The future of non-hormonal birth control: Antibodies can stop sperm in their tracks

Many women want non-hormonal birth control. A 22-year-old's findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
Unwanted pregnancy can now be added to the list of preventions that antibodies may be fighting in the near future. For decades, really since the 1980s, engineered monoclonal antibodies have been knocking out invading germs — preventing everything from cancer to COVID. Sperm, which have some of the same properties as germs, may be next.
Not only is there an unmet need on the market for alternatives to hormonal contraceptives, the genesis for the original research was personal for the then 22-year-old scientist who led it. Her findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
The genesis
It’s Suruchi Shrestha’s research — published in Science Translational Medicine in August 2021 and conducted as part of her dissertation while she was a graduate student at the University of North Carolina at Chapel Hill — that could change the future of contraception for many women worldwide. According to a Guttmacher Institute report, in the U.S. alone, there were 46 million sexually active women of reproductive age (15–49) who did not want to get pregnant in 2018. With the overturning of Roe v. Wade this year, Shrestha’s research could, indeed, be life changing for millions of American women and their families.
Now a scientist with NextVivo, Shrestha is not directly involved in the development of the contraceptive that is based on her research. But, back in 2016 when she was going through her own problems with hormonal contraceptives, she “was very personally invested” in her research project, Shrestha says. She was coping with a long list of negative effects from an implanted hormonal IUD. According to the Mayo Clinic, those can include severe pelvic pain, headaches, acute acne, breast tenderness, irregular bleeding and mood swings. After a year, she had the IUD removed, but it took another full year before all the side effects finally subsided; she also watched her sister suffer the “same tribulations” after trying a hormonal IUD, she says.
For contraceptive use either daily or monthly, Shrestha says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
Shrestha unshelved antibody research that had been sitting idle for decades. It was in the late 80s that scientists in Japan first tried to develop anti-sperm antibodies for contraceptive use. But, 35 years ago, “Antibody production had not been streamlined as it is now, so antibodies were very expensive,” Shrestha explains. So, they shifted away from birth control, opting to focus on developing antibodies for vaccines.
Over the course of the last three decades, different teams of researchers have been working to make the antibody more effective, bringing the cost down, though it’s still expensive, according to Shrestha. For contraceptive use either daily or monthly, she says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
The problem
The problem with contraceptives for women, Shrestha says, is that all but a few of them are hormone-based or have other negative side effects. In fact, some studies and reports show that millions of women risk unintended pregnancy because of medical contraindications with hormone-based contraceptives or to avoid the risks and side effects. While there are about a dozen contraceptive choices for women, there are two for men: the condom, considered 98% effective if used correctly, and vasectomy, 99% effective. Neither of these choices are hormone-based.
On the non-hormonal side for women, there is the diaphragm which is considered only 87 percent effective. It works better with the addition of spermicides — Nonoxynol-9, or N-9 — however, they are detergents; they not only kill the sperm, they also erode the vaginal epithelium. And, there’s the non-hormonal IUD which is 99% effective. However, the IUD needs to be inserted by a medical professional, and it has a number of negative side effects, including painful cramping at a higher frequency and extremely heavy or “abnormal” and unpredictable menstrual flows.
The hormonal version of the IUD, also considered 99% effective, is the one Shrestha used which caused her two years of pain. Of course, there’s the pill, which needs to be taken daily, and the birth control ring which is worn 24/7. Both cause side effects similar to the other hormonal contraceptives on the market. The ring is considered 93% effective mostly because of user error; the pill is considered 99% effective if taken correctly.
“That’s where we saw this opening or gap for women. We want a safe, non-hormonal contraceptive,” Shrestha says. Compounding the lack of good choices, is poor access to quality sex education and family planning information, according to the non-profit Urban Institute. A focus group survey suggested that the sex education women received “often lacked substance, leaving them feeling unprepared to make smart decisions about their sexual health and safety,” wrote the authors of the Urban Institute report. In fact, nearly half (45%, or 2.8 million) of the pregnancies that occur each year in the US are unintended, reports the Guttmacher Institute. Globally the numbers are similar. According to a new report by the United Nations, each year there are 121 million unintended pregnancies, worldwide.
