The future of non-hormonal birth control: Antibodies can stop sperm in their tracks

Many women want non-hormonal birth control. A 22-year-old's findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
Unwanted pregnancy can now be added to the list of preventions that antibodies may be fighting in the near future. For decades, really since the 1980s, engineered monoclonal antibodies have been knocking out invading germs — preventing everything from cancer to COVID. Sperm, which have some of the same properties as germs, may be next.
Not only is there an unmet need on the market for alternatives to hormonal contraceptives, the genesis for the original research was personal for the then 22-year-old scientist who led it. Her findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
The genesis
It’s Suruchi Shrestha’s research — published in Science Translational Medicine in August 2021 and conducted as part of her dissertation while she was a graduate student at the University of North Carolina at Chapel Hill — that could change the future of contraception for many women worldwide. According to a Guttmacher Institute report, in the U.S. alone, there were 46 million sexually active women of reproductive age (15–49) who did not want to get pregnant in 2018. With the overturning of Roe v. Wade last year, Shrestha’s research could, indeed, be life changing for millions of American women and their families.
Now a scientist with NextVivo, Shrestha is not directly involved in the development of the contraceptive that is based on her research. But, back in 2016 when she was going through her own problems with hormonal contraceptives, she “was very personally invested” in her research project, Shrestha says. She was coping with a long list of negative effects from an implanted hormonal IUD. According to the Mayo Clinic, those can include severe pelvic pain, headaches, acute acne, breast tenderness, irregular bleeding and mood swings. After a year, she had the IUD removed, but it took another full year before all the side effects finally subsided; she also watched her sister suffer the “same tribulations” after trying a hormonal IUD, she says.
For contraceptive use either daily or monthly, Shrestha says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
Shrestha unshelved antibody research that had been sitting idle for decades. It was in the late 80s that scientists in Japan first tried to develop anti-sperm antibodies for contraceptive use. But, 35 years ago, “Antibody production had not been streamlined as it is now, so antibodies were very expensive,” Shrestha explains. So, they shifted away from birth control, opting to focus on developing antibodies for vaccines.
Over the course of the last three decades, different teams of researchers have been working to make the antibody more effective, bringing the cost down, though it’s still expensive, according to Shrestha. For contraceptive use either daily or monthly, she says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
The problem
The problem with contraceptives for women, Shrestha says, is that all but a few of them are hormone-based or have other negative side effects. In fact, some studies and reports show that millions of women risk unintended pregnancy because of medical contraindications with hormone-based contraceptives or to avoid the risks and side effects. While there are about a dozen contraceptive choices for women, there are two for men: the condom, considered 98% effective if used correctly, and vasectomy, 99% effective. Neither of these choices are hormone-based.
On the non-hormonal side for women, there is the diaphragm which is considered only 87 percent effective. It works better with the addition of spermicides — Nonoxynol-9, or N-9 — however, they are detergents; they not only kill the sperm, they also erode the vaginal epithelium. And, there’s the non-hormonal IUD which is 99% effective. However, the IUD needs to be inserted by a medical professional, and it has a number of negative side effects, including painful cramping at a higher frequency and extremely heavy or “abnormal” and unpredictable menstrual flows.
The hormonal version of the IUD, also considered 99% effective, is the one Shrestha used which caused her two years of pain. Of course, there’s the pill, which needs to be taken daily, and the birth control ring which is worn 24/7. Both cause side effects similar to the other hormonal contraceptives on the market. The ring is considered 93% effective mostly because of user error; the pill is considered 99% effective if taken correctly.
“That’s where we saw this opening or gap for women. We want a safe, non-hormonal contraceptive,” Shrestha says. Compounding the lack of good choices, is poor access to quality sex education and family planning information, according to the non-profit Urban Institute. A focus group survey suggested that the sex education women received “often lacked substance, leaving them feeling unprepared to make smart decisions about their sexual health and safety,” wrote the authors of the Urban Institute report. In fact, nearly half (45%, or 2.8 million) of the pregnancies that occur each year in the US are unintended, reports the Guttmacher Institute. Globally the numbers are similar. According to a new report by the United Nations, each year there are 121 million unintended pregnancies, worldwide.
