Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
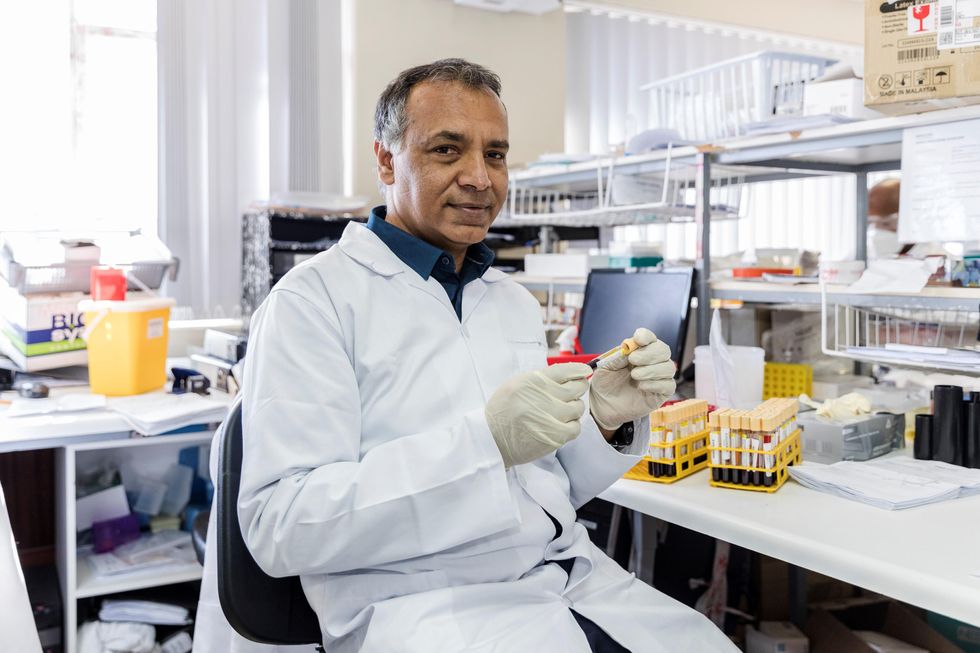
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
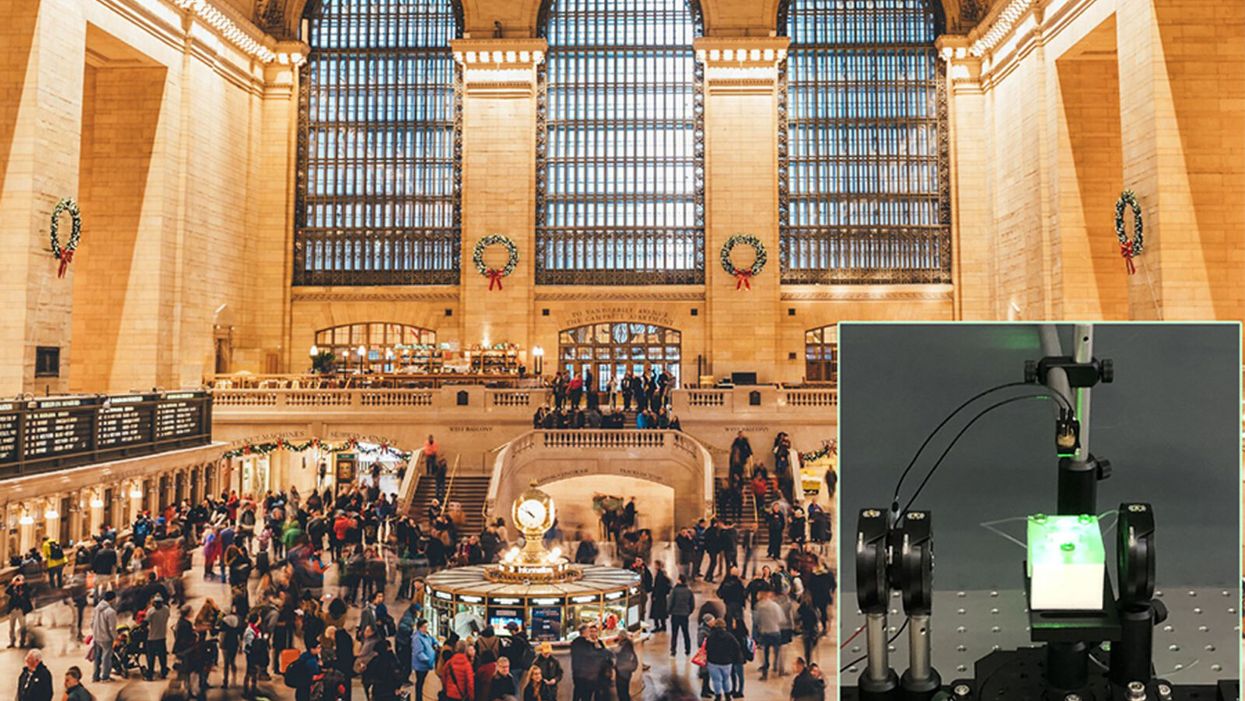
A biosensor in development (inset) could potentially be used to detect novel viruses in transit hubs like Grand Central Station in New York City.
