Coronavirus Risk Calculators: What You Need to Know
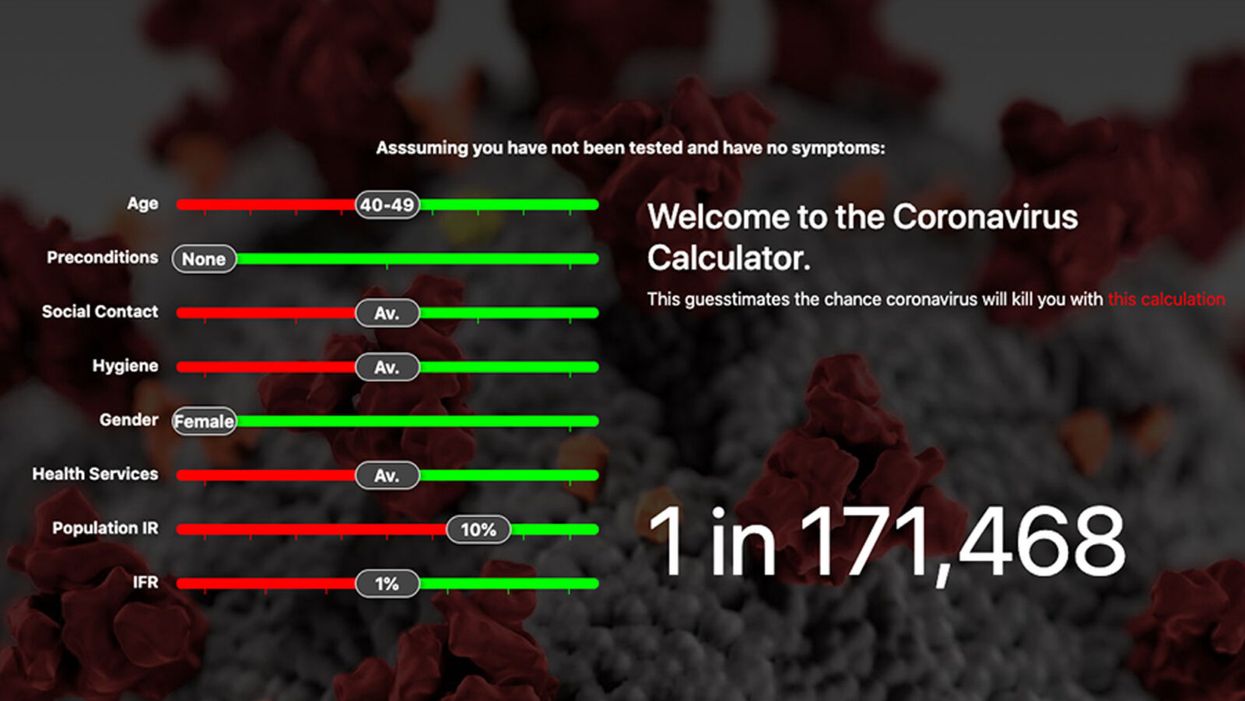
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.
Elaine Kamil had just returned home after a few days of business meetings in 2013 when she started having chest pains. At first Kamil, then 66, wasn't worried—she had had some chest pain before and recently went to a cardiologist to do a stress test, which was normal.
"I can't be having a heart attack because I just got checked," she thought, attributing the discomfort to stress and high demands of her job. A pediatric nephrologist at Cedars-Sinai Hospital in Los Angeles, she takes care of critically ill children who are on dialysis or are kidney transplant patients. Supporting families through difficult times and answering calls at odd hours is part of her daily routine, and often leaves her exhausted.
She figured the pain would go away. But instead, it intensified that night. Kamil's husband drove her to the Cedars-Sinai hospital, where she was admitted to the coronary care unit. It turned out she wasn't having a heart attack after all. Instead, she was diagnosed with a much less common but nonetheless dangerous heart condition called takotsubo syndrome, or broken heart syndrome.
