The future of non-hormonal birth control: Antibodies can stop sperm in their tracks

Many women want non-hormonal birth control. A 22-year-old's findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
Unwanted pregnancy can now be added to the list of preventions that antibodies may be fighting in the near future. For decades, really since the 1980s, engineered monoclonal antibodies have been knocking out invading germs — preventing everything from cancer to COVID. Sperm, which have some of the same properties as germs, may be next.
Not only is there an unmet need on the market for alternatives to hormonal contraceptives, the genesis for the original research was personal for the then 22-year-old scientist who led it. Her findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
The genesis
It’s Suruchi Shrestha’s research — published in Science Translational Medicine in August 2021 and conducted as part of her dissertation while she was a graduate student at the University of North Carolina at Chapel Hill — that could change the future of contraception for many women worldwide. According to a Guttmacher Institute report, in the U.S. alone, there were 46 million sexually active women of reproductive age (15–49) who did not want to get pregnant in 2018. With the overturning of Roe v. Wade this year, Shrestha’s research could, indeed, be life changing for millions of American women and their families.
Now a scientist with NextVivo, Shrestha is not directly involved in the development of the contraceptive that is based on her research. But, back in 2016 when she was going through her own problems with hormonal contraceptives, she “was very personally invested” in her research project, Shrestha says. She was coping with a long list of negative effects from an implanted hormonal IUD. According to the Mayo Clinic, those can include severe pelvic pain, headaches, acute acne, breast tenderness, irregular bleeding and mood swings. After a year, she had the IUD removed, but it took another full year before all the side effects finally subsided; she also watched her sister suffer the “same tribulations” after trying a hormonal IUD, she says.
For contraceptive use either daily or monthly, Shrestha says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
Shrestha unshelved antibody research that had been sitting idle for decades. It was in the late 80s that scientists in Japan first tried to develop anti-sperm antibodies for contraceptive use. But, 35 years ago, “Antibody production had not been streamlined as it is now, so antibodies were very expensive,” Shrestha explains. So, they shifted away from birth control, opting to focus on developing antibodies for vaccines.
Over the course of the last three decades, different teams of researchers have been working to make the antibody more effective, bringing the cost down, though it’s still expensive, according to Shrestha. For contraceptive use either daily or monthly, she says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
The problem
The problem with contraceptives for women, Shrestha says, is that all but a few of them are hormone-based or have other negative side effects. In fact, some studies and reports show that millions of women risk unintended pregnancy because of medical contraindications with hormone-based contraceptives or to avoid the risks and side effects. While there are about a dozen contraceptive choices for women, there are two for men: the condom, considered 98% effective if used correctly, and vasectomy, 99% effective. Neither of these choices are hormone-based.
On the non-hormonal side for women, there is the diaphragm which is considered only 87 percent effective. It works better with the addition of spermicides — Nonoxynol-9, or N-9 — however, they are detergents; they not only kill the sperm, they also erode the vaginal epithelium. And, there’s the non-hormonal IUD which is 99% effective. However, the IUD needs to be inserted by a medical professional, and it has a number of negative side effects, including painful cramping at a higher frequency and extremely heavy or “abnormal” and unpredictable menstrual flows.
The hormonal version of the IUD, also considered 99% effective, is the one Shrestha used which caused her two years of pain. Of course, there’s the pill, which needs to be taken daily, and the birth control ring which is worn 24/7. Both cause side effects similar to the other hormonal contraceptives on the market. The ring is considered 93% effective mostly because of user error; the pill is considered 99% effective if taken correctly.
“That’s where we saw this opening or gap for women. We want a safe, non-hormonal contraceptive,” Shrestha says. Compounding the lack of good choices, is poor access to quality sex education and family planning information, according to the non-profit Urban Institute. A focus group survey suggested that the sex education women received “often lacked substance, leaving them feeling unprepared to make smart decisions about their sexual health and safety,” wrote the authors of the Urban Institute report. In fact, nearly half (45%, or 2.8 million) of the pregnancies that occur each year in the US are unintended, reports the Guttmacher Institute. Globally the numbers are similar. According to a new report by the United Nations, each year there are 121 million unintended pregnancies, worldwide.
The science
The early work on antibodies as a contraceptive had been inspired by women with infertility. It turns out that 9 to 12 percent of women who are treated for infertility have antibodies that develop naturally and work against sperm. Shrestha was encouraged that the antibodies were specific to the target — sperm — and therefore “very safe to use in women.” She aimed to make the antibodies more stable, more effective and less expensive so they could be more easily manufactured.