The science
The early work on antibodies as a contraceptive had been inspired by women with infertility. It turns out that 9 to 12 percent of women who are treated for infertility have antibodies that develop naturally and work against sperm. Shrestha was encouraged that the antibodies were specific to the target — sperm — and therefore “very safe to use in women.” She aimed to make the antibodies more stable, more effective and less expensive so they could be more easily manufactured.
Since antibodies tend to stick to things that you tell them to stick to, the idea was, basically, to engineer antibodies to stick to sperm so they would stop swimming. Shrestha and her colleagues took the binding arm of an antibody that they’d isolated from an infertile woman. Then, targeting a unique surface antigen present on human sperm, they engineered a panel of antibodies with as many as six to 10 binding arms — “almost like tongs with prongs on the tongs, that bind the sperm,” explains Shrestha. “We decided to add those grabbers on top of it, behind it. So it went from having two prongs to almost 10. And the whole goal was to have so many arms binding the sperm that it clumps it” into a “dollop,” explains Shrestha, who earned a patent on her research.
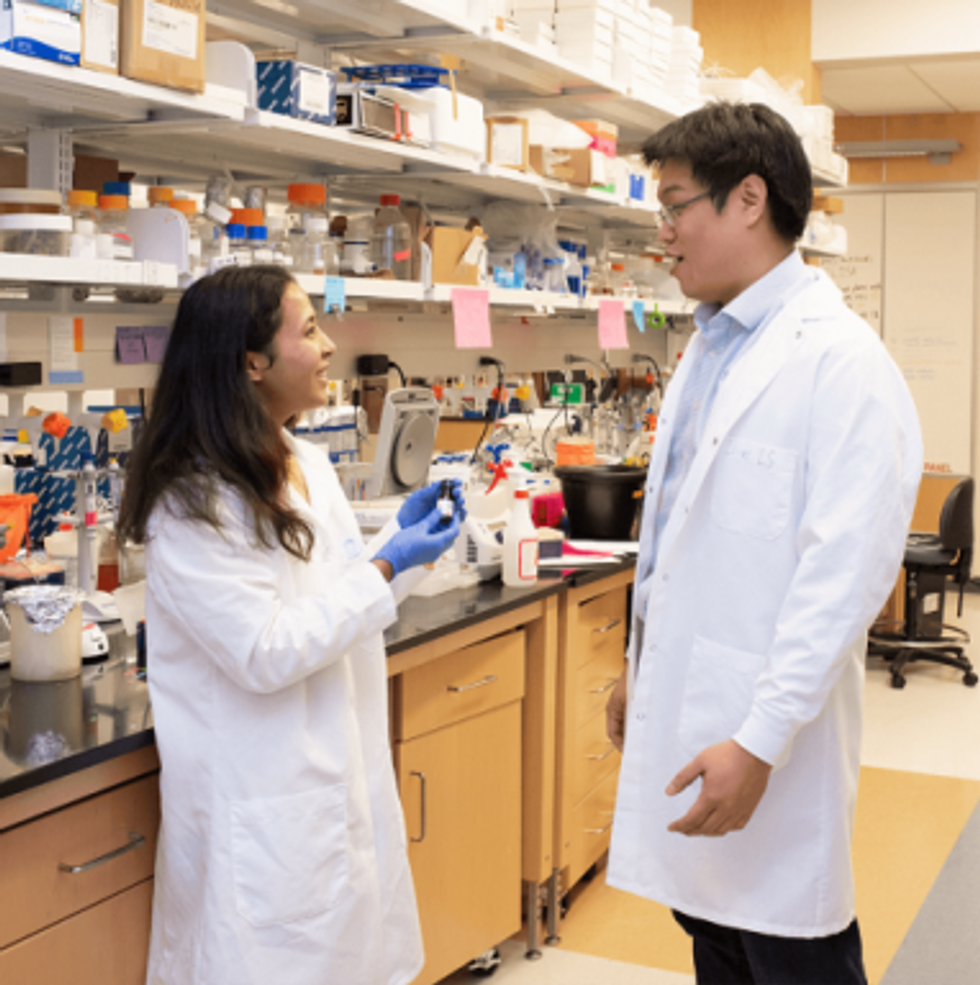
Suruchi Shrestha works in the lab with a colleague. In 2016, her research on antibodies for birth control was inspired by her own experience with side effects from an implanted hormonal IUD.