A heart attack happens when blood flow to the heart is obstructed—such as when an artery is blocked—causing heart muscle tissue to die. In takotsubo syndrome, the blood flow isn't blocked, but the heart doesn't pump it properly. The heart changes its shape and starts to resemble a Japanese fishing device called tako-tsubo, a clay pot with a wider body and narrower mouth, used to catch octopus.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks," explains Noel Bairey Merz, the cardiologist at Cedar Sinai who Kamil went to see after she was discharged.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks."
But even though the heart isn't permanently damaged, mortality rates due to takotsubo syndrome are comparable to those of a heart attack, Merz notes—about 4-5% of patients die from the attack, and 20% within the next five years. "It's as bad as a heart attack," Merz says—only it's much less known, even to doctors. The condition affects only about 1% of people, and there are around 15,000 new cases annually. It's diagnosed using a cardiac ventriculogram, an imaging test that allows doctors to see how the heart pumps blood.
Scientists don't fully understand what causes Takotsubo syndrome, but it usually occurs after extreme emotional or physical stress. Doctors think it's triggered by a so-called catecholamine storm, a phenomenon in which the body releases too much catecholamines—hormones involved in the fight-or-flight response. Evolutionarily, when early humans lived in savannas or forests and had to either fight off predators or flee from them, these hormones gave our ancestors the needed strength and stamina to take either action. Released by nerve endings and by the adrenal glands that sit on top of the kidneys, these hormones still flood our bodies in moments of stress, but an overabundance of them could sometimes be damaging.

Elaine Kamil
A recent study by scientists at Harvard Medical School linked increased risk of takotsubo to higher activity in the amygdala, a brain region responsible for emotions that's involved in responses to stress. The scientists believe that chronic stress makes people more susceptible to the syndrome. Notably, one small study suggested that the number of Takotsubo cases increased during the COVID-19 pandemic.
There are no specific drugs to treat takotsubo, so doctors rely on supportive therapies, which include medications typically used for high blood pressure and heart failure. In most cases, the heart returns to its normal shape within a few weeks. "It's a spontaneous recovery—the catecholamine storm is resolved, the injury trigger is removed and the heart heals itself because our bodies have an amazing healing capacity," Merz says. It also helps that tissues remain intact. 'The heart cells don't die, they just aren't functioning properly for some time."
That's the good news. The bad news is that takotsubo is likely to strike again—in 5-20% of patients the condition comes back, sometimes more severe than before.
That's exactly what happened to Kamil. After getting her diagnosis in 2013, she realized that she actually had a previous takotsubo episode. In 2010, she experienced similar symptoms after her son died. "The night after he died, I was having severe chest pain at night, but I was too overwhelmed with grief to do anything about it," she recalls. After a while, the pain subsided and didn't return until three years later.
For weeks after her second attack, she felt exhausted, listless and anxious. "You lose confidence in your body," she says. "You have these little twinges on your chest, or if you start having arrhythmia, and you wonder if this is another episode coming up. It's really unnerving because you don't know how to read these cues." And that's very typical, Merz says. Even when the heart muscle appears to recover, patients don't return to normal right away. They have shortens of breath, they can't exercise, and they stay anxious and worried for a while.
Women over the age of 50 are diagnosed with takotsubo more often than other demographics. However, it happens in men too, although it typically strikes after physical stress, such as a triathlon or an exhausting day of cycling. Young people can also get takotsubo. Older patients are hospitalized more often, but younger people tend to have more severe complications. It could be because an older person may go for a jog while younger one may run a marathon, which would take a stronger toll on the body of a person who's predisposed to the condition.
Notably, the emotional stressors don't always have to be negative—the heart muscle can get out of shape from good emotions, too. "There have been case reports of takotsubo at weddings," Merz says. Moreover, one out of three or four takotsubo patients experience no apparent stress, she adds. "So it could be that it's not so much the catecholamine storm itself, but the body's reaction to it—the physiological reaction deeply embedded into out physiology," she explains.
