Coronavirus Risk Calculators: What You Need to Know
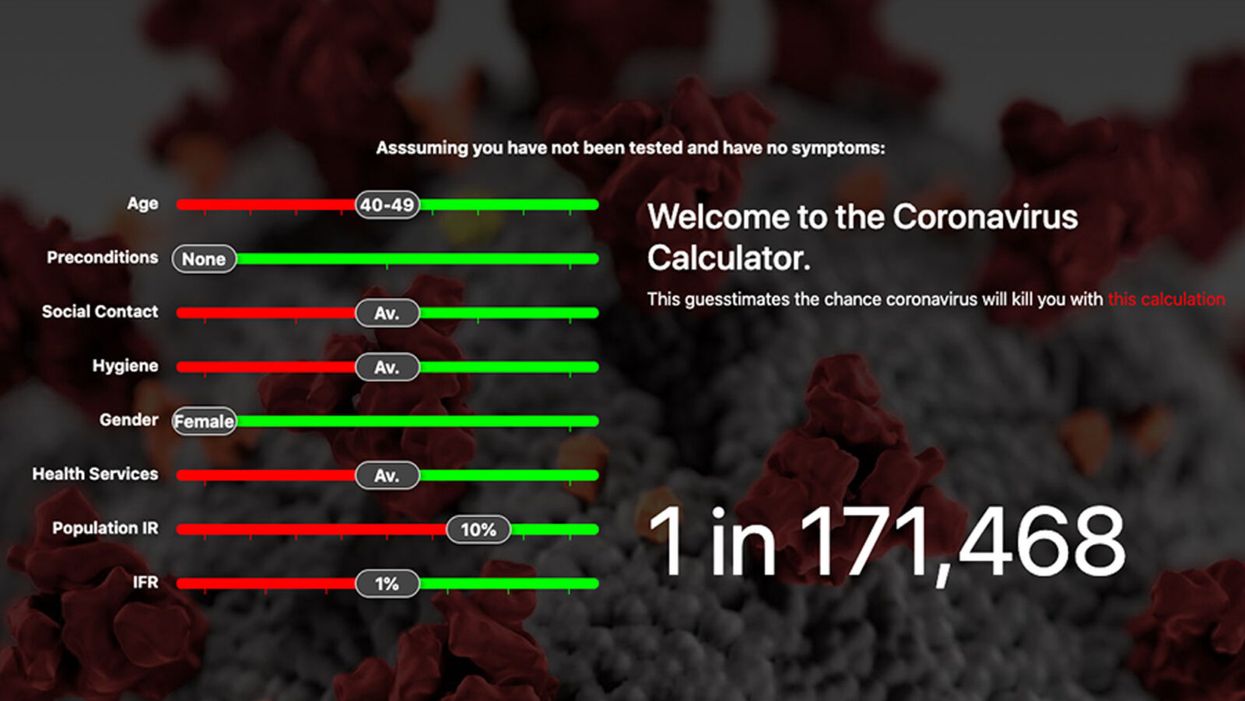
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.
New device finds breast cancer like earthquake detection
Jessica Fitzjohn, a postdoctoral fellow at the University of Canterbury, demonstrates the novel breast cancer screening device.
Mammograms are necessary breast cancer checks for women as they reach the recommended screening age between 40 and 50 years. Yet, many find the procedure uncomfortable. “I have large breasts, and to be able to image the full breast, the radiographer had to manipulate my breast within the machine, which took time and was quite uncomfortable,” recalls Angela, who preferred not to disclose her last name.
Breast cancer is the most widespread cancer in the world, affecting 2.3 million women in 2020. Screening exams such as mammograms can help find breast cancer early, leading to timely diagnosis and treatment. If this type of cancer is detected before the disease has spread, the 5-year survival rate is 99 percent. But some women forgo mammograms due to concerns about radiation or painful compression of breasts. Other issues, such as low income and a lack of access to healthcare, can also serve as barriers, especially for underserved populations.
Researchers at the University of Canterbury and startup Tiro Medical in Christchurch, New Zealand are hoping their new device—which doesn’t involve any radiation or compression of the breasts—could increase the accuracy of breast cancer screening, broaden access and encourage more women to get checked. They’re digging into clues from the way buildings move in an earthquake to help detect more cases of this disease.
Earthquake engineering inspires new breast cancer screening tech
What’s underneath a surface affects how it vibrates. Earthquake engineers look at the vibrations of swaying buildings to identify the underlying soil and tissue properties. “As the vibration wave travels, it reflects the stiffness of the material between that wave and the surface,” says Geoff Chase, professor of engineering at the University of Canterbury in Christchurch, New Zealand.
