After a Diagnosis, Patients Are Finding Solace—and Empowerment—in a Sensitive Corner of Social Media

Katherine Leon and her dog enjoy nice weather in their backyard in Virginia. Leon went from feeling like she was "wandering in the woods" with doctors who hadn't experienced her spontaneous coronary artery dissection, or SCAD, to starting the world's largest registry for research on the condition.
When Kimberly Richardson of Chicago underwent chemotherapy in 2013 for ovarian cancer, her hip began to hurt. Her doctor assigned six months of physical therapy, but the pain persisted.
She took the mystery to Facebook, where she got 200 comments from cancer survivors all pointing to the same solution: Claritin. Two days after starting the antihistamine, her hip felt fine. Claritin, it turns out, reduces bone marrow swelling, a side effect of a stimulant given after chemo.
Richardson isn't alone in using social media for health. Thirty-six percent of adults with chronic diseases have benefited from health advice on the internet, or know others who have. The trend has likely accelerated during COVID-19. "With increases in anxiety and loneliness, patients find comfort in peer support," said Chris Renfro-Wallace, the chief operating officer of PatientsLikeMe, a popular online community.
Sites like PatientsLikeMe and several others are giving rise to a patient-centered view of healthcare, challenging the idea that MD stands for medical deity. They're engaging people in new ways, such as virtual clinical trials. But with misinformation spreading online about health issues, including COVID-19, there's also reason for caution.
Engaged by Design
Following her diagnosis at age 50, Richardson searched the Web. "All I saw were infographics saying in five years I'd be dead."
Eventually, she found her Facebook groups and a site called Inspire, where she met others with her rare granulosa cell tumor. "You get 15 minutes with your doctor, but on social media you can keep posting until you satisfy your question."
Virtual communities may be especially helpful for people with rarely diagnosed diseases, who wouldn't otherwise meet. When Katherine Leon of Virginia suffered chest pain after the birth of her second son, doctors said it was spontaneous coronary artery dissection, or SCAD, involving a torn artery. But she had no risk factors for heart disease. Feeling like she was "wandering in the woods" with doctors who hadn't experienced her situation, she searched online and stumbled on communities like Inspire with members who had. The experience led her to start her own Alliance and the world's largest registry for advancing research on SCAD.
"Inspire is really an extension of yourself," she said. If designed well, online sites can foster what psychologist Keith Sawyer called group mind, a dynamic where participants balance their own voices with listening to others, maximizing community engagement in health. To achieve it, participants must have what Sawyer called a "blending of egos," which may be fostered when sites let users post anonymously. They must also share goals and open communication. The latter priority has driven Brian Loew, Inspire's CEO, to safeguard the privacy of health information exchanged on the site, often asking himself, "Would I be okay if a family member had this experience?"
The vibe isn't so familial on some of Facebook's health-focused groups. There, people might sense marketers and insurers peering over their shoulders. In 2018, a researcher discovered that companies could exploit personal information on a private Facebook community for BRCA-positive women. Members of the group started a nonprofit, the Light Collective, to help peer-to-peer support platforms improve their transparency.
PatientsLikeMe and Inspire nurture the shared experience by hosting pages on scores of diseases, allowing people to better understand treatment options for multiple conditions—and find others facing the same set of issues. Four in ten American adults have more than one chronic disease.
Sawyer observed that groups are further engaged when there's a baseline of common knowledge. To that end, some platforms take care in structuring dialogues among members to promote high-quality information, stepping in to moderate when necessary. On Inspire, members get emails when others reply to their posts, instead of instant messaging. The communication lag allows staff to notice misinformation and correct it. Facebook conversations occur in real-time among many more people; "moderation is almost impossible," said Leon.
Even on PatientsLikeMe and Inspire, deciding which content to police can be tough, as variations across individuals may result in conflicting but equally valid posts. Leon's left main artery was 90 percent blocked, requiring open heart surgery, whereas others with SCAD have angina, warranting a different approach. "It's a real range of experience," she explained. "That's probably the biggest challenge: supporting everyone where they are."
Critically, these sites don't treat illnesses. "If a member asks a medical question, we typically tell them to go to their doctor," said Loew, the Inspire CEO.
Increasingly, it may be the other way around.
The Patient Will See You Now
"Some doctors embrace the idea of an educated patient," said Loew. "The more information, the better." Others, he said, aren't thrilled about patients learning on their own.
"Doctors were behind the eight ball," said Shikha Jain, an oncologist in Chicago. "We were encouraged for years to avoid social media due to patient privacy issues. There's been a drastic shift in the last few years."