The science
The early work on antibodies as a contraceptive had been inspired by women with infertility. It turns out that 9 to 12 percent of women who are treated for infertility have antibodies that develop naturally and work against sperm. Shrestha was encouraged that the antibodies were specific to the target — sperm — and therefore “very safe to use in women.” She aimed to make the antibodies more stable, more effective and less expensive so they could be more easily manufactured.
Since antibodies tend to stick to things that you tell them to stick to, the idea was, basically, to engineer antibodies to stick to sperm so they would stop swimming. Shrestha and her colleagues took the binding arm of an antibody that they’d isolated from an infertile woman. Then, targeting a unique surface antigen present on human sperm, they engineered a panel of antibodies with as many as six to 10 binding arms — “almost like tongs with prongs on the tongs, that bind the sperm,” explains Shrestha. “We decided to add those grabbers on top of it, behind it. So it went from having two prongs to almost 10. And the whole goal was to have so many arms binding the sperm that it clumps it” into a “dollop,” explains Shrestha, who earned a patent on her research.
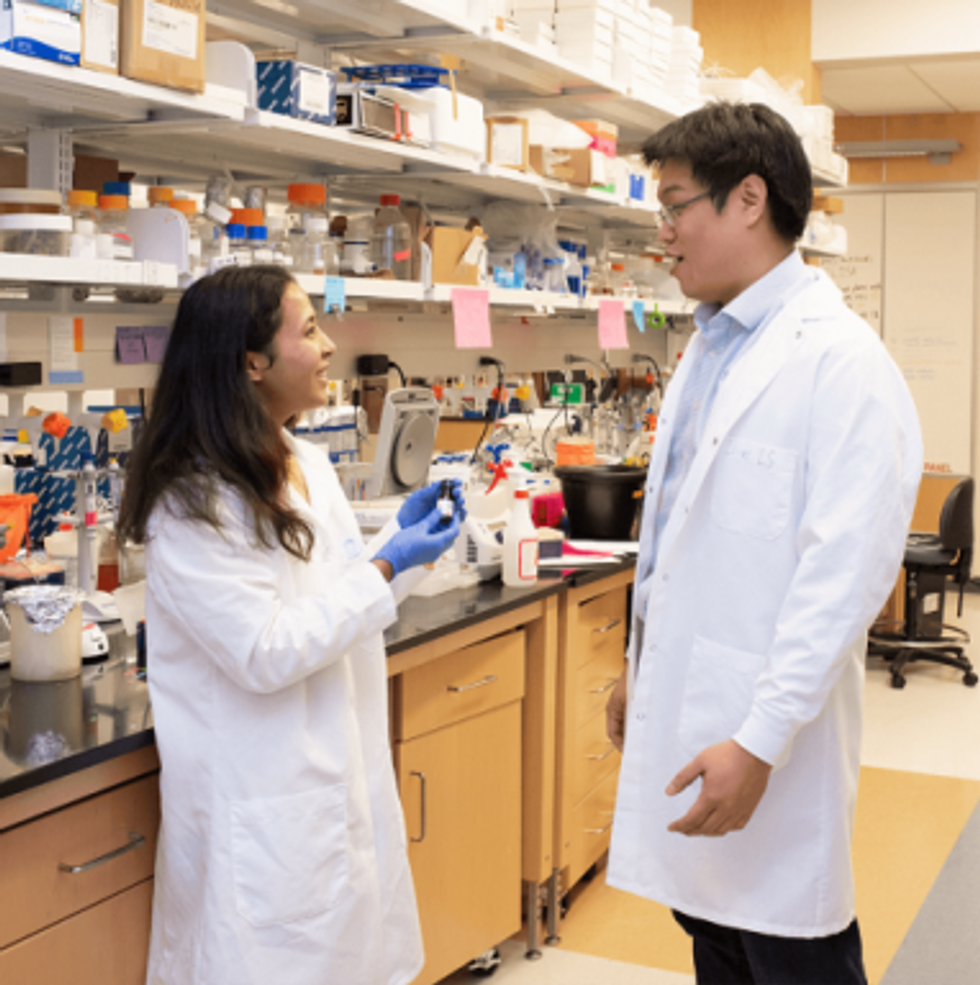
Suruchi Shrestha works in the lab with a colleague. In 2016, her research on antibodies for birth control was inspired by her own experience with side effects from an implanted hormonal IUD.