Since antibodies tend to stick to things that you tell them to stick to, the idea was, basically, to engineer antibodies to stick to sperm so they would stop swimming. Shrestha and her colleagues took the binding arm of an antibody that they’d isolated from an infertile woman. Then, targeting a unique surface antigen present on human sperm, they engineered a panel of antibodies with as many as six to 10 binding arms — “almost like tongs with prongs on the tongs, that bind the sperm,” explains Shrestha. “We decided to add those grabbers on top of it, behind it. So it went from having two prongs to almost 10. And the whole goal was to have so many arms binding the sperm that it clumps it” into a “dollop,” explains Shrestha, who earned a patent on her research.
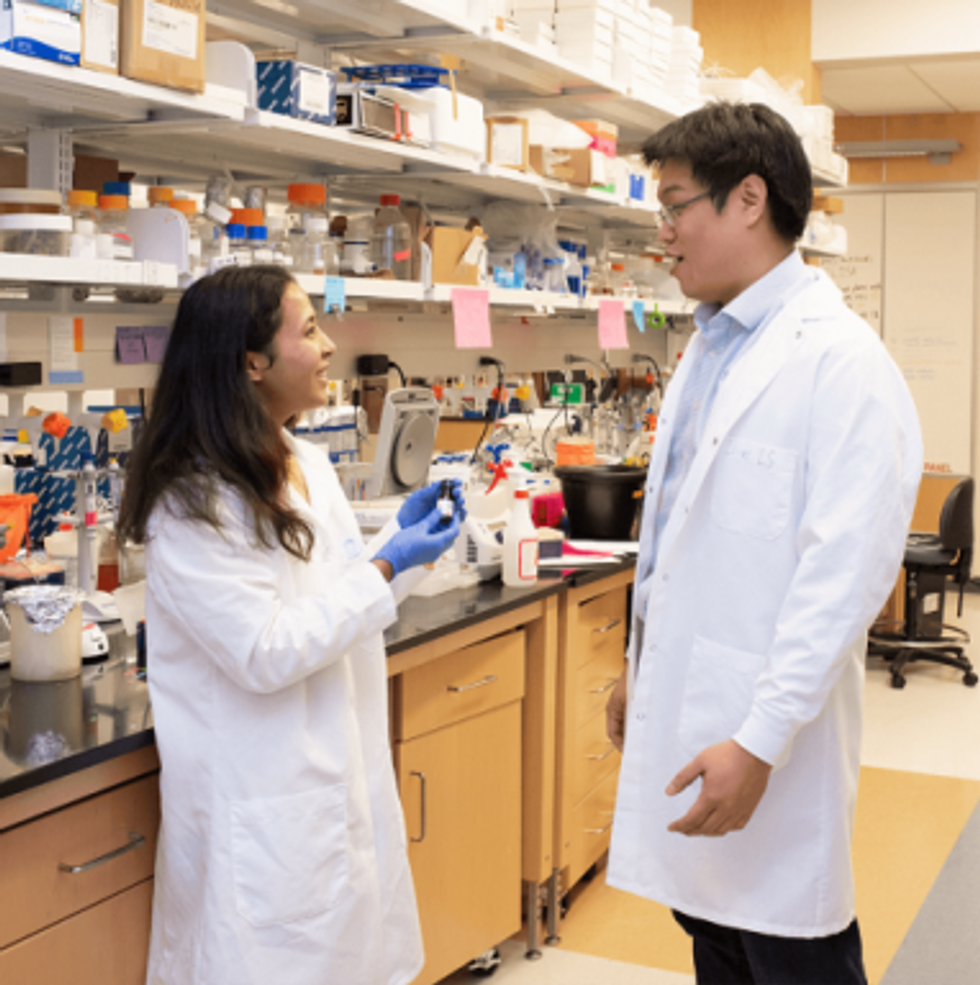
Suruchi Shrestha works in the lab with a colleague. In 2016, her research on antibodies for birth control was inspired by her own experience with side effects from an implanted hormonal IUD.
UNC - Chapel Hill
The sperm stays right where it met the antibody, never reaching the egg for fertilization. Eventually, and naturally, “Our vaginal system will just flush it out,” Shrestha explains.
“She showed in her early studies that [she] definitely got the sperm immotile, so they didn't move. And that was a really promising start,” says Jasmine Edelstein, a scientist with an expertise in antibody engineering who was not involved in this research. Shrestha’s team at UNC reproduced the effect in the sheep, notes Edelstein, who works at the startup Be Biopharma. In fact, Shrestha’s anti-sperm antibodies that caused the sperm to agglutinate, or clump together, were 99.9% effective when delivered topically to the sheep’s reproductive tracts.
