Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

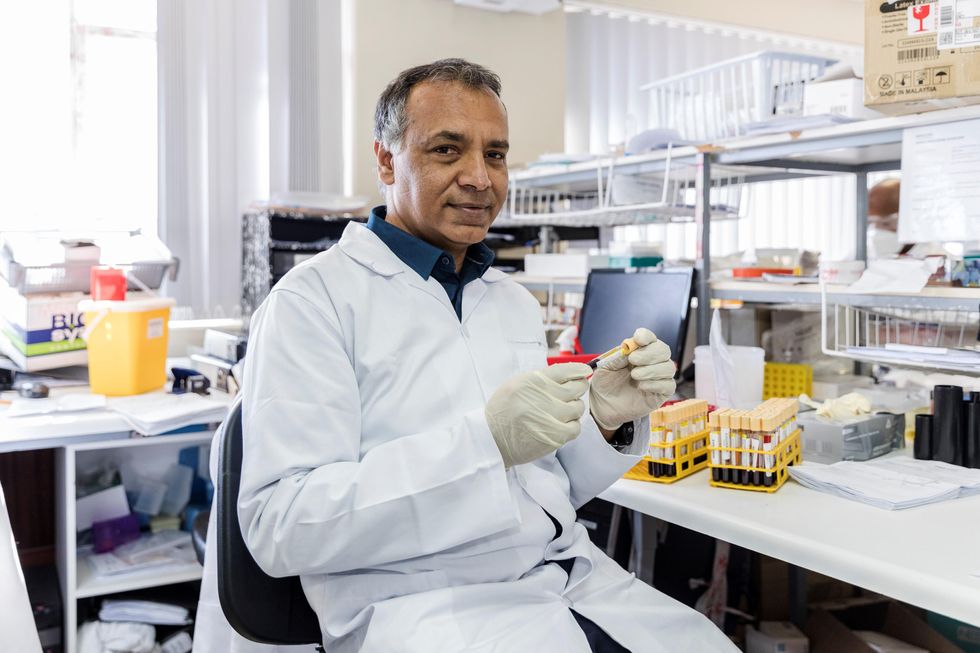
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Waste smothering our oceans is worth billions – here’s what we can do with all that sh$t
In 2015, human poop was valued at $9.5 billion per year, which today would be $11.5 billion. The Ocean Sewage Alliance is uniting experts from key sectors to change how we handle our sewage and, in the process, create all sorts of economic benefits.
There’s hardly a person out there who hasn’t heard of the Great Pacific Garbage Patch. That type of pollution is impossible to miss. It stares you in the face from pictures and videos of sea turtles with drinking straws up their noses and acres of plastic swirling in the sea.
It demands you to solve the problem—and it works. The campaign to raise awareness about plastic pollution in the oceans has resulted in new policies, including bans on microplastics in personal care products, technology to clean up the plastic, and even new plastic-like materials that are better for the environment.
But there’s a different type of pollution smothering the ocean as you read this. Unfortunately, this one is almost invisible, but no less damaging. In fact, it’s even more serious than plastic and most people have no idea it even exists. It is literally under our noses, destroying our oceans, lakes, and rivers – and yet we are missing it completely while contributing to it daily. In fact, we exacerbate it multiple times a day—every time we use the bathroom.
It is the way we do our sewage.
Most of us don’t think much about what happens after we flush the toilet. Most of us probably assume that the substances we flush go “somewhere” and are dealt with safely. But we typically don’t think about it beyond that.
Most of us also probably don’t think about what’s in the ocean or lakes we swim in. Since others are swimming, jumping in is just fine. But our waterways are far from clean. In fact, at times they are incredibly filthy. In the US, we are dumping 1.2 trillion of gallons of untreated sewage into the environment every year. Just New York City alone discharges 27 billion gallons into the Hudson River basin annually.
How does this happen? Part of it is the unfortunate side effect of our sewage system design that dates back to over a century ago when cities were smaller and fewer people were living so close together.
Back then, engineers designed the so-called “combine sewer overflow systems,” or CSOs, in which the storm water pipes are connected to the sanitary sewer pipes. In normal conditions, the sewage effluent from homes flows to the treatment plants where it gets cleaned and released into the waterways. But when it rains, the pipe system becomes so overwhelmed with water that the treatment plant can’t process it fast enough. So the treatment plant has to release the excess water through its discharge pipes—directly, without treatment, into streams, rivers and the ocean.
The 1.2 trillion gallons of CSO releases isn’t even the full picture. There are also discharges from poorly maintained septic systems, cesspools and busted pipes of the aging wastewater infrastructure. The state of Hawaii alone has 88,000 cesspools that need replacing and are currently leaking 53 million gallons of raw sewage daily into their coastal waters. You may think twice about swimming on your Hawaii vacations.