UNC - Chapel Hill
The sperm stays right where it met the antibody, never reaching the egg for fertilization. Eventually, and naturally, “Our vaginal system will just flush it out,” Shrestha explains.
“She showed in her early studies that [she] definitely got the sperm immotile, so they didn't move. And that was a really promising start,” says Jasmine Edelstein, a scientist with an expertise in antibody engineering who was not involved in this research. Shrestha’s team at UNC reproduced the effect in the sheep, notes Edelstein, who works at the startup Be Biopharma. In fact, Shrestha’s anti-sperm antibodies that caused the sperm to agglutinate, or clump together, were 99.9% effective when delivered topically to the sheep’s reproductive tracts.
The future
Going forward, Shrestha thinks the ideal approach would be delivering the antibodies through a vaginal ring. “We want to use it at the source of the spark,” Shrestha says, as opposed to less direct methods, such as taking a pill. The ring would dissolve after one month, she explains, “and then you get another one.”
Engineered to have a long shelf life, the anti-sperm antibody ring could be purchased without a prescription, and women could insert it themselves, without a doctor. “That's our hope, so that it is accessible,” Shrestha says. “Anybody can just go and grab it and not worry about pregnancy or unintended pregnancy.”
Her patented research has been licensed by several biotech companies for clinical trials. A number of Shrestha’s co-authors, including her lab advisor, Sam Lai, have launched a company, Mucommune, to continue developing the contraceptives based on these antibodies.
And, results from a small clinical trial run by researchers at Boston University Chobanian & Avedisian School of Medicine show that a dissolvable vaginal film with antibodies was safe when tested on healthy women of reproductive age. That same group of researchers earlier this year received a $7.2 million grant from the National Institute of Health for further research on monoclonal antibody-based contraceptives, which have also been shown to block transmission of viruses, like HIV.
“As the costs come down, this becomes a more realistic option potentially for women,” says Edelstein. “The impact could be tremendous.”
This “Absolutely Tireless” Researcher Made an Important Breakthrough for Cancer Patients
Theo Roth.
After months of looking at dead cells under a microscope, Theo Roth finally glimpsed what he had been hoping to see—flickers of green. His method was working.
"If we can go into the cell and add in new code and instructions, now we can give it whatever new functions we want."
When Roth joined the laboratory of Alex Marson at the University of California, San Francisco in June 2016, he set to work trying to figure out a new way to engineer human T cells, a type of white blood cell that's an important part of the immune system. If he succeeded, the resulting approach could make it easier and faster for scientists to develop and test cell and gene therapies, new treatments that involve genetically reprogramming the body's own cells.
For decades, researchers have been using engineered viruses to bestow human cells with new genetic characteristics. These so-called viral vectors "infect" human cells, transferring whatever new genetic material scientists put into them. The idea is that this new DNA could give T cells a boost to better fight diseases like cancer and HIV.
Several successful clinical trials have used virally-modified human T cells, and in fact, the U.S. Food and Drug Administration last year approved two such groundbreaking cancer gene therapies, Kymriah and Yescarta. But the process of genetically manipulating cells with viruses is expensive and time-consuming. In addition, viruses tend to randomly insert DNA with little predictability.
"What Theo wanted to do was to paste in big sequences of DNA at a targeted site without viruses," says Marson, an associate professor of microbiology and immunology. "That would have the benefit of being able to rewrite a specific site in the genome and do it flexibly and quickly without having to make a new virus for every site you want to manipulate."
Scientists have for a while been interested in non-viral engineering methods, but T cells are fragile and notoriously difficult to work with.
