Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

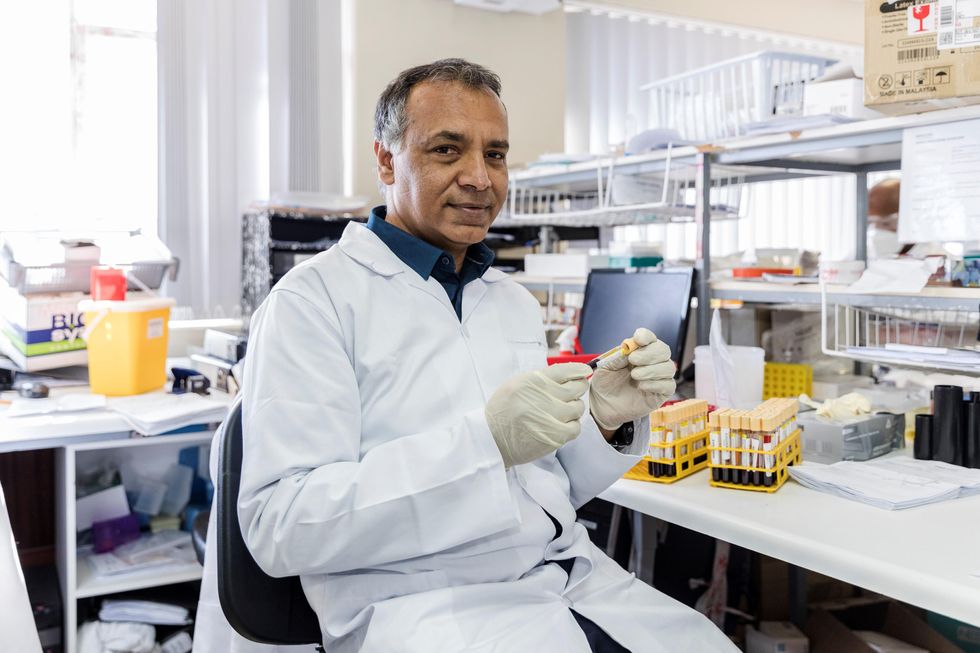
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Over 1 Million Seeds Are Buried Near the North Pole to Back Up the World’s Crops
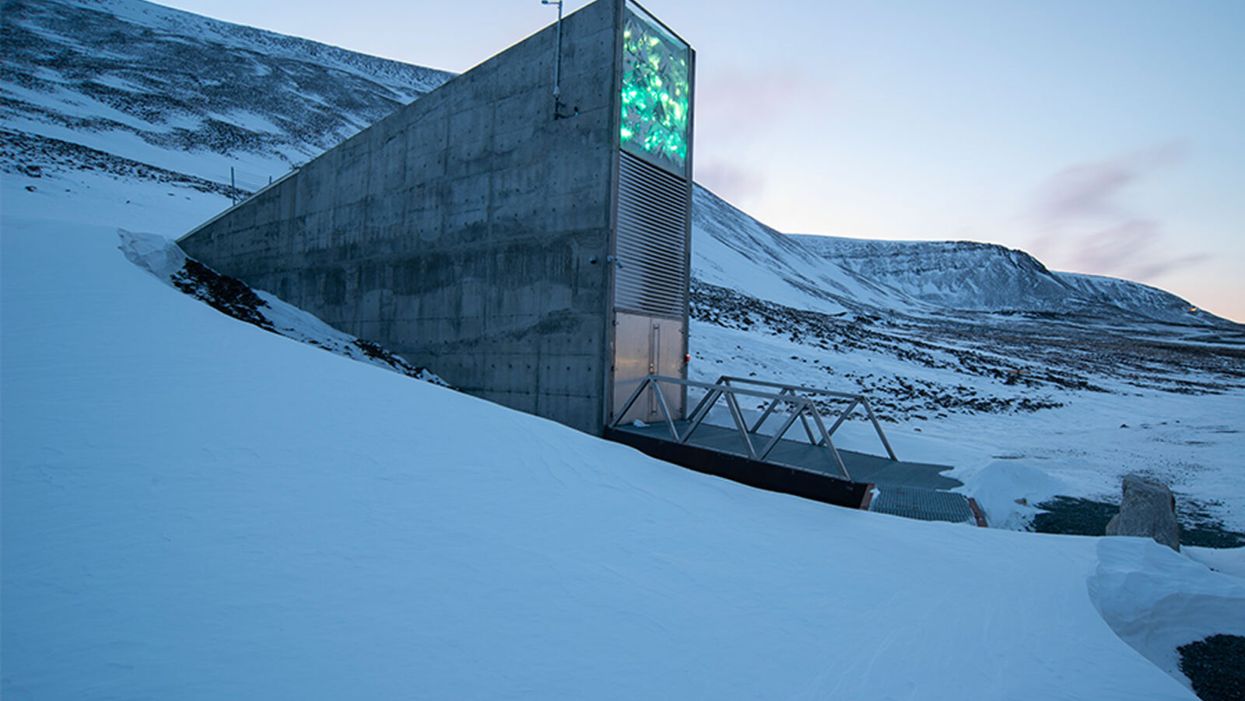
The Svalbard Global Seed Vault preserves more than one million of the world's seeds deep inside Platäfjellet Mountain.