The future
Going forward, Shrestha thinks the ideal approach would be delivering the antibodies through a vaginal ring. “We want to use it at the source of the spark,” Shrestha says, as opposed to less direct methods, such as taking a pill. The ring would dissolve after one month, she explains, “and then you get another one.”
Engineered to have a long shelf life, the anti-sperm antibody ring could be purchased without a prescription, and women could insert it themselves, without a doctor. “That's our hope, so that it is accessible,” Shrestha says. “Anybody can just go and grab it and not worry about pregnancy or unintended pregnancy.”
Her patented research has been licensed by several biotech companies for clinical trials. A number of Shrestha’s co-authors, including her lab advisor, Sam Lai, have launched a company, Mucommune, to continue developing the contraceptives based on these antibodies.
And, results from a small clinical trial run by researchers at Boston University Chobanian & Avedisian School of Medicine show that a dissolvable vaginal film with antibodies was safe when tested on healthy women of reproductive age. That same group of researchers earlier this year received a $7.2 million grant from the National Institute of Health for further research on monoclonal antibody-based contraceptives, which have also been shown to block transmission of viruses, like HIV.
“As the costs come down, this becomes a more realistic option potentially for women,” says Edelstein. “The impact could be tremendous.”
A New Test Aims to Objectively Measure Pain. It Could Help Legitimate Sufferers Access the Meds They Need.
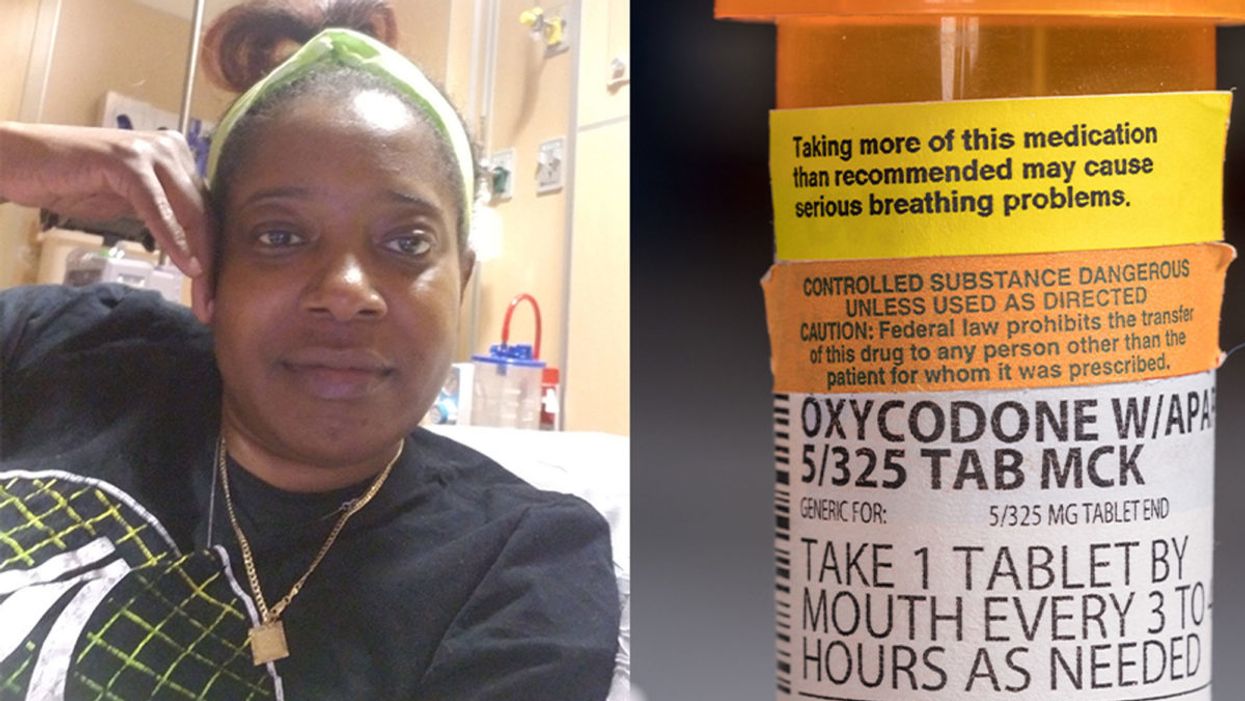
Sickle cell patient Bridgett Willkie found herself being labeled an addict when she sought an opioid prescription to control her pain.
