After a Diagnosis, Patients Are Finding Solace—and Empowerment—in a Sensitive Corner of Social Media

Katherine Leon and her dog enjoy nice weather in their backyard in Virginia. Leon went from feeling like she was "wandering in the woods" with doctors who hadn't experienced her spontaneous coronary artery dissection, or SCAD, to starting the world's largest registry for research on the condition.
When Kimberly Richardson of Chicago underwent chemotherapy in 2013 for ovarian cancer, her hip began to hurt. Her doctor assigned six months of physical therapy, but the pain persisted.
She took the mystery to Facebook, where she got 200 comments from cancer survivors all pointing to the same solution: Claritin. Two days after starting the antihistamine, her hip felt fine. Claritin, it turns out, reduces bone marrow swelling, a side effect of a stimulant given after chemo.
Richardson isn't alone in using social media for health. Thirty-six percent of adults with chronic diseases have benefited from health advice on the internet, or know others who have. The trend has likely accelerated during COVID-19. "With increases in anxiety and loneliness, patients find comfort in peer support," said Chris Renfro-Wallace, the chief operating officer of PatientsLikeMe, a popular online community.
Sites like PatientsLikeMe and several others are giving rise to a patient-centered view of healthcare, challenging the idea that MD stands for medical deity. They're engaging people in new ways, such as virtual clinical trials. But with misinformation spreading online about health issues, including COVID-19, there's also reason for caution.
Engaged by Design
Following her diagnosis at age 50, Richardson searched the Web. "All I saw were infographics saying in five years I'd be dead."
Eventually, she found her Facebook groups and a site called Inspire, where she met others with her rare granulosa cell tumor. "You get 15 minutes with your doctor, but on social media you can keep posting until you satisfy your question."
Virtual communities may be especially helpful for people with rarely diagnosed diseases, who wouldn't otherwise meet. When Katherine Leon of Virginia suffered chest pain after the birth of her second son, doctors said it was spontaneous coronary artery dissection, or SCAD, involving a torn artery. But she had no risk factors for heart disease. Feeling like she was "wandering in the woods" with doctors who hadn't experienced her situation, she searched online and stumbled on communities like Inspire with members who had. The experience led her to start her own Alliance and the world's largest registry for advancing research on SCAD.
"Inspire is really an extension of yourself," she said. If designed well, online sites can foster what psychologist Keith Sawyer called group mind, a dynamic where participants balance their own voices with listening to others, maximizing community engagement in health. To achieve it, participants must have what Sawyer called a "blending of egos," which may be fostered when sites let users post anonymously. They must also share goals and open communication. The latter priority has driven Brian Loew, Inspire's CEO, to safeguard the privacy of health information exchanged on the site, often asking himself, "Would I be okay if a family member had this experience?"
The vibe isn't so familial on some of Facebook's health-focused groups. There, people might sense marketers and insurers peering over their shoulders. In 2018, a researcher discovered that companies could exploit personal information on a private Facebook community for BRCA-positive women. Members of the group started a nonprofit, the Light Collective, to help peer-to-peer support platforms improve their transparency.
PatientsLikeMe and Inspire nurture the shared experience by hosting pages on scores of diseases, allowing people to better understand treatment options for multiple conditions—and find others facing the same set of issues. Four in ten American adults have more than one chronic disease.
Sawyer observed that groups are further engaged when there's a baseline of common knowledge. To that end, some platforms take care in structuring dialogues among members to promote high-quality information, stepping in to moderate when necessary. On Inspire, members get emails when others reply to their posts, instead of instant messaging. The communication lag allows staff to notice misinformation and correct it. Facebook conversations occur in real-time among many more people; "moderation is almost impossible," said Leon.
Even on PatientsLikeMe and Inspire, deciding which content to police can be tough, as variations across individuals may result in conflicting but equally valid posts. Leon's left main artery was 90 percent blocked, requiring open heart surgery, whereas others with SCAD have angina, warranting a different approach. "It's a real range of experience," she explained. "That's probably the biggest challenge: supporting everyone where they are."
Critically, these sites don't treat illnesses. "If a member asks a medical question, we typically tell them to go to their doctor," said Loew, the Inspire CEO.
Increasingly, it may be the other way around.
The Patient Will See You Now
"Some doctors embrace the idea of an educated patient," said Loew. "The more information, the better." Others, he said, aren't thrilled about patients learning on their own.
"Doctors were behind the eight ball," said Shikha Jain, an oncologist in Chicago. "We were encouraged for years to avoid social media due to patient privacy issues. There's been a drastic shift in the last few years."