Previously, Marson's lab had collaborated with CRISPR pioneer Jennifer Doudna and her team at the University of California, Berkeley to use an electrical pulse together with CRISPR components to knock out certain genes. They also found some success with inserting very small pieces of DNA into a targeted site.
But Roth, a 27-year-old graduate student at UCSF pursuing MD and PhD degrees, was determined to figure out how to paste in much bigger sequences of genetic information. Marson says it was an "ambitious" goal. Scientists had tried before, but found that stuffing large chunks of DNA into T cells would quickly kill them.
"If we can go into the cell and add in new code and instructions, now we can give it whatever new functions we want," Roth says. "If you can add in new DNA sequences at the site that you want, then you have a much greater capacity to generate a cell that's going to be therapeutic or curative for a disease."
"He has already made his mark on the field."
So Roth began experimenting with hundreds of different variables a week, trying to find the right conditions to allow him to engineer T cells without the need for viruses. To know if the technique was working, Roth and his colleagues used a green fluorescent protein that would be expressed in cells that had successfully been modified.
"We went from having a lot of dead cells that didn't have any green to having maybe 1 percent of them being green," Roth says. "At that stage we got really excited."
After nearly a year of testing, he and collaborators found a combination of T cell ratios and DNA quantity mixed with CRISPR and zaps of electricity that seemed to work. These electrical pulses, called electroporation, deliver a jolt to cells that makes their membranes temporarily more permeable, allowing the CRISPR system to slip through. Once inside cells, CRISPR seeks out a specific place in the genome and makes a programmed, precise edit.
Roth and his colleagues used the approach to repair a genetic defect in T cells taken from children with a rare autoimmune disease and also to supercharge T cells so that they'd seek out and selectively kill human cancer cells while leaving healthy cells intact. In mice transplanted with human melanoma tissue, the edited T cells went to straight to the cancerous cells and attacked them. The findings were published in Nature in July.
Marson and Roth think even a relatively small number of modified T cells could be effective at treating some cancers, infections, and autoimmune diseases.
Roth is now working with the Parker Institute for Cancer Immunotherapy in San Francisco to engineer cells to treat a variety of cancers and hopefully commercialize his technique. Fred Ramsdell, vice president at the Parker Institute, says he's impressed by Roth's work. "He has already made his mark on the field."
Right now, there's a huge manufacturing backlog for viruses. If researchers want to start a clinical trial to test a new gene or cell therapy, they often have to wait a year to get the viruses they need.
"I think the biggest immediate impact is that it will lower the cost of a starting an early phase clinical trial."
Ramsdell says what Roth's findings allow researchers to do is engineer T cells quickly and more efficiently, cutting the time it takes to make them from several months to just a few weeks. That will allow researchers to develop and test several potential therapies in the lab at once.
"I think the biggest immediate impact is that it will lower the cost of a starting an early phase clinical trial," Roth says.
This isn't the first time Roth's work has been in the spotlight. As an undergraduate at Stanford University, he made significant contributions to traumatic brain injury research by developing a mouse model for observing the brain's cellular response to a concussion. He started the research, which was also published in Nature, the summer before entering college while he was an intern in Dorian McGavern's lab at the National Institutes of Health.
When Roth entered UCSF as a graduate student, his scientific interests shifted.
"It's definitely a big leap" from concussion research, says McGavern, who still keeps in touch with Roth. But he says he's not surprised about Roth's path. "He's absolutely tireless when it comes to the pursuit of science."
Roth says he's optimistic about the potential for gene and cell therapies to cure patients. "I want to try to figure out what one of the next therapies we should put into patients should be."