UNC - Chapel Hill
The sperm stays right where it met the antibody, never reaching the egg for fertilization. Eventually, and naturally, “Our vaginal system will just flush it out,” Shrestha explains.
“She showed in her early studies that [she] definitely got the sperm immotile, so they didn't move. And that was a really promising start,” says Jasmine Edelstein, a scientist with an expertise in antibody engineering who was not involved in this research. Shrestha’s team at UNC reproduced the effect in the sheep, notes Edelstein, who works at the startup Be Biopharma. In fact, Shrestha’s anti-sperm antibodies that caused the sperm to agglutinate, or clump together, were 99.9% effective when delivered topically to the sheep’s reproductive tracts.
The future
Going forward, Shrestha thinks the ideal approach would be delivering the antibodies through a vaginal ring. “We want to use it at the source of the spark,” Shrestha says, as opposed to less direct methods, such as taking a pill. The ring would dissolve after one month, she explains, “and then you get another one.”
Engineered to have a long shelf life, the anti-sperm antibody ring could be purchased without a prescription, and women could insert it themselves, without a doctor. “That's our hope, so that it is accessible,” Shrestha says. “Anybody can just go and grab it and not worry about pregnancy or unintended pregnancy.”
Her patented research has been licensed by several biotech companies for clinical trials. A number of Shrestha’s co-authors, including her lab advisor, Sam Lai, have launched a company, Mucommune, to continue developing the contraceptives based on these antibodies.
And, results from a small clinical trial run by researchers at Boston University Chobanian & Avedisian School of Medicine show that a dissolvable vaginal film with antibodies was safe when tested on healthy women of reproductive age. That same group of researchers last year received a $7.2 million grant from the National Institute of Health for further research on monoclonal antibody-based contraceptives, which have also been shown to block transmission of viruses, like HIV.
“As the costs come down, this becomes a more realistic option potentially for women,” says Edelstein. “The impact could be tremendous.”
This article was first published by Leaps.org in December, 2022. It has been lightly edited with updates for timeliness.
Harvard Researchers Are Using a Breakthrough Tool to Find the Antibodies That Best Knock Out the Coronavirus
Knowing which antibodies bind best to the coronavirus can help guide new medicines and vaccine development.
To find a cure for a deadly infectious disease in the 1995 medical thriller Outbreak, scientists extract the virus's antibodies from its original host—an African monkey.
"When a person is infected, the immune system makes antibodies kind of blindly."
The antibodies prevent the monkeys from getting sick, so doctors use these antibodies to make the therapeutic serum for humans. With SARS-CoV-2, the original hosts might be bats or pangolins, but scientists don't have access to either, so they are turning to the humans who beat the virus.
Patients who recovered from COVID-19 are valuable reservoirs of viral antibodies and may help scientists develop efficient therapeutics, says Stephen J. Elledge, professor of genetics and medicine at Harvard Medical School in Boston. Studying the structure of the antibodies floating in their blood can help understand what their immune systems did right to kill the pathogen.
When viruses invade the body, the immune system builds antibodies against them. The antibodies work like Velcro strips—they use special spots on their surface called paratopes to cling to the specific spots on the viral shell called epitopes. Once the antibodies circulating in the blood find their "match," they cling on to the virus and deactivate it.
But that process is far from simple. The epitopes and paratopes are built of various peptides that have complex shapes, are folded in specific ways, and may carry an electrical charge that repels certain molecules. Only when all of these parameters match, an antibody can get close enough to a viral particle—and shut it out.
So the immune system forges many different antibodies with varied parameters in hopes that some will work. "When a person is infected, the immune system makes antibodies kind of blindly," Elledge says. "It's doing a shotgun approach. It's not sure which ones will work, but it knows once it's made a good one that works."
