Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
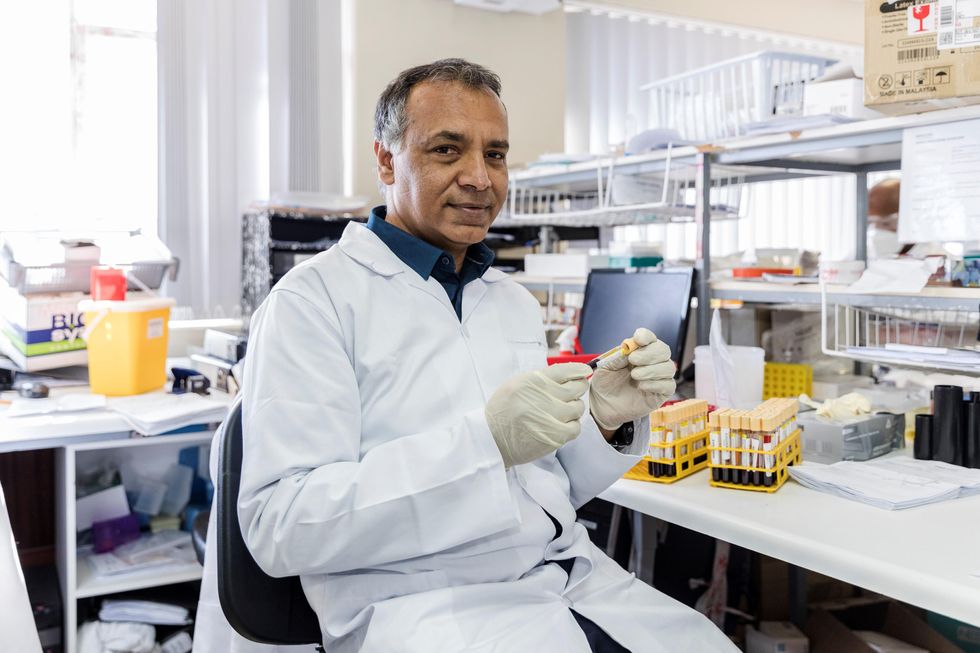
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Could epigenetic reprogramming reverse aging?
A range of strategies are being explored to reprogram the body's cells to an earlier state. Most scientists aren't betting on a new fountain of youth just yet - but, in theory, epigenetic reprogramming is a recipe for self-renewal.
Ten thousand years ago, the average human spent a maximum of 30 years on Earth. Despite the glory of Ancient Greece and the Roman Empire, most of their inhabitants didn’t surpass the age of 35. Between the 1500s and 1800, life expectancy (at least in Europe) fluctuated between 30 and 40 years.
Public health advancements like control of infectious diseases, better diet and clean sanitation, as well as social improvements have made it possible for human lifespans to double since 1800. Although lifespan differs widely today from country to country according to socioeconomic health, the average has soared to 73.2 years.
But this may turn out to be on the low side if epigenetic rejuvenation fulfills its great promise: to reverse aging, perhaps even completely. Epigenetic rejuvenation, or partial reprogramming, is the process by which a set of therapies are trying to manipulate epigenetics – how various changes can affect our genes – and the Yamanaka factors. These Yamanaka factors are a group of proteins that can convert any cell of the body into pluripotent stem cells, a group of cells that can turn into brand new cells, such as those of the brain or skin. At least in theory, it could be a recipe for self-renewal.
“Partial reprogramming tries to knock a few years off of people’s biological age, while preserving their original cell identity and function,” says Yuri Deigin, cofounder and director of YouthBio Therapeutics, a longevity startup utilizing partial reprogramming to develop gene therapies aimed at the renewal of epigenetic profiles. YouthBio plans to experiment with injecting these gene therapies into target organs. Once the cargo is delivered, a specific small molecule will trigger gene expression and rejuvenate those organs.
“Our ultimate mission is to find the minimal number of tissues we would need to target to achieve significant systemic rejuvenation,” Deigin says. Initially, YouthBio will apply these therapies to treat age-related conditions. Down the road, though, their goal is for everyone to get younger. “We want to use them for prophylaxis, which is rejuvenation that would lower disease risk,” Deigin says.
Epigenetics has swept the realm of biology off its feet over the last decade. We now know that we can switch genes on and off by tweaking the chemical status quo of the DNA’s local environment. "Epigenetics is a fascinating and important phenomenon in biology,’’ says Henry Greely, a bioethicist at Stanford Law School. Greely is quick to stress that this kind of modulation (turning genes on and off and not the entire DNA) happens all the time. “When you eat and your blood sugar goes up, the gene in the beta cells of your pancreas that makes insulin is turned on or up. Almost all medications are going to have effects on epigenetics, but so will things like exercise, food, and sunshine.”
