Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
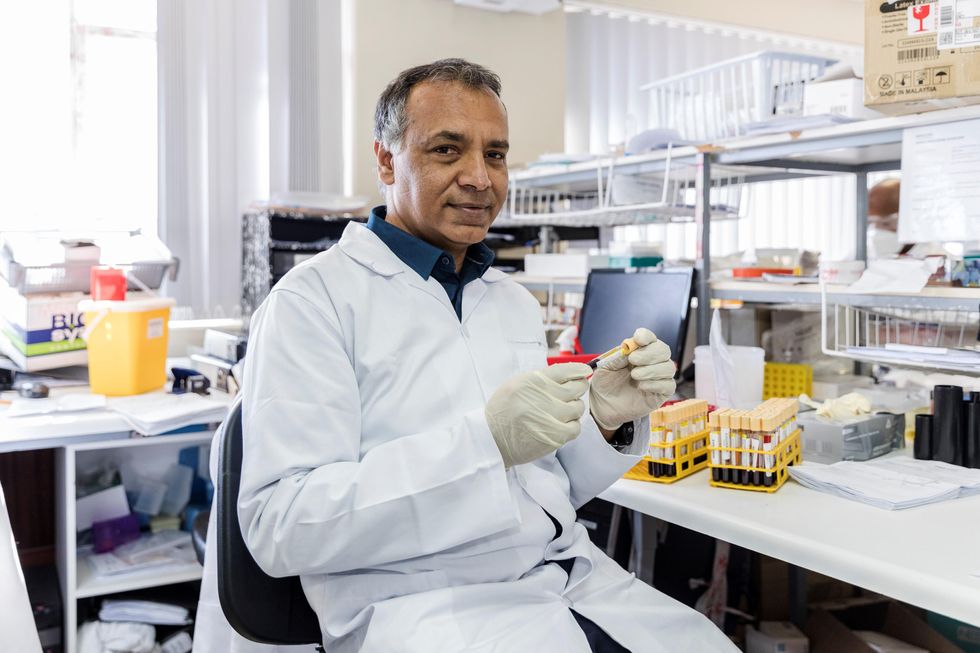
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Podcast: New Solutions to Combat Gluten Sensitivities and Food Allergies
Biotech company Ukko is designing proteins that will be safe for everyone to eat, starting with peanut and gluten.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
This month, we talk Anat Binur, the CEO of Israeli/U.S.-based biotech company Ukko. Ukko is taking a revolutionary approach to the distressing problem of food allergies and gluten sensitivities: their scientists are designing and engineering proteins that keep the good biophysical properties of the original proteins, while removing the immune-triggering parts that can cause life-threatening allergies. The end goal is proteins that are safe for everyone. Ukko is focusing first on developing a new safe gluten protein for use in baking and a new peanut protein for use as a therapeutic. Their unique platform could theoretically be used for any protein-based allergy, including cats and bees. Hear more in this episode.
Watch the 60-second trailer
Listen to the whole episode
<div id="buzzsprout-player-9950980"></div><script src="https://www.buzzsprout.com/1714953/9950980-solving-food-allergies-with-biotech-company-ukko.js?container_id=buzzsprout-player-9950980&player=small" type="text/javascript" charset="utf-8"></script>
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Can a Non-Invasive Magnetic Helmet Treat Brain Cancer?
Glioblastoma is an aggressive and deadly brain cancer, causing more than 10,000 deaths in the US per year. In the last 30 years there has only been limited improvement in the survival rate despite advances in radiation therapy and chemotherapy. Today the typical survival rate is just 14 months and that extra time is spent suffering from the adverse and often brutal effects of radiation and chemotherapy.
Scientists are trying to design more effective treatments for glioblastoma with fewer side effects, and a team at the Department of Neurosurgery at Houston Methodist Hospital has created a magnetic helmet-based treatment called oncomagnetic therapy: a promising non-invasive treatment for shrinking cancerous tumors. In the first patient tried, the device was able to reduce the tumor of a glioblastoma patient by 31%. The researchers caution, however, that much more research is needed to determine its safety and effectiveness.
