it’s pretty exciting to see that all coming together,” he adds.
Researchers advance drugs that treat pain without addiction
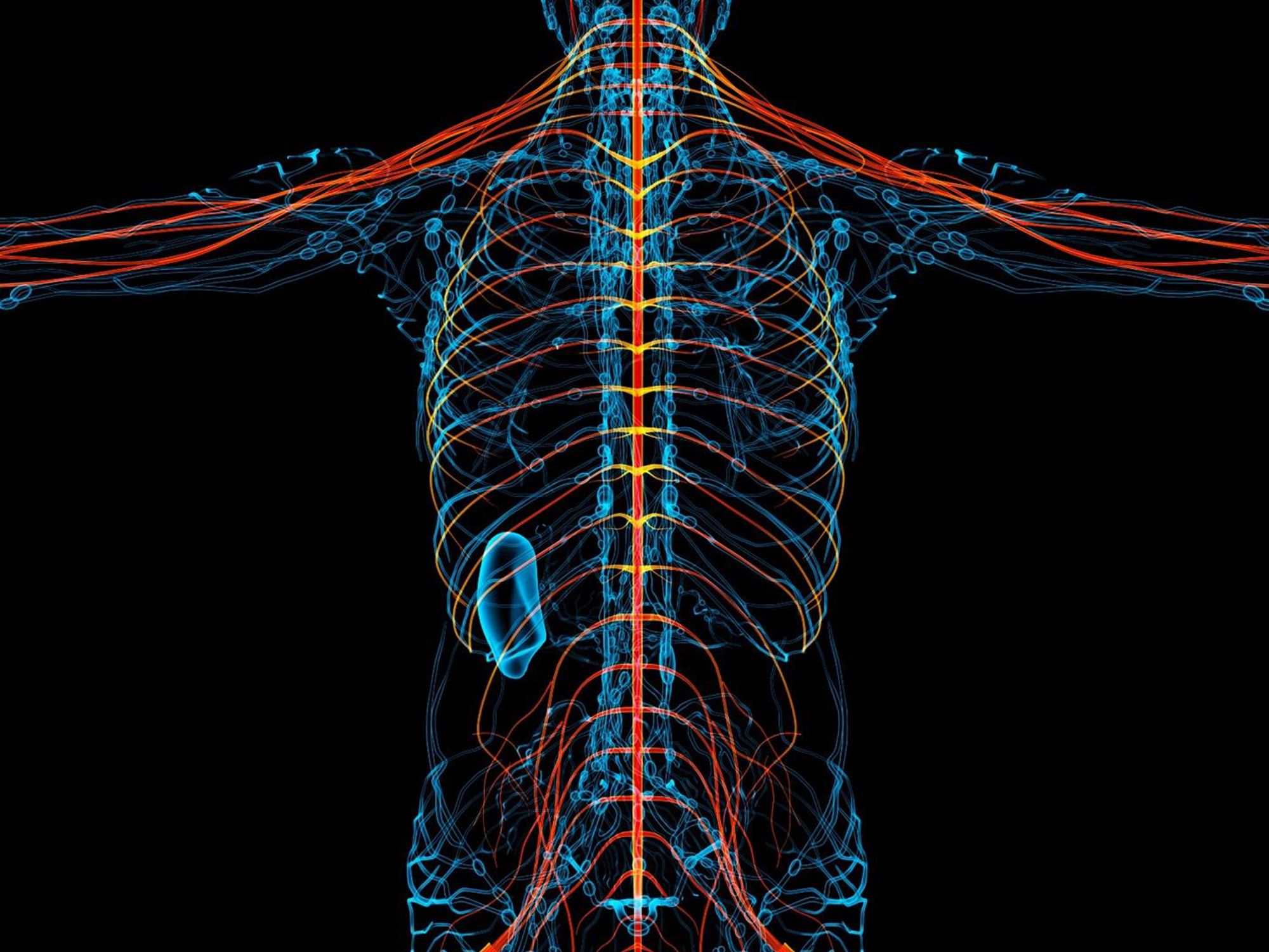
New therapies are using creative approaches that target the body’s sensory neurons, which send pain signals to the brain.