The unprecedented scale and impact of the COVID-19 pandemic has caused scientists and engineers around the world to stop whatever they were working on and shift their research toward understanding a novel virus instead.
"We have confidence that we can use our system in the next pandemic."
For Guangyu Qiu, normally an environmental engineer at the Swiss Federal Laboratories for Materials Science and Technology, that means finding a clever way to take his work on detecting pollution in the air and apply it to living pathogens instead. He's developing a new type of biosensor to make disease diagnostics and detection faster and more accurate than what's currently available.
But even though this pandemic was the impetus for designing a new biosensor, Qiu actually has his eye on future disease outbreaks. He admits that it's unlikely his device will play a role in quelling this virus, but says researchers already need to be thinking about how to make better tools to fight the next one — because there will be a next one.
"In the last 20 years, there [have been] three different coronavirus [outbreaks] ... so we have to prepare for the coming one," Qiu says. "We have confidence that we can use our system in the next pandemic."
"A Really, Really Neat Idea"
His main concern is the diagnostic tool that's currently front and center for testing patients for SARS-Cov-2, the virus causing the novel coronavirus disease. The tool, called PCR (short for reverse transcription polymerase chain reaction), is the gold standard because it excels at detecting viruses in even very small samples of mucus. PCR can amplify genetic material in the limited sample and look for a genetic code matching the virus in question. But in many parts of the world, mucus samples have to be sent out to laboratories for that work, and results can take days to return. PCR is also notoriously prone to false positives and negatives.
"I read a lot of newspapers that report[ed] ... a lot of false negative or false positive results at the very beginning of the outbreak," Qiu says. "It's not good for protecting people to prevent further transmission of the disease."
So he set out to build a more sensitive device—one that's less likely to give you a false result. Qiu's biosensor relies on an idea similar to the dual-factor authentication required of anyone trying to access a secure webpage. Instead of verifying that a virus is really present by using one way of detecting genetic code, as with PCR, this biosensor asks for two forms of ID.
SARS-CoV-2 is what's called an RNA virus, which means it has a single strand of genetic code, unlike double-stranded DNA. Inside Qiu's biosensor are receptors with the complementary code for this particular virus' RNA; if the virus is present, its RNA will bind with the receptors, locking together like velcro. The biosensor also contains a prism and a laser that work together to verify that this RNA really belongs to SARS-CoV-2 by looking for a specific wavelength of light and temperature.
If the biosensor doesn't detect either, or only registers a match for one and not the other, then it can't produce a positive result. This multi-step authentication process helps make sure that the RNA binding with the receptors isn't a genetically similar coronavirus like SARS-CoV, known for its 2003 outbreak, or MERS-CoV, which caused an epidemic in 2012.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
Spina Bifida Claimed My Son's Mobility. Incredible Breakthroughs May Let Future Kids Run Free.
Sarah Watts's son Henry was born with spina bifida and can't stand or walk without assistance.
When our son Henry, now six, was diagnosed with spina bifida at his 20-week ultrasound, my husband and I were in shock. It took us more than a few minutes to understand what the doctor was telling us.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change.
Neither of us had any family history of birth defects. Our fifteen-month-old daughter, June, was in perfect health.
But more than that, spina bifida – a malformation of the neural tube that eventually becomes the baby's spine – is woefully complex. The defect, the doctor explained, was essentially a hole in Henry's lower spine from which his spinal nerves were protruding – and because they were exposed to my amniotic fluid, those nerves were already permanently damaged. After birth, doctors could push the nerves back into his body and sew up the hole, but he would likely experience some level of paralysis, bladder and bowel dysfunction, and a buildup of cerebrospinal fluid that would require a surgical implant called a shunt to correct. The damage was devastating – and irreversible.
