After a Diagnosis, Patients Are Finding Solace—and Empowerment—in a Sensitive Corner of Social Media

Katherine Leon and her dog enjoy nice weather in their backyard in Virginia. Leon went from feeling like she was "wandering in the woods" with doctors who hadn't experienced her spontaneous coronary artery dissection, or SCAD, to starting the world's largest registry for research on the condition.
When Kimberly Richardson of Chicago underwent chemotherapy in 2013 for ovarian cancer, her hip began to hurt. Her doctor assigned six months of physical therapy, but the pain persisted.
She took the mystery to Facebook, where she got 200 comments from cancer survivors all pointing to the same solution: Claritin. Two days after starting the antihistamine, her hip felt fine. Claritin, it turns out, reduces bone marrow swelling, a side effect of a stimulant given after chemo.
Richardson isn't alone in using social media for health. Thirty-six percent of adults with chronic diseases have benefited from health advice on the internet, or know others who have. The trend has likely accelerated during COVID-19. "With increases in anxiety and loneliness, patients find comfort in peer support," said Chris Renfro-Wallace, the chief operating officer of PatientsLikeMe, a popular online community.
Sites like PatientsLikeMe and several others are giving rise to a patient-centered view of healthcare, challenging the idea that MD stands for medical deity. They're engaging people in new ways, such as virtual clinical trials. But with misinformation spreading online about health issues, including COVID-19, there's also reason for caution.
Engaged by Design
Following her diagnosis at age 50, Richardson searched the Web. "All I saw were infographics saying in five years I'd be dead."
Eventually, she found her Facebook groups and a site called Inspire, where she met others with her rare granulosa cell tumor. "You get 15 minutes with your doctor, but on social media you can keep posting until you satisfy your question."
Virtual communities may be especially helpful for people with rarely diagnosed diseases, who wouldn't otherwise meet. When Katherine Leon of Virginia suffered chest pain after the birth of her second son, doctors said it was spontaneous coronary artery dissection, or SCAD, involving a torn artery. But she had no risk factors for heart disease. Feeling like she was "wandering in the woods" with doctors who hadn't experienced her situation, she searched online and stumbled on communities like Inspire with members who had. The experience led her to start her own Alliance and the world's largest registry for advancing research on SCAD.
"Inspire is really an extension of yourself," she said. If designed well, online sites can foster what psychologist Keith Sawyer called group mind, a dynamic where participants balance their own voices with listening to others, maximizing community engagement in health. To achieve it, participants must have what Sawyer called a "blending of egos," which may be fostered when sites let users post anonymously. They must also share goals and open communication. The latter priority has driven Brian Loew, Inspire's CEO, to safeguard the privacy of health information exchanged on the site, often asking himself, "Would I be okay if a family member had this experience?"
The vibe isn't so familial on some of Facebook's health-focused groups. There, people might sense marketers and insurers peering over their shoulders. In 2018, a researcher discovered that companies could exploit personal information on a private Facebook community for BRCA-positive women. Members of the group started a nonprofit, the Light Collective, to help peer-to-peer support platforms improve their transparency.
PatientsLikeMe and Inspire nurture the shared experience by hosting pages on scores of diseases, allowing people to better understand treatment options for multiple conditions—and find others facing the same set of issues. Four in ten American adults have more than one chronic disease.
Sawyer observed that groups are further engaged when there's a baseline of common knowledge. To that end, some platforms take care in structuring dialogues among members to promote high-quality information, stepping in to moderate when necessary. On Inspire, members get emails when others reply to their posts, instead of instant messaging. The communication lag allows staff to notice misinformation and correct it. Facebook conversations occur in real-time among many more people; "moderation is almost impossible," said Leon.
Even on PatientsLikeMe and Inspire, deciding which content to police can be tough, as variations across individuals may result in conflicting but equally valid posts. Leon's left main artery was 90 percent blocked, requiring open heart surgery, whereas others with SCAD have angina, warranting a different approach. "It's a real range of experience," she explained. "That's probably the biggest challenge: supporting everyone where they are."
Critically, these sites don't treat illnesses. "If a member asks a medical question, we typically tell them to go to their doctor," said Loew, the Inspire CEO.
Increasingly, it may be the other way around.
The Patient Will See You Now
"Some doctors embrace the idea of an educated patient," said Loew. "The more information, the better." Others, he said, aren't thrilled about patients learning on their own.