Elledge and his team want to take the guessing out of the process. They are using their home-built tool VirScan to comb through the blood samples of the recovered COVID-19 patients to see what parameters the efficient antibodies should have. First developed in 2015, the VirScan has a library of epitopes found on the shells of viruses known to afflict humans, akin to a database of criminals' mug shots maintained by the police.
Originally, VirScan was meant to reveal which pathogens a person overcame throughout a lifetime, and could identify over 1,000 different strains of viruses and bacteria. When the team ran blood samples against the VirScan's library, the tool would pick out all the "usual suspects." And unlike traditional blood tests called ELISA, which can only detect one pathogen at a time, VirScan can detect all of them at once. Now, the team has updated VirScan with the SARS-CoV-2 "mug shot" and is beginning to test which antibodies from the recovered patients' blood will bind to them.
Knowing which antibodies bind best can also help fine-tune vaccines.
Obtaining blood samples was a challenge that caused some delays. "So far most of the recovered patients have been in China and those samples are hard to get," Elledge says. It also takes a person five to 10 days to develop antibodies, so the blood must be drawn at the right time during the illness. If a person is asymptomatic, it's hard to pinpoint the right moment. "We just got a couple of blood samples so we are testing now," he said. The team hopes to get some results very soon.
Elucidating the structure of efficient antibodies can help create therapeutics for COVID-19. "VirScan is a powerful technology to study antibody responses," says Harvard Medical School professor Dan Barouch, who also directs the Center for Virology and Vaccine Research. "A detailed understanding of the antibody responses to COVID-19 will help guide the design of next-generation vaccines and therapeutics."
For example, scientists can synthesize antibodies to specs and give them to patients as medicine. Once vaccines are designed, medics can use VirScan to see if those vaccinated again COVID-19 generate the necessary antibodies.
Knowing which antibodies bind best can also help fine-tune vaccines. Sometimes, viruses cause the immune system to generate antibodies that don't deactivate it. "We think the virus is trying to confuse the immune system; it is its business plan," Elledge says—so those unhelpful antibodies shouldn't be included in vaccines.
More importantly, VirScan can also tell which people have developed immunity to SARS-CoV-2 and can return to their workplaces and businesses, which is crucial to restoring the economy. Knowing one's immunity status is especially important for doctors working on the frontlines, Elledge notes. "The resistant ones can intubate the sick."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Defenders of civil liberties fear that the erosion of privacy will become a long-term consequence of the pandemic.
As countries around the world combat the coronavirus outbreak, governments that already operated sophisticated surveillance programs are ramping up the tracking of their citizens.
"The potential for invasions of privacy, abuse, and stigmatization is enormous."
Countries like China, South Korea, Israel, Singapore and others are closely monitoring citizens to track the spread of the virus and prevent further infections, and policymakers in the United States have proposed similar steps. These shifts in policy have civil liberties defenders alarmed, as history has shown increases in surveillance tend to stick around after an emergency is over.
In China, where the virus originated and surveillance is already ubiquitous, the government has taken measures like having people scan a QR code and answer questions about their health and travel history to enter their apartment building. The country has also increased the tracking of cell phones, encouraged citizens to report people who appear to be sick, utilized surveillance drones, and developed facial recognition that can identify someone even if they're wearing a mask.
In Israel, the government has begun tracking people's cell phones without a court order under a program that was initially meant to counter terrorism. Singapore has also been closely tracking people's movements using cell phone data. In South Korea, the government has been monitoring citizens' credit card and cell phone data and has heavily utilized facial recognition to combat the spread of the coronavirus.
Here at home, the United States government and state governments have been using cell phone data to determine where people are congregating. White House senior adviser Jared Kushner's task force to combat the coronavirus outbreak has proposed using cell phone data to track coronavirus patients. Cities around the nation are also using surveillance drones to maintain social distancing orders. Companies like Apple and Google that work closely with the federal government are currently developing systems to track Americans' cell phones.