The impressive structure protrudes from the side of a snowy mountain on the Svalbard Archipelago, a cluster of islands about halfway between Norway and the North Pole.
"Before, we trusted the permafrost. We do not trust the permafrost anymore."
Art installations on the building's rooftop and front façade glimmer like diamonds in the polar night, but it is what lies buried deep inside the frozen rock, 475 feet from the building's entrance, that is most precious. Here, in the Svalbard Global Seed Vault, are backup copies of more than a million of the world's agricultural seeds.

Inside the vault, seed boxes from many gene banks and many countries. "The seeds don't know national boundaries," says Kent Nnadozie, the UN's Secretary of the International Treaty on Plant Genetic Resources for Food and Agriculture.
(Photo credit: Svalbard Global Seed Vault/Riccardo Gangale)
The Svalbard vault -- which has been called the Doomsday Vault, or a Noah's Ark for seeds -- preserves the genetic materials of more than 6000 crop species and their wild relatives, including many of the varieties within those species. Svalbard's collection represents all the traits that will enable the plants that feed the world to adapt – with the help of farmers and plant breeders – to rapidly changing climactic conditions, including rising temperatures, more intense drought, and increasing soil salinity. "We save these seeds because we want to ensure food security for future generations," says Grethe Helene Evjen, Senior Advisor at the Norwegian Ministry of Agriculture and Food .
A recent study in the journal Nature predicted that global warming could cause catastrophic losses of biodiversity in regions across the globe throughout this century. Yet global warming also threatens the permafrost that surrounds the seed vault, the very thing that was once considered a failsafe means of keeping these seeds frozen and safeguarding the diversity of our crops. In fact, record temperatures in Svalbard a few years ago – and a significant breach of water into the access tunnel to the vault -- prompted the Norwegian government to invest $20 million euros on improvements at the facility to further secure the genetic resources locked inside. The hope: that technology can work in concert with nature's freezer to keep the world's seeds viable.
"Before, we trusted the permafrost," says Hege Njaa Aschim, a spokesperson for Statsbygg, the government agency that recently completed the upgrades at the seed vault. "We do not trust the permafrost anymore."
The Apex of the Global Conservation System
More than 1700 genebanks around the globe preserve the diverse seed varieties from their regions. They range from small community seed banks in developing countries, where small farmers save and trade their seeds with growers in nearby villages, to specialized university collections, to national and international genetic resource repositories. But many of these facilities are vulnerable to war, natural disasters, or even lack of funding.
"If anything should happen to the resources in a regular genebank, Svalbard is the backup – it's essentially the apex of the global conservation system," says Kent Nnadozie, Secretary of the International Treaty on Plant Genetic Resources for Food and Agriculture at the United Nations, who likens the Global Vault to the Central Reserve Bank. "You have regular banks that do active trading, but the Central Bank is the final reserve where the banks store their gold deposits."
Similarly, farmers deposit their seeds in regional genebanks, and also look to these banks for new varieties to help their crops adapt to, say, increasing temperatures, or resist intrusive pests. Regional banks, in turn, store duplicates from their collections at Svalbard. These seeds remain the sovereign property of the country or institution depositing them; only they can "make a withdrawal."
The Global Vault has already proven invaluable: The International Centre for Agricultural Research in the Dry Areas (ICARDA), formerly located outside of Aleppo, Syria, held more than 140,000 seed samples, including plants that were extinct in their natural habitats, before the Syrian Crisis in 2012. Fortunately, they had managed to back up most of their seed samples at Svalbard before they were forced to relocate to Lebanon and Morocco. In 2017, ICARDA became the first – and only – organization to withdraw their stored seeds. They have now regenerated almost all of the samples at their new locations and recently redeposited new seeds for safekeeping at Svalbard.
