Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

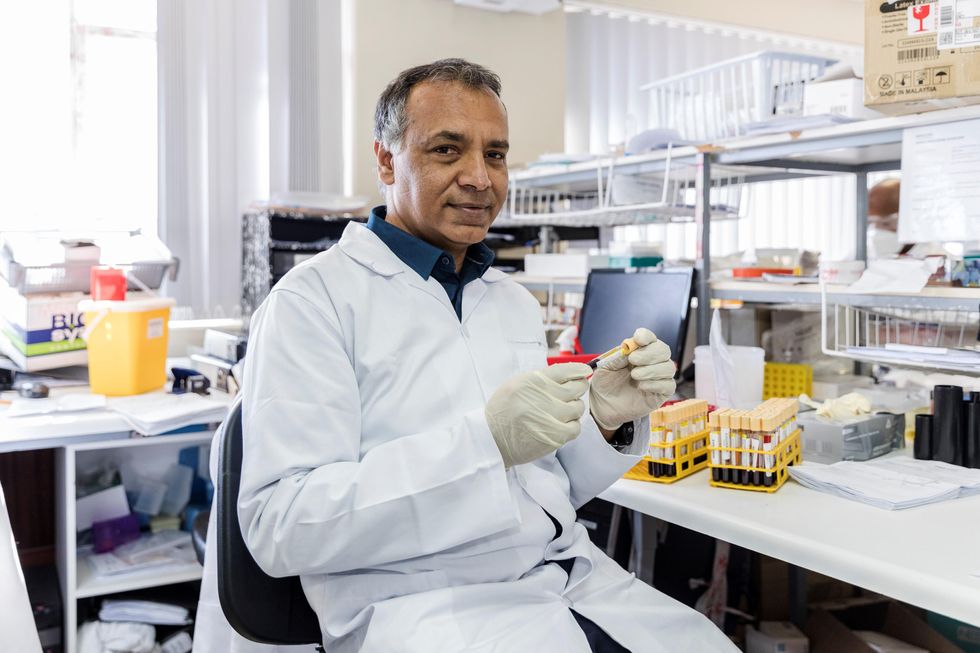
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Did researchers finally find a way to lick COVID?
A professor of medicine at the University of Michigan is researching whether lactoferrin, which is found in dairy products such as ice cream, can help to prevent COVID-19 infections.
Already vaccinated and want more protection from COVID-19? A protein found in ice cream could help, some research suggests, though there are a bunch of caveats.
The protein, called lactoferrin, is found in the milk of mammals and thus in dairy products, including ice cream. It has astounding antiviral properties that have been taken for granted and remain largely unexplored because it is a natural product, meaning that it cannot be patented and exploited by pharmaceutical companies.
Still, a few researchers in Europe and elsewhere have sought to better understand the compound.
Jonathan Sexton runs a drug screening program at the University of Michigan where cells are infected with a pathogen and then exposed to a library of the thousands of small molecule drug compounds – which can enter the body more easily than drugs with heavier molecules – approved by the FDA. In addition, the library includes compounds that passed phase 1 safety studies but later proved ineffective against the targeted disease. Each drug is dissolved in a solvent for exposure to the cells in the laborious testing process made feasible by robotic automation.
When COVID hit, researchers scrambled to identify any approved drug that might help fight the infection. Sexton decided to screen the drug library as well as some dietary supplements against SARS-CoV-2, the virus that causes the disease. Sexton says that the grunt work fell to Jesse Wotring, “a very talented PhD student,” who pulled lactoferrin off the shelf. But the regular solvent used in the testing process would destroy the protein, so he had to take another approach and do all the work by hand.
“We were agnostic,” says Sexton, who didn't have a strong interest in lactoferrin or any of the other compounds in the library, but the data was quite clear; lactoferrin “consistently produced the best efficacy...it was the absolute home run.” The findings were published in separate papers last year and in February.
It turns out that lactoferrin has several different mechanisms of action against SARS-CoV-2, inhibiting the virus from entering cells, moving around within them and replicating. Lactoferrin also modulates the overall immune response, which makes it difficult for the virus to simultaneously mutate resistance to the protein at every step of replication. “It has broad efficacy against every [SARS-CoV-2] variant that we've tested,” he says.
From bench to bedside
Sexton's initial interest was to develop a drug for the acute phase of COVID infection, to treat a hospitalized patient or prevent that hospitalization. But with the quick approval of vaccines and drugs to treat the disease, he increasingly focused on ways to better prevent infection and inhibit spread of the virus.
“If you can get lactoferrin to persist in your upper GI tract, then it may very well prevent the primary infection, and that's what we're really interested in.” He reasoned that a chewing gum formula might release enough lactoferrin into the mucosal tissue of the mouth and upper airways to inhibit replication and give the immune system a chance to knock out the virus before it can establish a foothold. It could also reduce the amount of virus spread through talking.
To get enough lactoferrin to have a possible beneficial effect, one would have to drink gallons of milk a day, “and that would have other undesirable consequences, like getting extremely obese,” says Sexton. Obesity is one of the leading risk factors for severe COVID disease.