"Doctors were behind the eight ball," said Shikha Jain, an oncologist in Chicago. "We were encouraged for years to avoid social media due to patient privacy issues. There's been a drastic shift in the last few years."
Jain recently co-founded IMPACT, a grassroots organization that networks with healthcare workers across Illinois for greater awareness of health issues. She thinks doctors must meet patients where they are—increasingly, online—and learn about the various platforms where patients connect. Doctors can then suggest credible online sources for their patients' conditions. Learning about different sites takes time, Jain said, "but that's the nature of being a physician in this day and age."
At stake is the efficiency of doctor-patient interactions. "I like when patients bring in research," Jain said. "It opens up the dialogue and lets them inform the decision-making process." Richardson, the cancer survivor, agreed. "We shouldn't make the physician the villain in this conversation." Interviewed over Zoom, she was engaging but quick to challenge the assumptions behind some questions; her toughness was palpable, molded by years of fighting disease—and the healthcare system. Many doctors are forced by that system into faster office visits, she said. "If patients help their doctor get to the heart of the issue in a shorter time, now we're going down a narrower road of tests."
These conversations could be enhanced by PatientsLikeMe's Doctor Visit Guide. It uses algorithms to consolidate health data that members track on the site into a short report they can share with their physicians. "It gives the doctor a richer data set to really see how a person has been doing," said Renfro-Wallace.
Doctors aren't the only ones benefiting from these sites.
Who Profits?
A few platforms like Inspire make money by connecting their members to drug companies, so they can participate in the companies' clinical trials to test out new therapies. A cynic might say the sites are just fronts for promoting the pharmaceuticals.
The need is real, though, as many clinical trials suffer from low participation, and the experimental treatments can improve health. The key for Loew, Inspire's CEO, is being transparent about his revenue model. "When you sign up, we assume you didn't read the fine print [in the terms of agreement]." So, when Inspire tells members about openings in trials, it's a reminder the site works with pharma.
"When I was first on Inspire, all of that was invisible to me," said Leon. "It didn't dawn on me for years." Richardson believes many don't notice pharma's involvement because they're preoccupied by their medical issues.
One way Inspire builds trust is by partnering with patient advocacy groups, which tend to be nonprofit and science-oriented, said Craig Lipset, the former head of clinical innovation for Pfizer. When he developed a rare lung disease, he joined the board of a foundation that partners with Inspire's platform. The section dedicated to his disease is emblazoned with his foundation's logo and colors. Contrast that with other sites that build communities at the direct behest of drug companies, he said.
Insurance companies are also eyeing these communities. Last month, PatientsLikeMe raised $26 million in financing from investors including Optum Ventures, which belongs to the same health care company that owns a leading health insurance company, UnitedHealthcare. PatientsLikeMe is an independent company, though, and data is shared with UnitedHealth only if patients provide consent. The site is using the influx of resources to gamify improvements in health, resembling programs run by UnitedHealth that assign nutrition and fitness "missions," with apps for tracking progress. Soon, PatientsLikeMe will roll out a smarter data tracking system that gives members actionable insights and prompts them to take actions based on their conditions, as well as competitions to motivate healthier behaviors.
Such as a race to vaccinate, perhaps.
Dealing with Misinformation
An advantage of health-focused communities is the intimacy of their gatherings, compared to behemoths like Facebook. Loew, Inspire's head, is mindful of Dunbar's rule: humans can manage only about 150 friends. Inspire's social network mapping suggests many connections among members, but of different strength; Loew hopes to keep his site's familial ambiance even while expanding membership. Renfro-Wallace is exploring video and voice-only meetings to enrich the shared experiences on PatientsLikeMe, while respecting members' privacy.
But a main driver of growth and engagement online is appealing to emotion rather than reason; witness Facebook during the pandemic. "We know that misinformation and scary things spread far more rapidly than something positive," said Ann Lewandowski, the executive director of Wisconsin Immunization Neighborhood, a coalition of health providers and associations countering vaccine hesitancy across the state.
"Facebook's moderation mechanism is terrible," she said. Vaccine advocates in her region who try to flag misinformation on Facebook often have their content removed because the site's algorithm associates their posts with the distortions they're trying to warn people about.
In the realm of health, where accessing facts can mean life or death—and where ad-based revenue models conflict with privacy needs—there's probably a ceiling on how large social media sites should scale. Loew views Inspire as co-existing, not competing with Facebook.