"That throbbing you feel for the first minute after a door slams on your finger."
This is how Central Florida resident Bridgett Willkie describes the attacks of pain caused by her sickle cell anemia – a genetic blood disorder in which a patient's red blood cells become shaped like sickles and get stuck in blood vessels, thereby obstructing the flow of blood and oxygen.
"I found myself being labeled as an addict and I never was."
Willkie's lifelong battle with the condition has led to avascular necrosis in both of her shoulders, hips, knees and ankles. This means that her bone tissue is dying due to insufficient blood supply (sickle cell anemia is among the medical conditions that can decrease blood flow to one's bones).
"That adds to the pain significantly," she says. "Every time my heart beats, it hurts. And the pain moves. It follows the path of circulation. I liken it to a traffic jam in my veins."
For more than a decade, she received prescriptions for Oxycontin. Then, four years ago, her hematologist – who had been her doctor for 18 years – suffered a fatal heart attack. She says her longtime doctor's replacement lacked experience treating sickle cell patients and was uncomfortable writing her a prescription for opioids. What's more, this new doctor wanted to place her in a drug rehab facility.
"Because I refused to go, he stopped writing my scripts," she says. The ensuing three months were spent at home, detoxing. She describes the pain as unbearable. "Sometimes I just wanted to die."
One of the effects of the opioid epidemic is that many legitimate pain patients have seen their opioids significantly reduced or downright discontinued because of their doctors' fears of over-prescribing addictive medications.
"I found myself being labeled as an addict and I never was...Being treated like a drug-seeking patient is degrading and humiliating," says Willkie, who adds that when she is at the hospital, "it's exhausting arguing with the doctors...You dread them making their rounds because every day they come in talking about weaning you off your meds."
Situations such as these are fraught with tension between patients and doctors, who must remain wary about the risk of over-prescribing powerful and addictive medications. Adding to the complexity is that it can be very difficult to reliably assess a patient's level of physical pain.
However, this difficulty may soon decline, as Indiana University School of Medicine researchers, led by Dr. Alexander B. Niculescu, have reportedly devised a way to objectively assess physical pain by analyzing biomarkers in a patient's blood sample. The results of a study involving more than 300 participants were published earlier this year in the journal Molecular Psychiatry.
Niculescu – who is both a professor of psychiatry and medical neuroscience at the IU School of Medicine – explains that, when someone is in severe physical pain, a blood sample will show biomarkers related to intracellular adhesion and cell-signaling mechanisms. He adds that some of these biomarkers "have prior convergent evidence from animal or human studies for involvement in pain."
Aside from reliably measuring pain severity, Niculescu says blood biomarkers can measure the degree of one's response to treatment and also assess the risk of future recurrences of pain. He believes this new method's greatest benefit, however, might be the ability to identify a number of non-opioid medications that a particular patient is likely to respond to, based on his or her biomarker profile.
Clearly, such a method could be a gamechanger for pain patients and the professionals who treat them. As of yet, health workers have been forced to make crucial decisions based on their clinical impressions of patients; such impressions are invariably subjective. A method that enables people to prove the extent of their pain could remove the stigma that many legitimate pain patients face when seeking to obtain their needed medicine. It would also improve their chances of receiving sufficient treatment.
Niculescu says it's "theoretically possible" that there are some conditions which, despite being severe, might not reveal themselves through his testing method. But he also says that, "even if the same molecular markers that are involved in the pain process are not reflected in the blood, there are other indirect markers that should reflect the distress."
Niculescu expects his testing method will be available to the medical community at large within one to three years.
Willkie says she would welcome a reliable pain assessment method. Well-aware that she is not alone in her plight, she has more than 500 Facebook friends with sickle cell disease, and she says that "all of their opioid meds have been restricted or cut" as a result of the opioid crisis. Some now feel compelled to find their opioids "on the streets." She says she personally has never obtained opioids this way. Instead, she relies on marijuana to mitigate her pain.
Niculescu expects his testing method will be available to the medical community at large within one to three years: "It takes a while for things to translate from a lab setting to a commercial testing arena."
In the meantime, for Willkie and other patients, "we have to convince doctors and nurses that we're in pain."
Some people can eat red meat without negative health consequences, which may be due to variability between people's gut microbes.