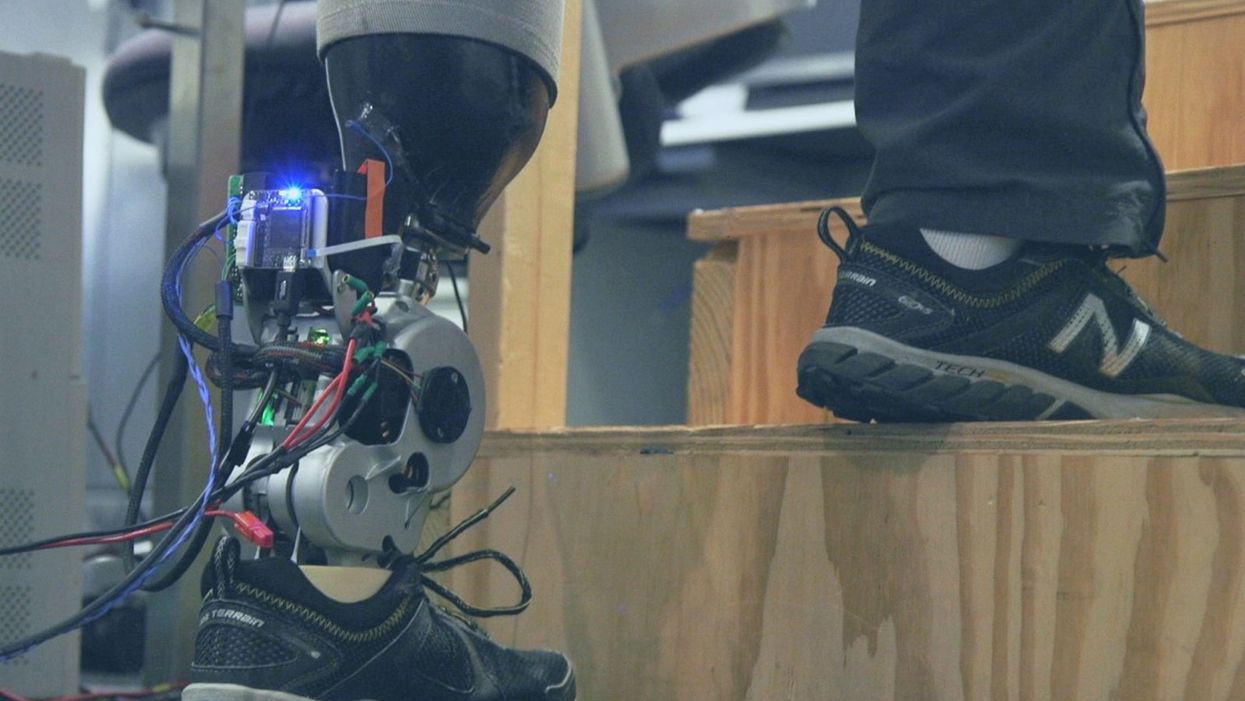
A patient with below-knee AMI amputation walks up the stairs.
"Here's a question for you," I say to our dinner guests, dodging a knowing glance from my wife. "Imagine a future in which you could surgically replace your legs with robotic substitutes that had all the functionality and sensation of their biological counterparts. Let's say these new legs would allow you to run all day at 20 miles per hour without getting tired. Would you have the surgery?"
Why are we so married to the arbitrary distinction between rehabilitating and augmenting?
Like most people I pose this question to, our guests respond with some variation on the theme of "no way"; the idea of undergoing a surgical procedure with the sole purpose of augmenting performance beyond traditional human limits borders on the unthinkable.
"Would your answer change if you had arthritis in your knees?" This is where things get interesting. People think differently about intervention when injury or illness is involved. The idea of a major surgery becomes more tractable to us in the setting of rehabilitation.
Consider the simplistic example of human walking speed. The average human walks at a baseline three miles per hour. If someone is only able to walk at one mile per hour, we do everything we can to increase their walking ability. However, to take a person who is already able to walk at three miles per hour and surgically alter their body so that they can walk twice as fast seems, to us, unreasonable.
What fascinates me about this is that the three-mile-per-hour baseline is set by arbitrary limitations of the healthy human body. If we ignore this reference point altogether, and consider that each case simply offers an improvement in walking ability, the line between augmentation and rehabilitation all but disappears. Why, then, are we so married to this arbitrary distinction between rehabilitating and augmenting? What makes us hold so tightly to baseline human function?