How It Works
“The whole idea originally came from a conversation I had with General Norman Schwarzkopf, a supposedly brilliant military strategist,” says David Baskin, professor of neurosurgery and leader of the effort at Houston Methodist. “I asked him what is the secret to your success and he said, ‘Energy. Take out the power grid and the enemy can't communicate.’ So I thought about what supplies [energy to] cancer, especially brain cancer.”
Baskin came up with the idea of targeting the mitochondria, which process and produce energy for cancer cells.
"This is the most exciting thing in glioblastoma treatment I've seen since I've been a neurosurgeon, but it is very preliminary,” Baskin says.
The magnetic helmet creates a powerful oscillating magnetic field. At a set range of frequencies and timings, it disrupts the flow of electrons in the mitochondria of cancer cells. This leads to a release of certain chemicals called Reactive Oxygen Species, or ROS. In normal cells, this excess ROS is much lower, and it's neutralized by other chemicals called antioxidants.
However, cancer cells already have more ROS: they grow rapidly and uncontrollably, so their mitochondria need to produce more energy which in turn generates more ROS. By using the powerful magnetic field, levels of ROS get so high that the malignant cells are torn apart.
The biggest challenge was working out the specific range of frequencies and timing parameters they needed to use to kill cancer cells. It took skill, intuition, luck and lots of experiments. The helmet could theoretically be used to treat all types of glioblastoma.
Developing the magnetic helmet was a collaborative process. Santosh Helekar is a neuroscientist at Houston Methodist Research Institute and the director of oncomagnetics (magnetic cancer therapies) at the Peak Center in Houston Methodist Hospital. His previous invention with colleagues gave the team a starting point to build on. “About 7 years back I developed a portable brain magnetic stimulation device to conduct brain research,” Helekar says. “We [then] conducted a pilot clinical trial in stroke patients. The results were promising.”
Helekar presented his findings to neurosurgeons including Baskin. They decided to collaborate. With a team of scientists behind them, they modified the device to kill cancer cells.

The magnetic helmet studied for treatment of glioblastoma
Dr. David Baskin
Initial Results
After success in the lab, the team got FDA approval to conduct a compassionate trial in a 53-year-old man with end-stage glioblastoma. He had tried every other treatment available. But within 30 days of using the magnetic helmet his tumor shrank by 31%.
Sadly, 36 days into the treatment, the patient had an unrelated head injury due to a fall. The treatment was paused and he later died of the injury. Autopsy results of his brain highlighted the dramatic reduction in tumor cells.
Baskin says, “This is the most exciting thing in glioblastoma treatment I've seen since I've been a neurosurgeon, but it is very preliminary.”
The helmet is part of a growing number of non-invasive cancer treatments. One device that is currently being used by glioblastoma patients is Optune. It uses electric fields called tumor treating fields to slow down cell division and has been through a successful phase 3 clinical trial.
The magnetic helmet has the promise to be another useful non-invasive treatment according to Professor Gabriel Zada, a neurosurgeon and director of the USC Brain Tumor Center. “We're learning that various electromagnetic fields and tumor treating fields appear to play a role in glioblastoma. So there is some precedent for this though the tumor treating fields work a little differently. I think there is major potential for it to be effective but of course it will require some trials.”
Professor Jonathan Sherman, a neurosurgeon and director of neuro-oncology at West Virginia University, reiterates the need for further testing. “It sounds interesting but it’s too early to tell what kind of long-term efficacy you get. We do not have enough data. Also if you’re disrupting [the magnetic field] you could negatively impact a patient. You could be affecting the normal conduction of electromagnetic activity in the brain.”
The team is currently extending their research. They are now testing the treatment in two other patients with end-stage glioblastoma. The immediate challenge is getting FDA approval for those at an earlier stage of the disease who are more likely to benefit.
The Future
Baskin and the team are designing a clinical trial in the U.S., .U.K. and Germany. After positive results in cell cultures, they’re in negotiations to collaborate with other researchers in using the technology for lung and breast cancer. With breast cancer, the soft tissue is easier to access so a magnetic device could be worn over the breast.
“My hope is to develop a treatment to treat and hopefully cure glioblastoma without radiation or chemotherapy,” Baskin says. “We're onto a strategy that could make a huge difference for patients with this disease and probably for patients with many other forms of cancer.”