Rapid Global Warming Threatens Permafrost
The Global Vault, a joint venture between the Norwegian government, the Crop Trust and the Nordic Genetic Resource Centre (NordGen) that started operating in 2008, was sited in Svalbard in part because of its remote yet accessible location: Svalbard is the northernmost inhabited spot on Earth with an airport. But experts also thought it a failsafe choice for long-term seed storage because its permafrost would offer natural freezing – even if cooling systems were to fail. No one imagined that the permafrost could fail.
"We've had record temperatures in the region recently, and there are a lot of signs that global warming is happening faster at the extreme latitudes," says Geoff Hawtin, a world-renowned authority in plant conservation, who is the founding director of -- and now advisor to -- the Crop Trust. "Svalbard is still arguably one of the safest places for the seeds from a temperature point of view, but it's actually not going to be as cold as we thought 20 years ago."
A recent report by the Norwegian Centre for Climate Services predicted that Svalbard could become 50 degrees Fahrenheit warmer by the year 2100. And data from the Norwegian government's environmental monitoring system in Svalbard shows that the permafrost is already thawing: The "active layer," that is, the layer of surface soil that seasonally thaws, has become 25-30 cm thicker since 1998.
Among the 35 depositors were several bringing their seeds to Svalbard for the first time, including the Cherokee Nation, which deposited nine heirloom seed varieties that predate European colonization.
Though the permafrost surrounding the seed vault chambers, which are situated well below the active layer, is still intact, the permafrost around the access tunnel never re-established as expected after construction of the Global Vault twelve years ago. As a result, when Svalbard saw record high temperatures and unprecedented rainfall in 2016, about 164 feet of rainwater and snowmelt leaked into the tunnel, turning it into a skating rink and spurring authorities to take what they called a "better safe than sorry approach." They invested in major upgrades to the facility. "The seeds in the vault were never threatened," says Aschim, "but technology has become more important at Svalbard."
Technology Gives Nature a Boost
For now, the permafrost deep inside the mountain still keeps the temperature in the vault down to about -25°F. The cooling systems then give nature a mechanical boost to keep the seed vault chilled even further, to about -64°F, the optimal temperature for conserving seeds. In addition to upgrading to a more effective and sustainable cooling system that runs on CO2, the Norwegian government added backup generators, removed heat-generating electrical equipment from inside the facility to an outside building, installed a thick, watertight door to the vault, and replaced the corrugated steel access tunnel with a cement tunnel that uses the same waterproofing technology as the North Sea oil platforms.
To re-establish the permafrost around the tunnel, they layered cooling pipes with frozen soil around the concrete tunnel, covered the frozen soil with a cooling mat, and topped the cooling mat with the original permafrost soil. They also added drainage ditches on the mountainside to divert meltwater away from the tunnel as the climate gets warmer and wetter.
New Deposits to the Global Vault
The day before COVID-19 arrived in Norway, on February 25th, Prime Minister Erna Solberg hosted the biggest seed-depositing event in the vault's history in honor of the new and improved vault. As snow fell on Svalbard, depositors from almost every continent traveled the windy road from Longyearbyen up Platåfjellet Mountain and braved frigid -8°F weather to celebrate the massive technical upgrades to the facility – and to hand over their seeds.
Among the 35 depositors were several bringing their seeds to Svalbard for the first time, including the Cherokee Nation, which deposited nine heirloom seed varieties that predate European colonization, and Israel's University of Haifa, whose deposit included multiple genotypes of wild emmer wheat, an ancient relative of the modern domesticated crop. The storage boxes carried ceremoniously over the threshold that day contained more than 65,000 new seed samples, bringing the total to more than a million, and almost filling the first of three seed chambers in the vault. (The Global Vault can store up to 4.5 million seed samples.)
"Svalbard's samples contain all the possibilities, all the options for the future of our agricultural crops – it's how crops are going to adapt," says Cary Fowler, former executive director of the Crop Trust, who was instrumental in establishing the Global Vault. "If our crops don't adapt to climate change, then neither will we." Dr. Fowler says he is confident that with the recent improvements in the vault, the seeds are going to remain viable for a very long time.
"It's sometimes tempting to get distracted by the romanticism of a seed vault inside a mountain near the North Pole – it's a little bit James Bondish," muses Dr. Fowler. "But the reality is we've essentially put an end to the extinction of more than a million samples of biodiversity forever."