We returned home with June and spent the next few days cycling between disbelief and total despair. But within a week, the maternal-fetal medicine specialist who diagnosed Henry called us up and gave us the first real optimism we had felt in days: There was a new, experimental surgery for spina bifida that was available in just a handful of hospitals around the country. Rather than waiting until birth to repair the baby's defect, some doctors were now trying out a prenatal repair, operating on the baby via c-section, closing the defect, and then keeping the mother on strict bedrest until it was time for the baby to be delivered, just before term.
This new surgery carried risks, he told us – but if it went well, there was a chance Henry wouldn't need a shunt. And because repairing the defect during my pregnancy meant the spinal nerves were exposed for a shorter amount of time, that meant we'd be preventing nerve damage – and less nerve damage meant that there was a chance he'd be able to walk.
Did we want in? the doctor asked.
Had I known more about spina bifida and the history of its treatment, this surgery would have seemed even more miraculous. Not too long ago, the standard of care for babies born with spina bifida was to simply let them die without medical treatment. In fact, it wasn't until the early 1950s that doctors even attempted to surgically repair the baby's defect at all, instead of opting to let the more severe cases die of meningitis from their open wound. (Babies who had closed spina bifida – a spinal defect covered by skin – sometimes survived past infancy, but rarely into adulthood).
But in the 1960s and 1970s, as more doctors started repairing defects and the shunting technology improved, patients with spina bifida began to survive past infancy. When catheterization was introduced, spina bifida patients who had urinary dysfunction, as is common, were able to preserve their renal function into adulthood, and they began living even longer. Within a few decades, spina bifida was no longer considered a death sentence; people were living fuller, happier lives.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change. The first major clinical trial for prenatal surgery and spina bifida, called Management of Myelomeningocele (MOMS) had just concluded, and its objective was to see whether repairing the baby's defect in utero would be beneficial. In the trial, doctors assigned eligible women to undergo prenatal surgery in the second trimester of their pregnancies and then followed up with their children throughout the first 30 months of the child's life.
The results were groundbreaking: Not only did the children in the surgery group perform better on motor skills and cognitive tests than did patients in the control group, only 40 percent of patients ended up needing shunts compared to 80 percent of patients who had postnatal surgery. The results were so overwhelmingly positive that the trial was discontinued early (and is now, happily, the medical standard of care). Our doctor relayed this information to us over the phone, breathless, and left my husband and me to make our decision.
After a few days of consideration, and despite the benefits, my husband and I actually ended up opting for the postnatal surgery instead. Prenatal surgery, although miraculous, would have required extensive travel for us, as well as giving birth in a city thousands of miles from home with no one to watch our toddler while my husband worked and I recovered. But other parents I met online throughout our pregnancy did end up choosing prenatal surgery for their children – and the majority of them now walk with little assistance and only a few require shunting.
Even more amazing to me is that now – seven years after Henry's diagnosis, and not quite a decade since the landmark MOMS trial – the standard of care could be about to change yet again.
Regardless of whether they have postnatal or prenatal surgery, most kids with spina bifida still experience some level of paralysis and rely on wheelchairs and walkers to move around. Now, researchers at UC Davis want to augment the fetal surgery with a stem cell treatment, using human placenta-derived mesenchymal stromal cells (PMSCs) and affixing them to a cellular scaffold on the baby's defect, which not only protects the spinal cord from further damage but actually encourages cellular regeneration as well.
The hope is that this treatment will restore gross motor function after the baby is born – and so far, in animal trials, that's exactly what's happening. Fetal sheep, who were induced with spinal cord injuries in utero, were born with complete motor function after receiving prenatal surgery and PMSCs. In 2017, a pair of bulldogs born with spina bifida received the stem cell treatment a few weeks after birth – and two months after surgery, both dogs could run and play freely, whereas before they had dragged their hind legs on the ground behind them. UC Davis researchers hope to bring this treatment into human clinical trials within the next year.
A century ago, a diagnosis of spina bifida meant almost certain death. Today, most children with spina bifida live into adulthood, albeit with significant disabilities. But thanks to research and innovation, it's entirely possible that within my lifetime – and certainly within Henry's – for the first time in human history, the disabilities associated with spina bifida could be a thing of the past.