Propagandists had months to perfect campaigns to dissuade people from mRNA vaccines. But even Lewandowski's doctor was misinformed about vaccine side effects for her condition, multiple sclerosis. She sees potential for health-focused sites to convene more virtual forums, in which patient advocacy groups educate doctors and patients on vaccine safety.
Inspire is raising awareness about COVID vaccines through a member survey with an interactive data visualization. Sampling thousands of members, the survey found vaccines are tolerated well among patients with cancer, autoimmune issues, and other serious conditions. Analytics for online groups are evolving quickly, said Lipset. "Think about the acceleration in research when you take the emerging capability for aggregating health data and mash it up with patients engaged in sharing."
Lipset recently co-founded the Decentralized Trials and Research Alliance to accelerate clinical trials and make them more accessible to patients—even from home, without risking the virus. Sites like PatientsLikeMe share this commitment, collaborating with Duke's ALS Clinic to let patients join a trial from home with just two clinic visits. Synthetic control groups were created by PatientsLikeMe's algorithms, eliminating the need for a placebo arm, enabling faster results.
As for Richardson, the ovarian cancer patient, being online has given her another type of access—to experts. She was diagnosed this year with breast cancer. "This time is totally different," she said. On Twitter, she's been direct messaging cancer researchers, whose replies have informed her disease-management strategy. When her oncologists prescribed 33 radiation treatments, she counter-proposed upping the dosage over fewer treatments. Her doctors agreed, cutting unnecessary trips from home. "I'm immuno-compromised," she said. "It's like Russian roulette. You're crossing your finger you won't get the virus."
After years of sticking up for her own health, Richardson is now positioned to look out for others. She collaborated with the University of Illinois Cancer Center on a training module that lets patients take control of their health. She's sharing it online, in a virtual community near you. "It helps you make intelligent decisions," she said. "When you speak your physician's language, it shifts the power in the room."
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
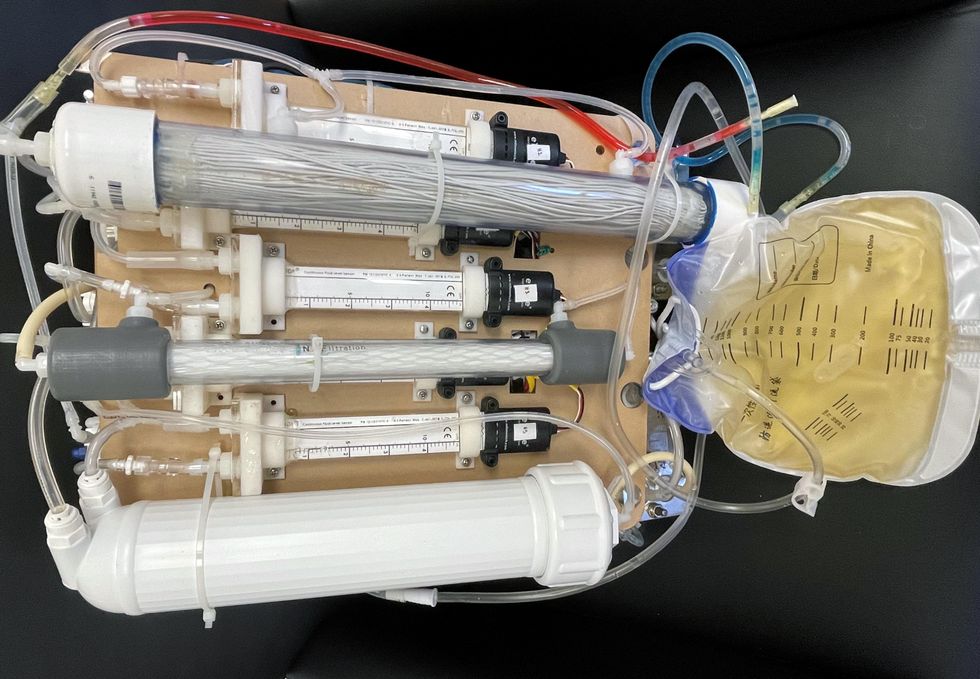
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of them can be useful for depression.
Even before the pandemic created a need for more telehealth options, depression was a hot area of research for app developers. Given the high prevalence of depression and its connection to suicidality — especially among today’s teenagers and young adults who grew up with mobile devices, use them often, and experience these conditions with alarming frequency — apps for depression could be not only useful but lifesaving.