From Crap to Cure: The Story of Fecal Transplants
Meg Newman, who suffered from C. difficile, underwent a fecal transplant that helped restore her to health.
C. difficile had Meg Newman's number; it had struck her 18 different times beginning in 1985. The bacterial infection takes over the gut bringing explosive diarrhea, dehydration, weight loss, and at its worst depletes blood platelets. It causes nearly 30,000 deaths each year in the U.S. alone.
"I was one sick puppy as that point and literally three days after the transplant I was doing pretty well, day four even better."
Meg knew these statistics not just from personal experience but also because she was a doctor at San Francisco General Hospital. Antibiotics had sometimes helped to treat the infection, but it never quite seemed to go away. Now, "It felt like part of my colon was sort of sliding off as I had the bowel movement." On her worst day she counted 33 bowel movements. It was 2005 and she knew she was at the end of her rope.
Medical training had taught Meg to look at the data. So when antibiotics failed, she searched the literature for other options. One was a seemingly off-the-wall treatment called fecal transplants, which essentially gives poop from a healthy person to one who is sick.
Its roots stretch back to "yellow soup" used to treat dysentery in China nearly two thousand years ago, in which ancient Chinese treaters would combine stool with liquid, mash it up, and administer it. The approach also is commonly used in veterinary medicine today. However, there were only about three papers on its use in humans in the medical literature at that time, she recalls. Still, the logic of the intervention appealed to her.
The gut microbiome as a concept and even a word were not widely known fifteen years ago. But the idea that the microbial community in her gut was in disarray, and a transplant of organisms from a healthy gut might help restore a more normal ecology made sense. And besides, the failure of standard medicine left her few options.
Meg spoke with a colleague, gastroenterologist Neil Stollman, about a possible fecal microbial transplant (FMT). Only a handful of doctors in the U.S. had ever done the procedure; Stollman had tried it just once before. After conversation with Newman, he agreed to do it.
They decided on Meg's partner Sherry as the donor. "I try very hard to use intimate sexual partners as the donor," explains Stollman. The reason is to reduce disease risk: "The logic there is pretty straightforward. If you have unprotected sex with this individual, in a monogamous way for a period of time, you have assumed pretty much any infectious risk," like hepatitis, HIV, and syphilis, he says. Other donors would be screened using the same criteria used to screen blood donations, plus screening for parasites that can live in stool but not blood.
The procedure
Martini aficionados fall into two camps, fans of shaken or stirred. In the early days the options for producing of fecal transplants were a blender or hand shaken. Stollman took the hands-on approach, mixing Sherry's fecal donation with saline to create "a milkshake in essence." He filtered it several times through gauze to get out the lumps.
Then he inserted a colonoscope, a long flexible tube, through the anus into Meg's colon. Generally a camera goes through the tube to look for polyps and cancers, while other tools can snip off polyps and retrieve tissue samples. Today he used it to insert the fecal "milkshake" as high up the colon as he could go. Imodium and bed rest were the final pieces. It works about 90 percent of the time today.
Meg went home with fingers crossed. "And within about two weeks things just slowed down; the diarrhea just stopped. I felt better so my appetite was better." The tide had turned, though it would take months to slowly repair the toll taken on her body from disease and antibiotics.
Then in 2011 another serious medical challenge required heavy use of antibiotics and Meg's C. difficile came roaring back; she needed a second FMT. Sherry had a bad sinus infection and had been on antibiotics, so that ruled her out as a donor. Red, Meg's godson, volunteered. He was twenty-one and had little or no exposure to antibiotics, which can harm friendly bacteria living in the gut.
"I was one sick puppy as that point," Meg recalls, "and literally three days after the transplant [from Red] I was doing pretty well, day four even better. It was unbelievable." It illustrated that donors are not the same, and that while an intimate partner may be the safest option, it also may not be the most efficacious donation in terms of providing missing parts of the microbial ecosystem.
Going mainstream
By then, FMTs were starting to come out of the shadows as more than just a medical oddity. One gigantic milestone in changing perceptions was a Dutch study on using the procedure to treat C. difficile that was published in January 2013 in the New England Journal of Medicine. "That was the first trial where people said, look this isn't voodoo. This wasn't made up; it really worked," says Colleen Kelly, another pioneer in using FMTs to treat C. difficile and a researcher at Brown University. A single dose was successful more than 80 percent of the time in resolving disease in patients who had failed multiple regimens of antibiotics.