Opioids are one of the most common ways to treat pain. They can be effective but are also highly addictive, an issue that has fueled the ongoing opioid crisis. In 2020, an estimated 2.3 million Americans were dependent on prescription opioids.
Opioids bind to receptors at the end of nerve cells in the brain and body to prevent pain signals. In the process, they trigger endorphins, so the brain constantly craves more. There is a huge risk of addiction in patients using opioids for chronic long-term pain. Even patients using the drugs for acute short-term pain can become dependent on them.
Scientists have been looking for non-addictive drugs to target pain for over 30 years, but their attempts have been largely ineffective. “We desperately need alternatives for pain management,” says Stephen E. Nadeau, a professor of neurology at the University of Florida.
A “dimmer switch” for pain
Paul Blum is a professor of biological sciences at the University of Nebraska. He and his team at Neurocarrus have created a drug called N-001 for acute short-term pain. N-001 is made up of specially engineered bacterial proteins that target the body’s sensory neurons, which send pain signals to the brain. The proteins in N-001 turn down pain signals, but they’re too large to cross the blood-brain barrier, so they don’t trigger the release of endorphins. There is no chance of addiction.
When sensory neurons detect pain, they become overactive and send pain signals to the brain. “We wanted a way to tone down sensory neurons but not turn them off completely,” Blum reveals. The proteins in N-001 act “like a dimmer switch, and that's key because pain is sensation overstimulated.”
Blum spent six years developing the drug. He finally managed to identify two proteins that form what’s called a C2C complex that changes the structure of a subunit of axons, the parts of neurons that transmit electrical signals of pain. Changing the structure reduces pain signaling.
“It will be a long path to get to a successful clinical trial in humans," says Stephen E. Nadeau, professor of neurology at the University of Florida. "But it presents a very novel approach to pain reduction.”
Blum is currently focusing on pain after knee and ankle surgery. Typically, patients are treated with anesthetics for a short time after surgery. But anesthetics usually only last for 4 to 6 hours, and long-term use is toxic. For some, the pain subsides. Others continue to suffer after the anesthetics have worn off and start taking opioids.
N-001 numbs sensation. It lasts for up to 7 days, much longer than any anesthetic. “Our goal is to prolong the time before patients have to start opioids,” Blum says. “The hope is that they can switch from an anesthetic to our drug and thereby decrease the likelihood they're going to take the opioid in the first place.”
Their latest animal trial showed promising results. In mice, N-001 reduced pain-like behaviour by 90 percent compared to the control group. One dose became effective in two hours and lasted a week. A high dose had pain-relieving effects similar to an opioid.
Professor Stephen P. Cohen, director of pain operations at John Hopkins, believes the Neurocarrus approach has potential but highlights the need to go beyond animal testing. “While I think it's promising, it's an uphill battle,” he says. “They have shown some efficacy comparable to opioids, but animal studies don't translate well to people.”
Nadeau, the University of Florida neurologist, agrees. “It will be a long path to get to a successful clinical trial in humans. But it presents a very novel approach to pain reduction.”
Blum is now awaiting approval for phase I clinical trials for acute pain. He also hopes to start testing the drug's effect on chronic pain.
Learning from people who feel no pain
Like Blum, a pharmaceutical company called Vertex is focusing on treating acute pain after surgery. But they’re doing this in a different way, by targeting a sodium channel that plays a critical role in transmitting pain signals.
In 2004, Stephen Waxman, a neurology professor at Yale, led a search for genetic pain anomalies and found that biologically related people who felt no pain despite fractures, burns and even childbirth had mutations in the Nav1.7 sodium channel. Further studies in other families who experienced no pain showed similar mutations in the Nav1.8 sodium channel.