Merz and her team are working to understand what makes people predisposed to takotsubo. They think a person's genetics play a role, but they haven't yet pinpointed genes that seem to be responsible. Genes code for proteins, which affect how the body metabolizes various compounds, which, in turn, affect the body's response to stress. Pinning down the protein involved in takotsubo susceptibility would allow doctors to develop screening tests and identify those prone to severe repeating attacks. It will also help develop medications that can either prevent it or treat it better than just waiting for the body to heal itself.
Researchers at the Imperial College London recently found that elevated levels of certain types of microRNAs—molecules involved in protein production—increase the chances of developing takotsubo.
In one study, researchers tried treating takotsubo in mice with a drug called suberanilohydroxamic acid, or SAHA, typically used for cancer treatment. The drug improved cardiac health and reversed the broken heart in rodents. It remains to be seen if the drug would have a similar effect on humans. But identifying a drug that shows promise is progress, Merz says. "I'm glad that there's research in this area."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
What to Know about the Fast-Spreading Delta Variant
A highly contagious form of the coronavirus known as the Delta variant is spreading rapidly and becoming increasingly prevalent around the world. First identified in India in December, Delta has now been identified in 111 countries.
In the United States, the variant now accounts for 83% of sequenced COVID-19 cases, said Rochelle Walensky, director of the Centers for Disease Control and Prevention, at a July 20 Senate hearing. In May, Delta was responsible for just 3% of U.S. cases. The World Health Organization projects that Delta will become the dominant variant globally over the coming months.
So, how worried should you be about the Delta variant? We asked experts some common questions about Delta.
What is a variant?
To understand Delta, it's helpful to first understand what a variant is. When a virus infects a person, it gets into your cells and makes a copy of its genome so it can replicate and spread throughout your body.
In the process of making new copies of itself, the virus can make a mistake in its genetic code. Because viruses are replicating all the time, these mistakes — also called mutations — happen pretty often. A new variant emerges when a virus acquires one or more new mutations and starts spreading within a population.
There are thousands of SARS-CoV-2 variants, but most of them don't substantially change the way the virus behaves. The variants that scientists are most interested in are known as variants of concern. These are versions of the virus with mutations that allow the virus to spread more easily, evade vaccines, or cause more severe disease.
"The vast majority of the mutations that have accumulated in SARS-CoV-2 don't change the biology as far as we're concerned," said Jennifer Surtees, a biochemist at the University of Buffalo who's studying the coronavirus. "But there have been a handful of key mutations and combinations of mutations that have led to what we're now calling variants of concern."
One of those variants of concern is Delta, which is now driving many new COVID-19 infections.
Why is the Delta variant so concerning?
"The reason why the Delta variant is concerning is because it's causing an increase in transmission," said Alba Grifoni, an infectious disease researcher at the La Jolla Institute for Immunology. "The virus is spreading faster and people — particularly those who are not vaccinated yet — are more prone to exposure."
The Delta variant has a few key mutations that make it better at attaching to our cells and evading the neutralizing antibodies in our immune system. These mutations have changed the virus enough to make it more than twice as contagious as the original SARS-CoV-2 virus that emerged in Wuhan and about 50% more contagious than the Alpha variant, previously known as B.1.1.7, or the U.K. variant.
These mutations were previously seen in other variants on their own, but it's their combination that makes Delta so much more infectious.
Do vaccines work against the Delta variant?
The good news is, the COVID-19 vaccines made by AstraZeneca, Johnson & Johnson, Moderna, and Pfizer still work against the Delta variant. They remain more than 90% effective at preventing hospitalizations and death due to Delta. While they're slightly less protective against disease symptoms, they're still very effective at preventing severe illness caused by the Delta variant.
"They're not as good as they were against the prior strains, but they're holding up pretty well," said Eric Topol, a physician and director of the Scripps Translational Research Institute, during a July 19 briefing for journalists.