Charlatans pounced on the growing interest in the microbiome, promoting FMT as a cure for all sorts of ailments for which there was no scientific evidence. The FDA stepped in, announcing it would regulate the procedure as a drug, and essentially banned use of FMTs until it wrote regulations. But the outcry from physicians and patients was so great it was forced to retreat and has allowed continued use in treating C. difficile albeit on an interim regulatory basis that has continued since 2013.
Another major change was the emergence of stool banks, modeled on blood banks. The most widely know is OpenBiome, established in 2012 as a nonprofit by young researchers at Harvard and MIT. It aimed to standardize donation of stool and screening for disease, and package them in frozen form for colonoscopic delivery, or pill form. It greatly simplified the process and more doctors became willing to use FMTs to treat C. difficile. Today, some gastroenterologists specialize in administering the transplants as a feature of their practice.
To be sure, there have been some setbacks, including a transplant between family members where the recipient became obese, likely in part because of bacteria in the material she received. The same thing has occurred in studies in mice. And last year, an elderly man died from a toxic strain of E. coli that was in material provided by a stool bank. That caused the FDA to add that pathogen to the list of those one must screen for in products designed for use as fecal transplants.
Cost remains an issue. OpenBiome charges $1500-$2000 per transplant dose, depending on whether a frozen or pill form of the product is used. And that is likely to go up as the FDA increases the number of diseases that must be screened for, such as the virus that causes COVID-19, which is present in feces and likely can be transmitted through feces. Most insurance companies do not cover FMTs because no product has been formally approved for use by the FDA.
One of the greatest treatment challenges is making the correct diagnosis, says physician Robin Patel, who initially treated patients at the Mayo Clinic in Rochester, Minnesota but now spends most of her time there developing new diagnostics. Many things can cause diarrhea and the simple presence of the organism does not mean that C. difficile is causing it. In addition, many people are colonized with the bug but never develop symptoms of the disease.
Patel used the expensive tool of whole genome sequencing to look in great detail at C. difficile in patients who were treated with antibiotics for the infection and had recurrent diarrhea. "Some of them, as you might predict, were getting their symptoms with the same exact strain [of C. difficile] but others were not, it was a different strain," suggesting that they had been reinfected.
If it is a different strain, you might want to try antibiotics, she says, but if the same strain is present, then you might want to try a different approach such as FMT. Whole genome sequencing is still too slow and expensive to use in regularly treating patients today, but Patel hopes to develop a rapid, cost-effective test to help doctors make those types of decisions.
Biotech companies are trying to develop alternatives to poop as a source for transplant to treat C. difficile. They are picking and choosing different bacteria that they can grow and then combine into a product, to varying degrees of success, but none have yet crossed the finish line of FDA approval.
"I think [the future of FMTs] is going to be targeted, even custom-made."
The FDA would like such a product because it is used to dealing with small molecule drugs that are standardized and produced in batches. Companies are pursing it because, as Kelly says, they are like sharks "smelling money in the water." Approval of such a product might cause the FDA to shut down existing stool banks that now exist in a regulatory limbo, leaving the company with a monopoly of exclusive rights to the treatment.
Back when Meg received her first fecal transplant, the procedure was so obscure that the guidelines for treating C. difficile put out by the American College of Gastroenterology didn't even mention FMT. The procedure crept into the 2013 revision of those guidelines as a treatment of last resort. Guidance under review for release later this year or early next year will ease use further but stop short of making it a first option.
Stollman imagines a future holy grail in treating C. difficile: "You give me a stool specimen and I run it through a scanner that tells me you have too much of this and too little of that. I have a sense of what normal [microbial composition of the gut] should be and add some of this and subtract some of that. Maybe I even give you some antibiotics to get rid of some of the bad guys, give you some probiotics. I think it is going to be targeted, even custom-made."
His complete vision for treating C. difficile won't arrive tomorrow, but given how rapidly FMTs have become part of medicine, it is likely to arrive in pieces and more quickly than one might think.
About five years ago Meg discovered she had an antibody deficiency that contributed to her health problems, including vulnerability to C. difficile. She began supplementation with immunoglobulin and "that has made a huge difference in my health. It is just unbelievable how much better I am." She is grateful that fecal transplants gave her the time to figure that out. She believes "there's every reason to consider it [FMT] as a first-line treatment and do the studies, ASAP."