Testing that theory has been difficult. The easiest way would be a “challenge trial,” where volunteers take the drug, or in this case gum, are exposed to the pathogen, and protection is measured. Some COVID challenge studies have been conducted in Europe but the FDA remains hesitant to allow such a study in the U.S. A traditional prevention study would be like a vaccine trial, involving thousands, perhaps tens of thousands of volunteers over a period of months or years, and it would be very expensive. No one has stepped forward to foot the bill.
So the next step for Sexton is a clinical trial of newly diagnosed COVID patients who will be given standard of care treatment, and layered on top of that they will receive either lactoferrin, probably in pill form, or a placebo. He has identified initial funding. “We would study their viral load over time as well as their symptoms.”
One issue the FDA is grappling with in considering the proposed trial is that it typically decides whether to approve drugs from a factory by applying a rigorous standard, called good manufacturing practices, while food products, which are the source of lactoferrin, are produced under somewhat different standards. The agency still has not finalized rules on how to deal with natural products used as drugs, such as fecal transplants, convalescent plasma, or medical marijuana.
Sexton is frustrated by the delay because lactoferrin derived from bovine milk whey has been used for many decades as a protein supplement by athletes, it is a large component of most infant formula, and the largest number of clinical studies of lactoferrin involve premature infants. There is no question of its safety, he says.
Do it yourself
So what can you do while waiting for regulatory wheels to spin and clinical trial data to be generated?
Could a dose of Ben & Jerry's provide some protection against SARS-CoV-2?
Sexton chuckles at the suggestion. He supposes it couldn't hurt. But to get enough lactoferrin to have a possible beneficial effect, one would have to drink gallons of milk a day, “and that would have other undesirable consequences, like getting extremely obese.” Obesity is one of the leading risk factors for severe COVID disease.
Pseudo-milk products made from soy, almonds, oats, or other plant products do not contain lactoferrin; it has to come from a teat. So that rules them out.
Whey-based protein shakes might be a useful way to add lactoferrin to the diet.
Probably the best option is to take conventional gelatin capsules of lactoferrin that are widely available wherever supplements are sold. Sexton calculates that about a gram a day, four 250 milligram capsules, should do it. He advises two in the morning and two a night. “You really want to take them on an empty stomach...your stomach treats [the lactoferrin protein] like it would a steak” and chops it for absorption in the intestine, which you do not want. About 70 percent of lactoferrin can get through an empty stomach, but eating food cranks up digestive gastric acids and the amount of intact lactoferrin that gets through to the gut plummets.
Sexton cautions, “We have not determined clinical efficacy yet,” and he is not offering advice as a physician, but in the spirit of harm reduction, he realizes that some people are going to try things that might help them. Lactoferrin “is remarkably safe. And so people have to make their own decisions about what they are willing to take and what they are not,” he says.
In today's episode, Leaps.org interviews Camila dos Santos, a molecular biologist at Cold Spring Harbor Lab, about her research on breasts and what makes them unique compared to any other part of the body.
My guest today for the Making Sense of Science podcast is Camila dos Santos, associate professor at Cold Spring Harbor Lab, who is a leading researcher of the inner lives of human mammary glands, more commonly known as breasts. These organs are unlike any other because throughout life they undergo numerous changes, first in puberty, then during pregnancies and lactation periods, and finally at the end of the cycle, when babies are weaned. A complex interplay of hormones governs these processes, in some cases increasing the risk of breast cancer and sometimes lowering it. Witnessing the molecular mechanics behind these processes in humans is not possible, so instead Dos Santos studies organoids—the clumps of breast cells donated by patients who undergo breast reduction surgeries or biopsies.
Show notes:
2:52 In response to hormones that arise during puberty, the breast cells grow and become more specialized, preparing the tissue for making milk.
7:53 How do breast cells know when to produce milk? It’s all governed by chemical messaging in the body. When the baby is born, the brain will release the hormone called oxytocin, which will make the breast cells contract and release the milk.
12:40 Breast resident immune cells are including T-cells and B-cells, but because they live inside the breast tissue their functions differ from the immune cells in other parts of the body,
17:00 With organoids—dimensional clumps of cells that are cultured in a dish—it is possible to visualize and study how these cells produce milk.
21:50 Women who are pregnant later in life are more likely to require medical intervention to breastfeed. Scientists are trying to understand the fundamental reasons why it happens.
26:10 Breast cancer has many risks factors. Generic mutations play a big role. All of us have the BRCA genes, but it is the alternation in the DNA sequence of the BRCA gene that can increase the predisposition to breast cancer. Aging and menopause are the risk factors for breast cancer, and so are pregnancies.
29:22 Women that are pregnant before the age of 20 to 25, have a decreased risk of breast cancer. And the hypothesis here is that during pregnancy breast cells more specialized, as specialized cells, they have a limited lifespan. It's more likely that they die before they turn into cancer.
33:08 Organoids are giving scientists an opportunity to practice personalized medicine. Scientists can test drugs on organoids taken from a patient to identify the most efficient treatment protocol.
Links:
Camila dos Santos’s Lab Page.
Editor's note: In addition to being a regular writer for Leaps.org, Lina Zeldovich is the guest host for today's episode of the Making Sense of Science podcast.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