Scientists set out to modify these channels. Many unsuccessful efforts followed, but Vertex has now developed VX-548, a medicine to inhibit Nav1.8. Typically, sodium ions flow through sodium channels to generate rapid changes in voltage which create electrical pulses. When pain is detected, these pulses in the Nav1.8 channel transmit pain signals. VX-548 uses small molecules to inhibit the channel from opening. This blocks the flow of sodium ions and the pain signal. Because Nav1.8 operates only in peripheral nerves, located outside the brain, VX-548 can relieve pain without any risk of addiction.
"Frankly we need drugs for chronic pain more than acute pain," says Waxman.
The team just finished phase II clinical trials for patients following abdominoplasty surgery and bunionectomy surgery.
After abdominoplasty surgery, 76 patients were treated with a high dose of VX-548. Researchers then measured its effectiveness in reducing pain over 48 hours, using the SPID48 scale, in which higher scores are desirable. The score for Vertex’s drug was 110.5 compared to 72.7 in the placebo group, whereas the score for patients taking an opioid was 85.2. The study involving bunionectomy surgery showed positive results as well.
Waxman, who has been at the forefront of studies into Nav1.7 and Nav1.8, believes that Vertex's results are promising, though he highlights the need for further clinical trials.
“Blocking Nav1.8 is an attractive target,” he says. “[Vertex is] studying pain that is relatively simple and uniform, and that's key to having a drug trial that is informative. But the study needs to be replicated and frankly we need drugs for chronic pain more than acute pain. If this is borne out by additional studies, it's one important step in a journey.”
Vertex will be launching phase III trials later this year.
Finding just the right amount of Nerve Growth Factor
Whereas Neurocarrus and Vertex are targeting short-term pain, a company called Levicept is concentrating on relieving chronic osteoarthritis pain. Around 32.5 million Americans suffer from osteoarthritis. Patients commonly take NSAIDs, or non-steroidal anti-inflammatory drugs, but they cannot be taken long-term. Some take opioids but they aren't very effective.
Levicept’s drug, Levi-04, is designed to modify a signaling pathway associated with pain. Nerve Growth Factor (NGF) is a neurotrophin: it’s involved in nerve growth and function. NGF signals by attaching to receptors. In pain there are excess neurotrophins attaching to receptors and activating pain signals.
“What Levi-04 does is it returns the natural equilibrium of neurotrophins,” says Simon Westbrook, the CEO and founder of Levicept. It stabilizes excess neurotrophins so that the NGF pathway does not signal pain. Levi-04 isn't addictive since it works within joints and in nerves outside the brain.
Westbrook was initially involved in creating an anti-NGF molecule for Pfizer called Tanezumab. At first, Tanezumab seemed effective in clinical trials and other companies even started developing their own versions. However, a problem emerged. Tanezumab caused rapidly progressive osteoarthritis, or RPOA, in some patients because it completely removed NGF from the system. NGF is not just involved in pain signalling, it’s also involved in bone growth and maintenance.
Levicept has found a way to modify the NGF pathway without completely removing NGF. They have now finished a small-scale phase I trial mainly designed to test safety rather than efficacy. “We demonstrated that Levi-04 is safe and that it bound to its target, NGF,” says Westbrook. It has not caused RPOA.
Professor Philip Conaghan, director of the Leeds Institute of Rheumatic and Musculoskeletal Medicine, believes that Levi-04 has potential but urges the need for caution. “At this early stage of development, their molecule looks promising for osteoarthritis pain,” he says. “They will have to watch out for RPOA which is a potential problem.”
Westbrook starts phase II trials with 500 patients this summer to check for potential side effects and test the drug’s efficacy.
There is a real push to find an effective alternative to opioids. “We have a lot of work to do,” says Professor Waxman. “But I am confident that we will be able to develop new, much more effective pain therapies.”