“For people who are not depressed, but have been depressed in the past, the apps can be helpful for maintaining positive thinking and behaviors,” said Andrea K. Wittenborn, PhD, director of the Couple and Family Therapy Doctoral Program and a professor in human development and family studies at Michigan State University. “For people who are mildly to severely depressed, apps can be a useful complement to working with a mental health professional.”
Health and fitness apps, in general, number in the hundreds of thousands. These are driving a market expected to reach $102.45 billion by next year. The mobile mental health app market is a small part of this but still sizable at $500 million, with revenues generated through user health insurance, employers, and direct payments from individuals.
Apps can provide data that health professionals cannot gather on their own. People’s constant interaction with smartphones and wearable devices yields data on many health conditions for millions of patients in their natural environments and while they go about their usual activities. Compared with the in-office measurements of weight and blood pressure and the brevity of doctor-patient interactions, the thousands of data points gathered unobtrusively over an extended time period provide a far better and more detailed picture of the person and their health.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in digital biomarkers that relate to depressive symptoms and other conditions.
Building on three decades of research since early “apps” were used for delivering treatment manuals to health professionals, today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of these apps can be useful for depression.
Some apps primarily provide a virtual connection to a group of mental health professionals employed or contracted by the app. Others have options for meditation, sleeping or, in the case of industry leaders Calm and Headspace, overall well-being. On the cutting edge are apps that detect changes in a person’s use of mobile devices and their interactions with them.
Apps such as AbleTo, Happify Health, and Woebot Health focus on cognitive behavioral therapy, a type of counseling with proven potential to change a person’s behaviors and feelings. “CBT has been demonstrated in innumerable studies over the last several decades to be effective in the treatment of behavioral health conditions such as depression and anxiety disorders,” said Dr. Reena Pande, chief medical officer at AbleTo. “CBT is intended to be delivered as a structured intervention incorporating key elements, including behavioral activation and adaptive thinking strategies.”
These CBT skills help break the negative self-talk (rumination) common in patients with depression. They are taught and reinforced by some self-guided apps, using either artificial intelligence or programmed interactions with users. Apps can address loneliness and isolation through connections with others, even when a symptomatic person doesn’t feel like leaving the house.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in “digital biomarkers” that can be associated with onset or worsening of depressive symptoms and other cognitive conditions. In one study, Mindstrong Health gathered a year’s worth of data on how people use their smartphones, such as scrolling through articles, typing and clicking. Mindstrong, whose founders include former leaders of the National Institutes of Health, modeled the timing and order of these actions to make assessments that correlated closely with gold-standard tests of cognitive function.
National organizations of mental health professionals have been following the expanding number of available apps over the years with keen interest. App Advisor is an initiative of the American Psychiatric Association that helps psychiatrists and other mental health professionals navigate the issues raised by mobile health technology. App Advisor does not rate or recommend particular apps but rather provides guidance about why apps should be assessed and how health professionals can do this.
A website that does review mental health apps is One Mind Psyber Guide, an independent nonprofit that partners with several national organizations. One Mind users can select among numerous search terms for the condition and therapeutic approach of interest. Apps are rated on a five-point scale, with reviews written by professionals in the field.
Do mental health apps related to depression have the kind of safety and effectiveness data required for medications and other medical interventions? Not always — and not often. Yet the overall results have shown early promise, Wittenborn noted.
“Studies that have attempted to detect depression from smartphone and wearable sensors [during a single session] have ranged in accuracy from about 86 to 89 percent,” Wittenborn said. “Studies that tried to predict changes in depression over time have been less accurate, with accuracy ranging from 59 to 85 percent.”
The Food and Drug Administration encourages the development of apps and has approved a few of them—mostly ones used by health professionals—but it is generally “hands off,” according to the American Psychiatric Association. The FDA has published a list of examples of software (including programming of apps) that it does not plan to regulate because they pose low risk to the public. First on the list is software that helps patients with diagnosed psychiatric conditions, including depression, maintain their behavioral coping skills by providing a “Skill of the Day” technique or message.
On its App Advisor site, the American Psychiatric Association says mental health apps can be dangerous or cause harm in multiple ways, such as by providing false information, overstating the app’s therapeutic value, selling personal data without clearly notifying users, and collecting data that isn’t relevant to mental health.
Although there is currently reason for caution, patients may eventually come to expect mental health professionals to recommend apps, especially as their rating systems, features and capabilities expand. Through such apps, patients might experience more and higher quality interactions with their mental health professionals. “Apps will continue to be refined and become more effective through future research,” said Wittenborn. “They will become more integrated into practice over time.”