Chase is applying this same concept to breasts. Analyzing the surface motion of the breast as it vibrates could reveal the stiffness of the tissues underneath. Regions of high stiffness could point to cancer, given that cancerous breast tissue can be up to 20 times stiffer than normal tissue. “If in essence every woman’s breast is soft soil, then if you have some granite rocks in there, we’re going to see that on the surface,” explains Chase.
The earthquake-inspired device exceeds the 87 percent sensitivity of a 3D mammogram.
That notion underpins a new breast screening device, the brainchild of Chase. Women lie face down, with their breast being screened inside a circular hole and the nipple resting on a small disc called an actuator. The actuator moves up and down, between one and two millimeters, so there’s a small vibration, “almost like having your phone vibrate on your nipple,” says Jessica Fitzjohn, a postdoctoral fellow at the University of Canterbury who collaborated on the device design with Chase.
Cameras surrounding the device take photos of the breast surface motion as it vibrates. The photos are fed into image processing algorithms that convert them into data points. Then, diagnostic algorithms analyze those data points to find any differences in the breast tissue. “We’re looking for that stiffness contrast which could indicate a tumor,” Fitzjohn says.
A nascent yet promising technology
The device has been tested in a clinical trial of 14 women: one with healthy breasts and 13 with a tumor in one breast. The cohort was small but diverse, varying in age, breast volume and tumor size.
Results from the trial yielded a sensitivity rate, or the likelihood of correctly detecting breast cancer, of 85 percent. Meanwhile, the device’s specificity rate, or the probability of diagnosing healthy breasts, was 77 percent. By combining and optimizing certain diagnostic algorithms, the device reached between 92 and 100 percent sensitivity and between 80 and 86 percent specificity, which is comparable to the latest 3D mammogram technology. Called tomosynthesis, these 3D mammograms take a number of sharper, clearer and more detailed 3D images compared to the single 2D image of a conventional mammogram, and have a specificity score of 92 percent. Although the earthquake-inspired device’s specificity is lower, it exceeds the 87 percent sensitivity of a 3D mammogram.
The team hopes that cameras with better resolution can help improve the numbers. And with a limited amount of data in the first trial, the researchers are looking into funding for another clinical trial to validate their results on a larger cohort size.
Additionally, during the trial, the device correctly identified one woman’s breast as healthy, while her prior mammogram gave a false positive. The device correctly identified it as being healthy tissue. It was also able to capture the tiniest tumor at 7 millimeters—around a third of an inch or half as long as an aspirin tablet.
Diagnostic findings from the device are immediate.

When using the earthquake-inspired device, women lie face down, with their breast being screened inside circular holes.
University of Canterbury.
But more testing is needed to “prove the device’s ability to pick up small breast cancers less than 10 to 15 millimeters in size, as we know that finding cancers when they are small is the best way of improving outcomes,” says Richard Annand, a radiologist at Pacific Radiology in New Zealand. He explains that mammography already detects most precancerous lesions, so if the device will only be able to find large masses or lumps it won’t be particularly useful. While not directly involved in administering the clinical trial for the device, Annand was a director at the time for Canterbury Breastcare, where the trial occurred.
Meanwhile, Monique Gary, a breast surgical oncologist and medical director of the Grand View Health Cancer program in Pennsylvania, U.S., is excited to see new technologies advancing breast cancer screening and early detection. But she notes that the device may be challenging for “patients who are unable to lay prone, such as pregnant women as well as those who are differently abled, and this machine might exclude them.” She adds that it would also be interesting to explore how breast implants would impact the device’s vibrational frequency.
Diagnostic findings from the device are immediate, with the results available “before you put your clothes back on,” Chase says. The absence of any radiation is another benefit, though Annand considers it a minor edge “as we know the radiation dose used in mammography is minimal, and the advantages of having a mammogram far outweigh the potential risk of radiation.”
The researchers also conducted a separate ergonomic trial with 40 women to assess the device’s comfort, safety and ease of use. Angela was part of that trial and described the experience as “easy, quick, painless and required no manual intervention from an operator.” And if a person is uncomfortable being topless or having their breasts touched by someone else, “this type of device would make them more comfortable and less exposed,” she says.
While mammograms remain “the ‘gold standard’ in breast imaging, particularly screening, physicians need an option that can be used in combination with mammography.
Fitzjohn acknowledges that “at the moment, it’s quite a crude prototype—it’s just a block that you lie on.” The team prioritized function over form initially, but they’re now planning a few design improvements, including more cushioning for the breasts and the surface where the women lie on.
While mammograms remains “the ‘gold standard’ in breast imaging, particularly screening, physicians need an option that is good at excluding breast cancer when used in combination with mammography, has good availability, is easy to use and is affordable. There is the possibility that the device could fill this role,” Annand says.
