Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

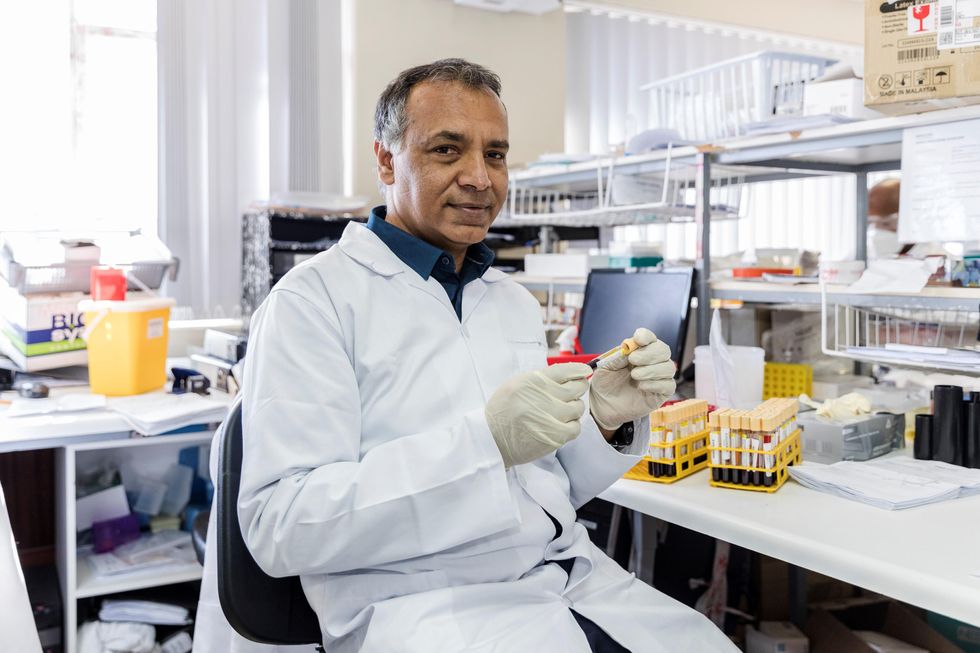
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Podcast: The Friday Five weekly roundup in health research
Researchers are making progress on a vaccine for Lyme disease, sex differences in cancer, new research on reducing your risk of dementia with leisure activities, and more in this week's Friday Five
The Friday Five covers five stories in health research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Covered in this week's Friday Five:
- Sex differences in cancer
- Promising research on a vaccine for Lyme disease
- Using a super material for brain-like devices
- Measuring your immunity to Covid
- Reducing dementia risk with leisure activities
Giving robots self-awareness as they move through space - and maybe even providing them with gene-like methods for storing rules of behavior - could be important steps toward creating more intelligent machines.
One day in recent past, scientists at Columbia University’s Creative Machines Lab set up a robotic arm inside a circle of five streaming video cameras and let the robot watch itself move, turn and twist. For about three hours the robot did exactly that—it looked at itself this way and that, like toddlers exploring themselves in a room full of mirrors. By the time the robot stopped, its internal neural network finished learning the relationship between the robot’s motor actions and the volume it occupied in its environment. In other words, the robot built a spatial self-awareness, just like humans do. “We trained its deep neural network to understand how it moved in space,” says Boyuan Chen, one of the scientists who worked on it.
For decades robots have been doing helpful tasks that are too hard, too dangerous, or physically impossible for humans to carry out themselves. Robots are ultimately superior to humans in complex calculations, following rules to a tee and repeating the same steps perfectly. But even the biggest successes for human-robot collaborations—those in manufacturing and automotive industries—still require separating the two for safety reasons. Hardwired for a limited set of tasks, industrial robots don't have the intelligence to know where their robo-parts are in space, how fast they’re moving and when they can endanger a human.