Jain recently co-founded IMPACT, a grassroots organization that networks with healthcare workers across Illinois for greater awareness of health issues. She thinks doctors must meet patients where they are—increasingly, online—and learn about the various platforms where patients connect. Doctors can then suggest credible online sources for their patients' conditions. Learning about different sites takes time, Jain said, "but that's the nature of being a physician in this day and age."
At stake is the efficiency of doctor-patient interactions. "I like when patients bring in research," Jain said. "It opens up the dialogue and lets them inform the decision-making process." Richardson, the cancer survivor, agreed. "We shouldn't make the physician the villain in this conversation." Interviewed over Zoom, she was engaging but quick to challenge the assumptions behind some questions; her toughness was palpable, molded by years of fighting disease—and the healthcare system. Many doctors are forced by that system into faster office visits, she said. "If patients help their doctor get to the heart of the issue in a shorter time, now we're going down a narrower road of tests."
These conversations could be enhanced by PatientsLikeMe's Doctor Visit Guide. It uses algorithms to consolidate health data that members track on the site into a short report they can share with their physicians. "It gives the doctor a richer data set to really see how a person has been doing," said Renfro-Wallace.
Doctors aren't the only ones benefiting from these sites.
Who Profits?
A few platforms like Inspire make money by connecting their members to drug companies, so they can participate in the companies' clinical trials to test out new therapies. A cynic might say the sites are just fronts for promoting the pharmaceuticals.
The need is real, though, as many clinical trials suffer from low participation, and the experimental treatments can improve health. The key for Loew, Inspire's CEO, is being transparent about his revenue model. "When you sign up, we assume you didn't read the fine print [in the terms of agreement]." So, when Inspire tells members about openings in trials, it's a reminder the site works with pharma.
"When I was first on Inspire, all of that was invisible to me," said Leon. "It didn't dawn on me for years." Richardson believes many don't notice pharma's involvement because they're preoccupied by their medical issues.
One way Inspire builds trust is by partnering with patient advocacy groups, which tend to be nonprofit and science-oriented, said Craig Lipset, the former head of clinical innovation for Pfizer. When he developed a rare lung disease, he joined the board of a foundation that partners with Inspire's platform. The section dedicated to his disease is emblazoned with his foundation's logo and colors. Contrast that with other sites that build communities at the direct behest of drug companies, he said.
Insurance companies are also eyeing these communities. Last month, PatientsLikeMe raised $26 million in financing from investors including Optum Ventures, which belongs to the same health care company that owns a leading health insurance company, UnitedHealthcare. PatientsLikeMe is an independent company, though, and data is shared with UnitedHealth only if patients provide consent. The site is using the influx of resources to gamify improvements in health, resembling programs run by UnitedHealth that assign nutrition and fitness "missions," with apps for tracking progress. Soon, PatientsLikeMe will roll out a smarter data tracking system that gives members actionable insights and prompts them to take actions based on their conditions, as well as competitions to motivate healthier behaviors.
Such as a race to vaccinate, perhaps.
Dealing with Misinformation
An advantage of health-focused communities is the intimacy of their gatherings, compared to behemoths like Facebook. Loew, Inspire's head, is mindful of Dunbar's rule: humans can manage only about 150 friends. Inspire's social network mapping suggests many connections among members, but of different strength; Loew hopes to keep his site's familial ambiance even while expanding membership. Renfro-Wallace is exploring video and voice-only meetings to enrich the shared experiences on PatientsLikeMe, while respecting members' privacy.
But a main driver of growth and engagement online is appealing to emotion rather than reason; witness Facebook during the pandemic. "We know that misinformation and scary things spread far more rapidly than something positive," said Ann Lewandowski, the executive director of Wisconsin Immunization Neighborhood, a coalition of health providers and associations countering vaccine hesitancy across the state.
"Facebook's moderation mechanism is terrible," she said. Vaccine advocates in her region who try to flag misinformation on Facebook often have their content removed because the site's algorithm associates their posts with the distortions they're trying to warn people about.
In the realm of health, where accessing facts can mean life or death—and where ad-based revenue models conflict with privacy needs—there's probably a ceiling on how large social media sites should scale. Loew views Inspire as co-existing, not competing with Facebook.
Propagandists had months to perfect campaigns to dissuade people from mRNA vaccines. But even Lewandowski's doctor was misinformed about vaccine side effects for her condition, multiple sclerosis. She sees potential for health-focused sites to convene more virtual forums, in which patient advocacy groups educate doctors and patients on vaccine safety.