Indeed, the researchers envision their new breast screening device as complementary to mammograms—a prescreening tool that could make breast cancer checks widely available. As the device is portable and doesn’t require specialized knowledge to operate, it can be used in clinics, pop-up screening facilities and rural communities. “If it was easily accessible, particularly as part of a checkup with a [general practitioner] or done in a practice the patient is familiar with, it may encourage more women to access this service,” Angela says. For those who find regular mammograms uncomfortable or can’t afford them, the earthquake-inspired device may be an option—and an even better one.
Broadening access could prompt more women to go for screenings, particularly younger women at higher risk of getting breast cancer because of a family history of the disease or specific gene mutations. “If we can provide an option for them then we can catch those cancers earlier,” Fitzjohn syas. “By taking screening to people, we’re increasing patient-centric care.”
With the team aiming to lower the device’s cost to somewhere between five and eight times less than mammography equipment, it would also be valuable for low-to-middle-income nations that are challenged to afford the infrastructure for mammograms or may not have enough skilled radiologists.
For Fitzjohn, the ultimate goal is to “increase equity in breast screening and catch cancer early so we have better outcomes for women who are diagnosed with breast cancer.”
Stronger psychedelics that rewire the brain, with Doug Drysdale
Today's podcast episode features Doug Drysdale, CEO of Cybin, a company that is leading innovations in psilocybin, mushrooms that may help people with anxiety and depression.
A promising development in science in recent years has been the use technology to optimize something natural. One-upping nature's wisdom isn't easy. In many cases, we haven't - and maybe we can't - figure it out. But today's episode features a fascinating example: using tech to optimize psychedelic mushrooms.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
These mushrooms have been used for religious, spiritual and medicinal purposes for thousands of years, but only in the past several decades have scientists brought psychedelics into the lab to enhance them and maximize their therapeutic value.
Today’s podcast guest, Doug Drysdale, is doing important work to lead this effort. Drysdale is the CEO of a company called Cybin that has figured out how to make psilocybin more potent, so it can be administered in smaller doses without side effects.
The natural form of psilocybin has been studied increasingly in the realm of mental health. Taking doses of these mushrooms appears to help people with anxiety and depression by spurring the development of connections in the brain, an example of neuroplasticity. The process basically shifts the adult brain from being fairly rigid like dried clay into a malleable substance like warm wax - the state of change that's constantly underway in the developing brains of children.
Neuroplasticity in adults seems to unlock some of our default ways of of thinking, the habitual thought patterns that’ve been associated with various mental health problems. Some promising research suggests that psilocybin causes a reset of sorts. It makes way for new, healthier thought patterns.
So what is Drysdale’s secret weapon to bring even more therapeutic value to psilocybin? It’s a process called deuteration. It focuses on the hydrogen atoms in psilocybin. These atoms are very light and don’t stick very well to carbon, which is another atom in psilocybin. As a result, our bodies can easily breaks down the bonds between the hydrogen and carbon atoms. For many people, that means psilocybin gets cleared from the body too quickly, before it can have a therapeutic benefit.
In deuteration, scientists do something simple but ingenious: they replace the hydrogen atoms with a molecule called deuterium. It’s twice as heavy as hydrogen and forms tighter bonds with the carbon. Because these pairs are so rock-steady, they slow down the rate at which psilocybin is metabolized, so it has more sustained effects on our brains.
Cybin isn’t Drysdale’s first go around at this - far from it. He has over 30 years of experience in the healthcare sector. During this time he’s raised around $4 billion of both public and private capital, and has been named Ernst and Young Entrepreneur of the Year. Before Cybin, he was the founding CEO of a pharmaceutical company called Alvogen, leading it from inception to around $500 million in revenues, across 35 countries. Drysdale has also been the head of mergers and acquisitions at Actavis Group, leading 15 corporate acquisitions across three continents.
In this episode, Drysdale walks us through the promising research of his current company, Cybin, and the different therapies he’s developing for anxiety and depression based not just on psilocybin but another psychedelic compound found in plants called DMT. He explains how they seem to have such powerful effects on the brain, as well as the potential for psychedelics to eventually support other use cases, including helping us strive toward higher levels of well-being. He goes on to discuss his views on mindfulness and lifestyle factors - such as optimal nutrition - that could help bring out hte best in psychedelics.
Show links:
Doug Drysdale full bio
Doug Drysdale twitter
Cybin website
Cybin development pipeline
Cybin's promising phase 2 research on depression
Johns Hopkins psychedelics research and psilocybin research
Mets owner Steve Cohen invests in psychedelic therapies

Doug Drysdale, CEO of Cybin