All of this might sound acceptable if you're worried about containing the outbreak and getting back to normal life, but as we saw when the Patriot Act was passed in 2001 in the wake of the 9/11 terrorist attacks, expansions of the surveillance state can persist long after the emergency that seemed to justify them.
Jay Stanley, senior policy analyst with the ACLU Speech, Privacy, and Technology Project, says that this public health emergency requires bold action, but he worries that actions may be taken that will infringe on our privacy rights.
"This is an extraordinary crisis that justifies things that would not be justified in ordinary times, but we, of course, worry that any such things would be made permanent," Stanley says.
Stanley notes that the 9/11 situation was different from this current situation because we still face the threat of terrorism today, and we always will. The Patriot Act was a response to that threat, even if it was an extreme response. With this pandemic, it's quite possible we won't face something like this again for some time.
"We know that for the last seven or eight decades, we haven't seen a microbe this dangerous become a pandemic, and it's reasonable to expect it's not going to be happening for a while afterward," Stanley says. "We do know that when a vaccine is produced and is produced widely enough, the COVID crisis will be over. This does, unlike 9/11, have a definitive ending."
The ACLU released a white paper last week outlining the problems with using location data from cell phones and how policymakers should proceed when they discuss the usage of surveillance to combat the outbreak.
"Location data contains an enormously invasive and personal set of information about each of us, with the potential to reveal such things as people's social, sexual, religious, and political associations," they wrote. "The potential for invasions of privacy, abuse, and stigmatization is enormous. Any uses of such data should be temporary, restricted to public health agencies and purposes, and should make the greatest possible use of available techniques that allow for privacy and anonymity to be protected, even as the data is used."
"The first thing you need to combat pervasive surveillance is to know that it's occurring."
Sara Collins, policy counsel at the digital rights organization Public Knowledge, says that one of the problems with the current administration is that there's not much transparency, so she worries surveillance could be increased without the public realizing it.
"You'll often see the White House come out with something—that they're going to take this action or an agency just says they're going to take this action—and there's no congressional authorization," Collins says. "There's no regulation. There's nothing there for the public discourse."
Collins says it's almost impossible to protect against infringements on people's privacy rights if you don't actually know what kind of surveillance is being done and at what scale.
"I think that's very concerning when there's no accountability and no way to understand what's actually happening," Collins says. "The first thing you need to combat pervasive surveillance is to know that it's occurring."
We should also be worried about corporate surveillance, Collins says, because the tech companies that keep track of our data work closely with the government and do not have a good track record when it comes to protecting people's privacy. She suspects these companies could use the coronavirus outbreak to defend the kind of data collection they've been engaging in for years.
Collins stresses that any increase in surveillance should be transparent and short-lived, and that there should be a limit on how long people's data can be kept. Otherwise, she says, we're risking an indefinite infringement on privacy rights. Her organization will be keeping tabs as the crisis progresses.
It's not that we shouldn't avail ourselves of modern technology to fight the pandemic. Indeed, once lockdown restrictions are gradually lifted, public health officials must increase their ability to isolate new cases and trace, test, and quarantine contacts.
But tracking the entire populace "Big Brother"-style is not the ideal way out of the crisis. Last week, for instance, a group of policy experts -- including former FDA Commissioner Scott Gottlieb -- published recommendations for how to achieve containment. They emphasized the need for widespread diagnostic and serologic testing as well as rapid case-based interventions, among other measures -- and they, too, were wary of pervasive measures to follow citizens.
The group wrote: "Improved capacity [for timely contact tracing] will be most effective if coordinated with health care providers, health systems, and health plans and supported by timely electronic data sharing. Cell phone-based apps recording proximity events between individuals are unlikely to have adequate discriminating ability or adoption to achieve public health utility, while introducing serious privacy, security, and logistical concerns."
The bottom line: Any broad increases in surveillance should be carefully considered before we go along with them out of fear. The Founders knew that privacy is integral to freedom; that's why they wrote the Fourth Amendment to protect it, and that right shouldn't be thrown away because we're in an emergency. Once you lose a right, you don't tend to get it back.