Jain recently co-founded IMPACT, a grassroots organization that networks with healthcare workers across Illinois for greater awareness of health issues. She thinks doctors must meet patients where they are—increasingly, online—and learn about the various platforms where patients connect. Doctors can then suggest credible online sources for their patients' conditions. Learning about different sites takes time, Jain said, "but that's the nature of being a physician in this day and age."
At stake is the efficiency of doctor-patient interactions. "I like when patients bring in research," Jain said. "It opens up the dialogue and lets them inform the decision-making process." Richardson, the cancer survivor, agreed. "We shouldn't make the physician the villain in this conversation." Interviewed over Zoom, she was engaging but quick to challenge the assumptions behind some questions; her toughness was palpable, molded by years of fighting disease—and the healthcare system. Many doctors are forced by that system into faster office visits, she said. "If patients help their doctor get to the heart of the issue in a shorter time, now we're going down a narrower road of tests."
These conversations could be enhanced by PatientsLikeMe's Doctor Visit Guide. It uses algorithms to consolidate health data that members track on the site into a short report they can share with their physicians. "It gives the doctor a richer data set to really see how a person has been doing," said Renfro-Wallace.
Doctors aren't the only ones benefiting from these sites.
Who Profits?
A few platforms like Inspire make money by connecting their members to drug companies, so they can participate in the companies' clinical trials to test out new therapies. A cynic might say the sites are just fronts for promoting the pharmaceuticals.
The need is real, though, as many clinical trials suffer from low participation, and the experimental treatments can improve health. The key for Loew, Inspire's CEO, is being transparent about his revenue model. "When you sign up, we assume you didn't read the fine print [in the terms of agreement]." So, when Inspire tells members about openings in trials, it's a reminder the site works with pharma.
"When I was first on Inspire, all of that was invisible to me," said Leon. "It didn't dawn on me for years." Richardson believes many don't notice pharma's involvement because they're preoccupied by their medical issues.
One way Inspire builds trust is by partnering with patient advocacy groups, which tend to be nonprofit and science-oriented, said Craig Lipset, the former head of clinical innovation for Pfizer. When he developed a rare lung disease, he joined the board of a foundation that partners with Inspire's platform. The section dedicated to his disease is emblazoned with his foundation's logo and colors. Contrast that with other sites that build communities at the direct behest of drug companies, he said.
Insurance companies are also eyeing these communities. Last month, PatientsLikeMe raised $26 million in financing from investors including Optum Ventures, which belongs to the same health care company that owns a leading health insurance company, UnitedHealthcare. PatientsLikeMe is an independent company, though, and data is shared with UnitedHealth only if patients provide consent. The site is using the influx of resources to gamify improvements in health, resembling programs run by UnitedHealth that assign nutrition and fitness "missions," with apps for tracking progress. Soon, PatientsLikeMe will roll out a smarter data tracking system that gives members actionable insights and prompts them to take actions based on their conditions, as well as competitions to motivate healthier behaviors.
Such as a race to vaccinate, perhaps.
Dealing with Misinformation
An advantage of health-focused communities is the intimacy of their gatherings, compared to behemoths like Facebook. Loew, Inspire's head, is mindful of Dunbar's rule: humans can manage only about 150 friends. Inspire's social network mapping suggests many connections among members, but of different strength; Loew hopes to keep his site's familial ambiance even while expanding membership. Renfro-Wallace is exploring video and voice-only meetings to enrich the shared experiences on PatientsLikeMe, while respecting members' privacy.
But a main driver of growth and engagement online is appealing to emotion rather than reason; witness Facebook during the pandemic. "We know that misinformation and scary things spread far more rapidly than something positive," said Ann Lewandowski, the executive director of Wisconsin Immunization Neighborhood, a coalition of health providers and associations countering vaccine hesitancy across the state.
"Facebook's moderation mechanism is terrible," she said. Vaccine advocates in her region who try to flag misinformation on Facebook often have their content removed because the site's algorithm associates their posts with the distortions they're trying to warn people about.
In the realm of health, where accessing facts can mean life or death—and where ad-based revenue models conflict with privacy needs—there's probably a ceiling on how large social media sites should scale. Loew views Inspire as co-existing, not competing with Facebook.
Propagandists had months to perfect campaigns to dissuade people from mRNA vaccines. But even Lewandowski's doctor was misinformed about vaccine side effects for her condition, multiple sclerosis. She sees potential for health-focused sites to convene more virtual forums, in which patient advocacy groups educate doctors and patients on vaccine safety.