Because Delta is better at evading our immune systems, it's likely causing more breakthrough infections — COVID-19 cases in people who are vaccinated. However, breakthrough infections were expected before the Delta variant became widespread. No vaccine is 100% effective, so breakthrough infections can happen with other vaccines as well. Experts say the COVID-19 vaccines are still working as expected, even if breakthrough infections occur. The majority of these infections are asymptomatic or cause only mild symptoms.
Should vaccinated people worry about the Delta variant?
Vaccines train our immune systems to protect us against infection. They do this by spurring the production of antibodies, which stick around in our bodies to help fight off a particular pathogen in case we ever come into contact with it.
But even if the new Delta variant slips past our neutralizing antibodies, there's another component of our immune system that can help overtake the virus: T cells. Studies are showing that the COVID-19 vaccines also galvanize T cells, which help limit disease severity in people who have been vaccinated.
"While antibodies block the virus and prevent the virus from infecting cells, T cells are able to attack cells that have already been infected," Grifoni said. In other words, T cells can prevent the infection from spreading to more places in the body. A study published July 1 by Grifoni and her colleagues found that T cells were still able to recognize mutated forms of the virus — further evidence that our current vaccines are effective against Delta.
Can fully vaccinated people spread the Delta variant?
Previously, scientists believed it was unlikely for fully vaccinated individuals with asymptomatic infections to spread Covid-19. But the Delta variant causes the virus to make so many more copies of itself inside the body, and high viral loads have been found in the respiratory tracts of people who are fully vaccinated. This suggests that vaccinated people may be able to spread the Delta variant to some degree.
If you have COVID-19 symptoms, even if you're fully vaccinated, you should get tested and isolate from friends and family because you could spread the virus.
What risk does Delta pose to unvaccinated people?
The Delta variant is behind a surge in cases in communities with low vaccination rates, and unvaccinated Americans currently account for 97% of hospitalizations due to COVID-19, according to Walensky. The best thing you can do right now to prevent yourself from getting sick is to get vaccinated.
Gigi Gronvall, an immunologist and senior scholar at the Johns Hopkins Center for Health Security, said in this week's "Making Sense of Science" podcast that it's especially important to get all required doses of the vaccine in order to have the best protection against the Delta variant. "Even if it's been more than the allotted time that you were told to come back and get the second, there's no time like the present," she said.
With more than 3.6 billion COVID-19 doses administered globally, the vaccines have been shown to be incredibly safe. Serious adverse effects are rare, although scientists continue to monitor for them.
Being vaccinated also helps prevent the emergence of new and potentially more dangerous variants. Viruses need to infect people in order to replicate, and variants emerge because the virus continues to infect more people. More infections create more opportunities for the virus to acquire new mutations.
Surtees and others worry about a scenario in which a new variant emerges that's even more transmissible or resistant to vaccines. "This is our window of opportunity to try to get as many people vaccinated as possible and get people protected so that so that the virus doesn't evolve to be even better at infecting people," she said.
Does Delta cause more severe disease?
While hospitalizations and deaths from COVID-19 are increasing again, it's not yet clear whether Delta causes more severe illness than previous strains.
How can we protect unvaccinated children from the Delta variant?
With children 12 and under not yet eligible for the COVID-19 vaccine, kids are especially vulnerable to the Delta variant. One way to protect unvaccinated children is for parents and other close family members to get vaccinated.
It's also a good idea to keep masks handy when going out in public places. Due to risk Delta poses, the American Academy of Pediatrics issued new guidelines July 19 recommending that all staff and students over age 2 wear face masks in school this fall, even if they have been vaccinated.
Parents should also avoid taking their unvaccinated children to crowded, indoor locations and make sure their kids are practicing good hand-washing hygiene. For children younger than 2, limit visits with friends and family members who are unvaccinated or whose vaccination status is unknown and keep up social distancing practices while in public.
While there's no evidence yet that Delta increases disease severity in children, parents should be mindful that in some rare cases, kids can get a severe form of the disease.
"We're seeing more children getting sick and we're seeing some of them get very sick," Surtees said. "Those children can then pass on the virus to other individuals, including people who are immunocompromised or unvaccinated."