Inspire is raising awareness about COVID vaccines through a member survey with an interactive data visualization. Sampling thousands of members, the survey found vaccines are tolerated well among patients with cancer, autoimmune issues, and other serious conditions. Analytics for online groups are evolving quickly, said Lipset. "Think about the acceleration in research when you take the emerging capability for aggregating health data and mash it up with patients engaged in sharing."
Lipset recently co-founded the Decentralized Trials and Research Alliance to accelerate clinical trials and make them more accessible to patients—even from home, without risking the virus. Sites like PatientsLikeMe share this commitment, collaborating with Duke's ALS Clinic to let patients join a trial from home with just two clinic visits. Synthetic control groups were created by PatientsLikeMe's algorithms, eliminating the need for a placebo arm, enabling faster results.
As for Richardson, the ovarian cancer patient, being online has given her another type of access—to experts. She was diagnosed this year with breast cancer. "This time is totally different," she said. On Twitter, she's been direct messaging cancer researchers, whose replies have informed her disease-management strategy. When her oncologists prescribed 33 radiation treatments, she counter-proposed upping the dosage over fewer treatments. Her doctors agreed, cutting unnecessary trips from home. "I'm immuno-compromised," she said. "It's like Russian roulette. You're crossing your finger you won't get the virus."
After years of sticking up for her own health, Richardson is now positioned to look out for others. She collaborated with the University of Illinois Cancer Center on a training module that lets patients take control of their health. She's sharing it online, in a virtual community near you. "It helps you make intelligent decisions," she said. "When you speak your physician's language, it shifts the power in the room."
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
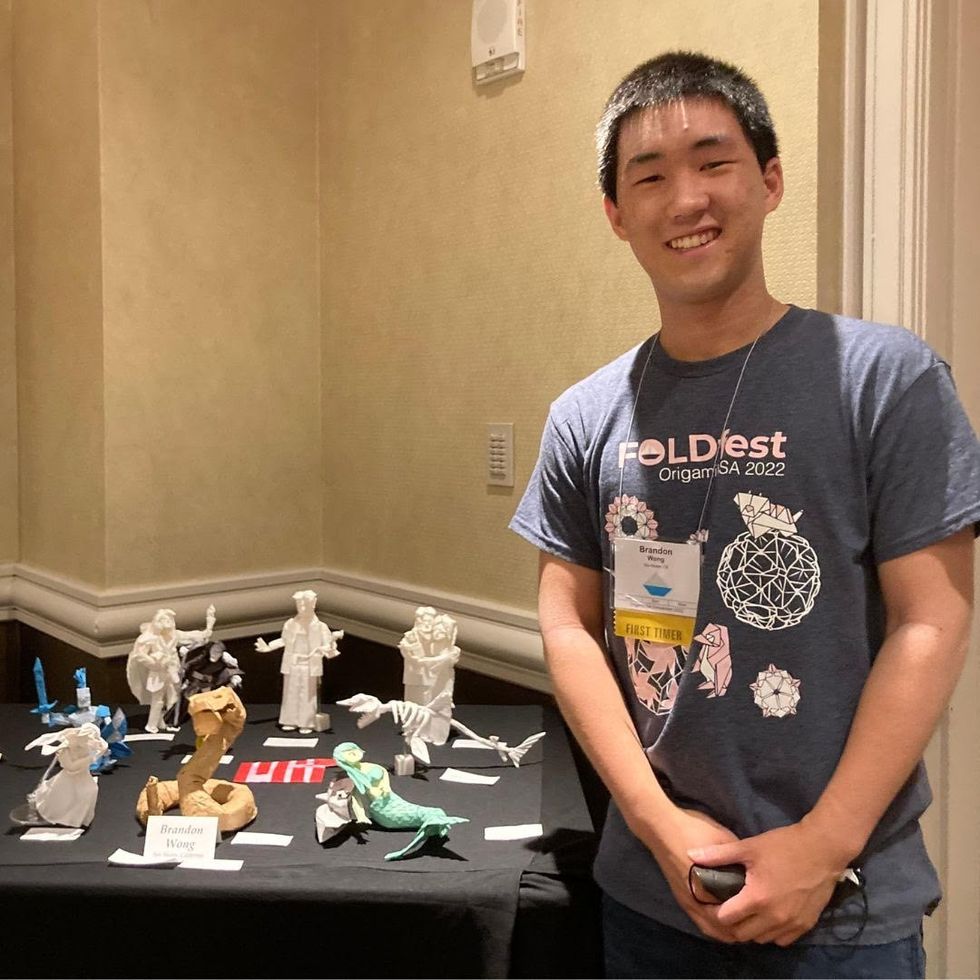
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