Inspire is raising awareness about COVID vaccines through a member survey with an interactive data visualization. Sampling thousands of members, the survey found vaccines are tolerated well among patients with cancer, autoimmune issues, and other serious conditions. Analytics for online groups are evolving quickly, said Lipset. "Think about the acceleration in research when you take the emerging capability for aggregating health data and mash it up with patients engaged in sharing."
Lipset recently co-founded the Decentralized Trials and Research Alliance to accelerate clinical trials and make them more accessible to patients—even from home, without risking the virus. Sites like PatientsLikeMe share this commitment, collaborating with Duke's ALS Clinic to let patients join a trial from home with just two clinic visits. Synthetic control groups were created by PatientsLikeMe's algorithms, eliminating the need for a placebo arm, enabling faster results.
As for Richardson, the ovarian cancer patient, being online has given her another type of access—to experts. She was diagnosed this year with breast cancer. "This time is totally different," she said. On Twitter, she's been direct messaging cancer researchers, whose replies have informed her disease-management strategy. When her oncologists prescribed 33 radiation treatments, she counter-proposed upping the dosage over fewer treatments. Her doctors agreed, cutting unnecessary trips from home. "I'm immuno-compromised," she said. "It's like Russian roulette. You're crossing your finger you won't get the virus."
After years of sticking up for her own health, Richardson is now positioned to look out for others. She collaborated with the University of Illinois Cancer Center on a training module that lets patients take control of their health. She's sharing it online, in a virtual community near you. "It helps you make intelligent decisions," she said. "When you speak your physician's language, it shifts the power in the room."
The U.S. must fund more biotech innovation – or other countries will catch up faster than you think
In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

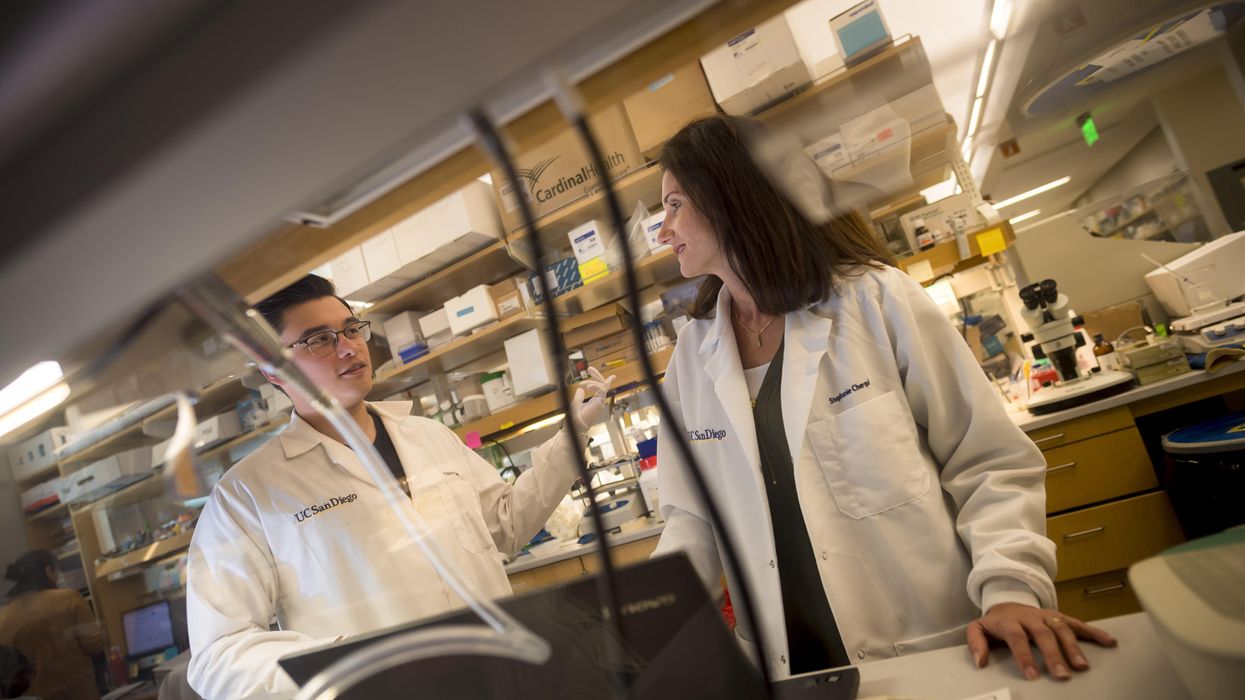
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.