In different countries' national dietary guidelines, red meats (beef, pork, and lamb) are often confined to a very small corner. Swedish officials, for example, advise the population to "eat less red and processed meat". Experts in Greece recommend consuming no more than four servings of red meat — not per week, but per month.
"Humans 100% rely on the microbes to digest this food."
Yet somehow, the matter is far from settled. Quibbles over the scientific evidence emerge on a regular basis — as in a recent BMJ article titled, "No need to cut red meat, say new guidelines." News headlines lately have declared that limiting red meat may be "bad advice," while carnivore diet enthusiasts boast about the weight loss and good health they've achieved on an all-meat diet. The wildly successful plant-based burgers? To them, a gimmick. The burger wars are on.
Nutrition science would seem the best place to look for answers on the health effects of specific foods. And on one hand, the science is rather clear: in large populations, people who eat more red meat tend to have more health problems, including cardiovascular disease, colorectal cancer, and other conditions. But this sort of correlational evidence fails to settle the matter once and for all; many who look closely at these studies cite methodological shortcomings and a low certainty of evidence.
Some scientists, meanwhile, are trying to cut through the noise by increasing their focus on the mechanisms: exactly how red meat is digested and the step-by-step of how this affects human health. And curiously, as these lines of evidence emerge, several of them center around gut microbes as active participants in red meat's ultimate effects on human health.
Dr. Stanley Hazen, researcher and medical director of preventive cardiology at Cleveland Clinic, was one of the first to zero in on gut microorganisms as possible contributors to the health effects of red meat. In looking for chemical compounds in the blood that could predict the future development of cardiovascular disease, his lab identified a molecule called trimethylamine-N-oxide (TMAO). Little by little, he and his colleagues began to gather both human and animal evidence that TMAO played a role in causing heart disease.
Naturally, they tried to figure out where the TMAO came from. Hazen says, "We found that animal products, and especially red meat, were a dietary source that, [along with] gut microbes, would generate this product that leads to heart disease development." They observed that the gut microbes were essential for making TMAO out of dietary compounds (like red meat) that contained its precursor, trimethylamine (TMA).
So in linking red meat to cardiovascular disease through TMAO, the surprising conclusion, says Hazen, was that, "Without a doubt, [the microbes] are the most important aspect of the whole pathway."
"I think it's just a matter of time [before] we will have therapeutic interventions that actually target our gut microbes, just like the way we take drugs that lower cholesterol levels."
Other researchers have taken an interest in different red-meat-associated health problems, like colorectal cancer and the inflammation that accompanies it. This was the mechanistic link tackled by the lab of professor Karsten Zengler of the UC San Diego Departments of Pediatrics and Bioengineering—and it also led straight back to the gut microbes.
Zengler and colleagues recently published a paper in Nature Microbiology that focused on the effects of a red meat carbohydrate (or sugar) called Neu5Gc.
He explains, "If you eat animal proteins in your diet… the bound sugars in your diet are cleaved off in your gut and they get recycled. Your own cells will not recognize between the foreign sugars and your own sugars, because they look almost identical." The unsuspecting human cells then take up these foreign sugars — spurring antibody production and creating inflammation.
Zengler showed, however, that gut bacteria use enzymes to cleave off the sugar during digestion, stopping the inflammation and rendering the sugar harmless. "There's no enzyme in the human body that can cleave this [sugar] off. Humans 100% rely on the microbes to digest this food," he says.
Both researchers are quick to caution that the health effects of diet are complex. Other work indicates, for example, that while intake of red meat can affect TMAO levels, so can intake of fish and seafood. But these new lines of evidence could help explain why some people, ironically, seem to be in perfect health despite eating a lot of red meat: their ideal frequency of meat consumption may depend on their existing community of gut microbes.
"It helps explain what accounts for inter-person variability," Hazen says.
These emerging mechanisms reinforce overall why it's prudent to limit red meat, just as the nutritional guidelines advised in the first place. But both Hazen and Zengler predict that interventions to buffer the effects of too many ribeyes may be just around the corner.
Zengler says, "Our idea is that you basically can help your own digestive system detoxify these inflammatory compounds in meat, if you continue eating red meat or you want to eat a high amount of red meat." A possibly strategy, he says, is to use specific pre- or probiotics to cultivate an inflammation-reducing gut microbial community.
Hazen foresees the emergence of drugs that act not on the human, but on the human's gut microorganisms. "I think it's just a matter of time [before] we will have therapeutic interventions that actually target our gut microbes, just like the way we take drugs that lower cholesterol levels."
He adds, "It's a matter of 'stay tuned', I think."