Overall, the US is facing a $271 billion backlog in wastewater infrastructure projects to update these aging systems. Across the Western world, countries are facing similar challenges with their aging sewage systems, especially the UK and European Union.
That’s not to say that other parts of the planet are in better shape. Out of the 7+ billion people populating our earth, 4.2 billion don’t have access to safe sanitation. Included in this insane number are roughly 2 billion people who have no toilet at all. Whether washed by rains or dumped directly into the waterways, a lot of this sludge pollutes the environment, the drinking water, and ultimately the ocean.

Pipes pour water onto a rocky shore in Jakarta, Indonesia.
Tom Fisk
What complicates this from an ocean health perspective is that it’s not just poop and pee that gets dumped into nearby waterways. It is all the things we put in and on our bodies and flush down our drains. That vicious mix of chemicals includes caffeine, antibiotics, antidepressants, painkillers, hormones, microplastics, cocaine, cooking oils, paint thinners, and PFAS—the forever chemicals present in everything from breathable clothing to fire retardant fabrics of our living room couches. Recent reports have found all of the above substances in fish—and then some.
Why do we allow so much untreated sewage spill into the sea? Frankly speaking, for decades scientists and engineers thought that the ocean could handle it. The mantra back then was “dilution is the solution to pollution,” which might’ve worked when there were much fewer people living on earth—but not now. Today science is telling us that this old approach doesn’t hold. That marine habitats are much more sensitive than we had expected and can’t handle the amount of wastewater we are discharging into them.
The excess nitrogen and phosphorus that the sewage (and agricultural runoff) dumps into the water causes harmful algal blooms, more commonly known as red or brown tides. The water column is overtaken by tiny algae that sucks up all the oxygen from the water, creating dead zones like the big fish kills in the Gulf of Mexico. These algae also cause public health issues by releasing gases toxic to people and animals, including dementia, neurological damage, and respiratory illness. Marshes and mangroves end up with weakened root systems and start dying off. In a wastewater modeling study I published last year, we found that 31 percent of salt marshes globally were heavily polluted with human sewage. Coral reefs get riddled with disease and overgrown by seaweed.
We could convert sewage into high-value goods. It can be used to generate electricity, fertilizer, and drinking water. The technologies not only exist but are getting better and more efficient all the time.
Moreover, by way of our sewage, we managed to transmit a human pathogen—Serratia marcescens, which causes urinary, respiratory and other infections in people—to corals! Recent reports from the Florida Keys are showing white pox disease popping up in elk horn corals caused by S.marcescens, which somehow managed to jump species. Many recent studies have documented just how common this type of pollution is across the globe.
Yet, there is some good news in that abysmal sewage flow. Just like with plastic pollution, realizing that there’s a problem is the first step, so awareness is key. That’s exactly why I co-founded Ocean Sewage Alliance last year—a nonprofit that aims to “re-potty train the world” by breaking taboos in talking about the poop and pee problem, as well as uniting experts from various key sectors to work together to end sewage pollution in coastal areas.
To end this pollution, we have to change the ways we handle our sewage. Even more exciting is that by solving the sewage problem we can create all sorts of economic benefits. In 2015, human poop was valued at $9.5 billion a year globally, which today would be $11.5 billion per year.
What would one do with that sh$t?
We could convert it into high-value goods. Sewage can be used to generate electricity, fertilizer, and drinking water. The technologies not only exist but are getting better and more efficient all the time. Some exciting examples include biodigesters and urine diversion (or peecycling) systems that can produce fertilizer and biogas, essentially natural gas. The United Nations estimates that the biogas produced from poop could provide electricity for 138 million homes. And the recovered and cleaned water can be used for irrigation, laundry and flushing toilets. It can even be refined to the point that it is safe for drinking water – just ask the folks in Orange County, CA who have been doing so for the last few decades.
How do we deal with all the human-made pollutants in our sewage? There is technology for that too. Called pyrolysis, it heats up sludge to high temperatures in the absence of oxygen, which causes most of the substances to degrade and fall apart.
There are solutions to the problems—as long as we acknowledge that the problems exist. The fact that you are reading this means that you are part of the solution already. The next time you flush your toilet, think about where this output may flow. Does your septic system work properly? Does your local treatment plant discharge raw sewage on rainy days? Can that plant implement newer technologies that can upcycle waste? These questions are part of re-potty training the world, one household at a time. And together, these households are the force that can turn back the toxic sewage tide. And keep our oceans blue.
The U.S. must fund more biotech innovation – or other countries will catch up faster than you think
In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”