Where We Stand Now
As the functionality of advanced prosthetic devices continues to increase at an astounding rate, questions like these are becoming more relevant. Experimental prostheses, intended for the rehabilitation of people with amputation, are now able to replicate the motions of biological limbs with high fidelity. Neural interfacing technologies enable a person with amputation to control these devices with their brain and nervous system. Before long, synthetic body parts will outperform biological ones.
Our approach allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb.
Against this backdrop, my colleagues and I developed a methodology to improve the connection between the biological body and a synthetic limb. Our approach, known as the agonist-antagonist myoneural interface ("AMI" for short), enables us to reflect joint movement sensations from a prosthetic limb onto the human nervous system. In other words, the AMI allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb. The AMI involves a reimagining of the amputation surgery, so that the resultant residual limb is better suited to interact with a neurally-controlled prosthesis. In addition to increasing functionality, the AMI was designed with the primary goal of enabling adoption of a prosthetic limb as part of a patient's physical identity (known as "embodiment").
Early results have been remarkable. Patients with below-knee AMI amputation are better able to control an experimental prosthetic leg, compared to people who had their legs amputated in the traditional way. In addition, the AMI patients show increased evidence of embodiment. They identify with the device, and describe feeling as though it is part of them, part of self.
Where We're Going
True embodiment of robotic devices has the potential to fundamentally alter humankind's relationship with the built world. Throughout history, humans have excelled as tool builders. We innovate in ways that allow us to design and augment the world around us. However, tools for augmentation are typically external to our body identity; there is a clean line drawn between smart phone and self. As we advance our ability to integrate synthetic systems with physical identity, humanity will have the capacity to sculpt that very identity, rather than just the world in which it exists.
For this potential to be realized, we will need to let go of our reservations about surgery for augmentation. In reality, this shift has already begun. Consider the approximately 17.5 million surgical and minimally invasive cosmetic procedures performed in the United States in 2017 alone. Many of these represent patients with no demonstrated medical need, who have opted to undergo a surgical procedure for the sole purpose of synthetically enhancing their body. The ethical basis for such a procedure is built on the individual perception that the benefits of that procedure outweigh its costs.
At present, it seems absurd that amputation would ever reach this point. However, as robotic technology improves and becomes more integrated with self, the balance of cost and benefit will shift, lending a new perspective on what now seems like an unfathomable decision to electively amputate a healthy limb. When this barrier is crossed, we will collide head-on with the question of whether it is acceptable for a person to "upgrade" such an essential part of their body.
At a societal level, the potential benefits of physical augmentation are far-reaching. The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady, firefighters whose legs allow them to kick through walls, and athletes who never again have to worry about injury. It will be a world in which a teenage boy and his grandmother embark together on a four-hour sprint through the woods, for the sheer joy of it. It will be a world in which the human experience is fundamentally enriched, because our bodies, which play such a defining role in that experience, are truly malleable.
This is not to say that such societal benefits stand without potential costs. One justifiable concern is the misuse of augmentative technologies. We are all quite familiar with the proverbial supervillain whose nervous system has been fused to that of an all-powerful robot.
The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady.
In reality, misuse is likely to be both subtler and more insidious than this. As with all new technology, careful legislation will be necessary to work against those who would hijack physical augmentations for violent or oppressive purposes. It will also be important to ensure broad access to these technologies, to protect against further socioeconomic stratification. This particular issue is helped by the tendency of the cost of a technology to scale inversely with market size. It is my hope that when robotic augmentations are as ubiquitous as cell phones, the technology will serve to equalize, rather than to stratify.
In our future bodies, when we as a society decide that the benefits of augmentation outweigh the costs, it will no longer matter whether the base materials that make us up are biological or synthetic. When our AMI patients are connected to their experimental prosthesis, it is irrelevant to them that the leg is made of metal and carbon fiber; to them, it is simply their leg. After our first patient wore the experimental prosthesis for the first time, he sent me an email that provides a look at the immense possibility the future holds:
What transpired is still slowly sinking in. I keep trying to describe the sensation to people. Then this morning my daughter asked me if I felt like a cyborg. The answer was, "No, I felt like I had a foot."