Can intentional control over epigenetic mechanisms lead to novel and useful therapies? “It is a very plausible scenario,” Greely says, though a great deal of basic research into epigenetics is required before it becomes a well-trodden way to stay healthy or treat disease. Whether these therapies could cause older cells to become younger in ways that have observable effects is “far from clear,” he says. “Historically, betting on someone’s new ‘fountain of youth’ has been a losing strategy.”
The road to de-differentiation, the process by which cells return to an earlier state, is not paved with roses; de-differentiate too much and you may cause pathology and even death.
In 2003 researchers finished sequencing the roughly 3 billion letters of DNA that make up the human genome. The human genome sequencing was hailed as a vast step ahead in our understanding of how genetics contribute to diseases like cancer or to developmental disorders. But for Josephine Johnston, director of research and research scholar at the Hastings Center, the hype has not lived up to its initial promise. “Other than some quite effective tests to diagnose certain genetic conditions, there isn't a radical intervention that reverses things yet,” Johnston says. For her, this is a testament to the complexity of biology or at least to our tendency to keep underestimating it. And when it comes to epigenetics specifically, Johnston believes there are some hard questions we need to answer before we can safely administer relevant therapies to the population.
“You'd need to do longitudinal studies. You can't do a study and look at someone and say they’re safe only six months later,” Johnston says. You can’t know long-term side effects this way, and how will companies position their therapies on the market? Are we talking about interventions that target health problems, or life enhancements? “If you describe something as a medical intervention, it is more likely to be socially acceptable, to attract funding from governments and ensure medical insurance, and to become a legitimate part of medicine,” she says.
Johnston’s greatest concerns are of the philosophical and ethical nature. If we’re able to use epigenetic reprogramming to double the human lifespan, how much of the planet’s resources will we take up during this long journey? She believes we have a moral obligation to make room for future generations. “We should also be honest about who's actually going to afford such interventions; they would be extraordinarily expensive and only available to certain people, and those are the people who would get to live longer, healthier lives, and the rest of us wouldn't.”
That said, Johnston agrees there is a place for epigenetic reprogramming. It could help people with diseases that are caused by epigenetic problems such as Fragile X syndrome, Prader-Willi syndrome and various cancers.
Zinaida Good, a postdoctoral fellow at Stanford Cancer Institute, says these problems are still far in the future. Any change will be incremental. “Thinking realistically, there’s not going to be a very large increase in lifespan anytime soon,” she says. “I would not expect something completely drastic to be invented in the next 5 to 10 years. ”
Good won’t get any such treatment for herself until it’s shown to be effective and safe. Nature has programmed our bodies to resist hacking, she says, in ways that could undermine any initial benefits to longevity. A preprint that is not yet peer-reviewed reports cellular reprogramming may lead to premature death due to liver and intestinal problems, and using the Yamanaka factors may have the potential to cause cancer, at least in animal studies.
“Side effects are an open research question that all partial reprogramming companies and labs are trying to address,” says Deigin. The road to de-differentiation, the process by which cells return to an earlier state, is not paved with roses; de-differentiate too much and you may cause pathology and even death. Deigin is exploring other, less risky approaches. “One way is to look for novel factors tailored toward rejuvenation rather than de-differentiation.” Unlike Yamanaka factors, such novel factors would never involve taking a given cell to a state in which it could turn cancerous, according to Deigin.
An example of a novel factor that could lower the risk of cancer is artificially introducing mRNA molecules, or molecules carrying the genetic information necessary to make proteins, by using electricity to penetrate the cell instead of a virus. There is also chemical-based reprogramming, in which chemicals are applied to convert regular cells into pluripotent cells. This approach is currently effective only for mice though.
“The search for novel factors tailored toward rejuvenation without de-differentiation is an ongoing research and development effort by several longevity companies, including ours,” says Deigin.
He isn't disclosing the details of his own company’s underlying approach to lowering the risk, but he’s hopeful that something will eventually end up working in humans. Yet another challenge is that, partly because of the uncertainties, the FDA hasn’t seen fit to approve a single longevity therapy. But with the longevity market projected to soar to $600 billion by 2025, Deigin says naysayers are clinging irrationally to the status quo. “Thankfully, scientific progress is moved forward by those who bet for something while disregarding the skeptics - who, in the end, are usually proven wrong.”
Podcast: The Friday Five Weekly Roundup in Health Research
In this week's Friday Five, a new face mask can detect Covid and send an alert to your phone. Plus, promising research for a breakthrough drug to treat schizophrenia, an AI tool that can create new proteins, progress on a longevity drug - and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five:
- A new mask can detect Covid and send an alert to your phone
- More promising research for a breakthrough drug to treat schizophrenia
- AI tool can create new proteins
- Connections between an unhealthy gut and breast cancer
- Progress on the longevity drug, rapamycin
And an honorable mention this week: Certain exercises may benefit some types of memory more than others