Over the past decade or so, humans have begun to expect more from robots. Engineers have been building smarter versions that can avoid obstacles, follow voice commands, respond to human speech and make simple decisions. Some of them proved invaluable in many natural and man-made disasters like earthquakes, forest fires, nuclear accidents and chemical spills. These disaster recovery robots helped clean up dangerous chemicals, looked for survivors in crumbled buildings, and ventured into radioactive areas to assess damage.
Now roboticists are going a step further, training their creations to do even better: understand their own image in space and interact with humans like humans do. Today, there are already robot-teachers like KeeKo, robot-pets like Moffin, robot-babysitters like iPal, and robotic companions for the elderly like Pepper.
But even these reasonably intelligent creations still have huge limitations, some scientists think. “There are niche applications for the current generations of robots,” says professor Anthony Zador at Cold Spring Harbor Laboratory—but they are not “generalists” who can do varied tasks all on their own, as they mostly lack the abilities to improvise, make decisions based on a multitude of facts or emotions, and adjust to rapidly changing circumstances. “We don’t have general purpose robots that can interact with the world. We’re ages away from that.”
Robotic spatial self-awareness – the achievement by the team at Columbia – is an important step toward creating more intelligent machines. Hod Lipson, professor of mechanical engineering who runs the Columbia lab, says that future robots will need this ability to assist humans better. Knowing how you look and where in space your parts are, decreases the need for human oversight. It also helps the robot to detect and compensate for damage and keep up with its own wear-and-tear. And it allows robots to realize when something is wrong with them or their parts. “We want our robots to learn and continue to grow their minds and bodies on their own,” Chen says. That’s what Zador wants too—and on a much grander level. “I want a robot who can drive my car, take my dog for a walk and have a conversation with me.”

Columbia scientists have trained a robot to become aware of its own "body," so it can map the right path to touch a ball without running into an obstacle, in this case a square.
Jane Nisselson and Yinuo Qin/ Columbia Engineering
Today’s technological advances are making some of these leaps of progress possible. One of them is the so-called Deep Learning—a method that trains artificial intelligence systems to learn and use information similar to how humans do it. Described as a machine learning method based on neural network architectures with multiple layers of processing units, Deep Learning has been used to successfully teach machines to recognize images, understand speech and even write text.
Trained by Google, one of these language machine learning geniuses, BERT, can finish sentences. Another one called GPT3, designed by San Francisco-based company OpenAI, can write little stories. Yet, both of them still make funny mistakes in their linguistic exercises that even a child wouldn’t. According to a paper published by Stanford’s Center for Research on Foundational Models, BERT seems to not understand the word “not.” When asked to fill in the word after “A robin is a __” it correctly answers “bird.” But try inserting the word “not” into that sentence (“A robin is not a __”) and BERT still completes it the same way. Similarly, in one of its stories, GPT3 wrote that if you mix a spoonful of grape juice into your cranberry juice and drink the concoction, you die. It seems that robots, and artificial intelligence systems in general, are still missing some rudimentary facts of life that humans and animals grasp naturally and effortlessly.
How does one give robots a genome? Zador has an idea. We can’t really equip machines with real biological nucleotide-based genes, but we can mimic the neuronal blueprint those genes create.
It's not exactly the robots’ fault. Compared to humans, and all other organisms that have been around for thousands or millions of years, robots are very new. They are missing out on eons of evolutionary data-building. Animals and humans are born with the ability to do certain things because they are pre-wired in them. Flies know how to fly, fish knows how to swim, cats know how to meow, and babies know how to cry. Yet, flies don’t really learn to fly, fish doesn’t learn to swim, cats don’t learn to meow, and babies don’t learn to cry—they are born able to execute such behaviors because they’re preprogrammed to do so. All that happens thanks to the millions of years of evolutions wired into their respective genomes, which give rise to the brain’s neural networks responsible for these behaviors. Robots are the newbies, missing out on that trove of information, Zador argues.
A neuroscience professor who studies how brain circuitry generates various behaviors, Zador has a different approach to developing the robotic mind. Until their creators figure out a way to imbue the bots with that information, robots will remain quite limited in their abilities. Each model will only be able to do certain things it was programmed to do, but it will never go above and beyond its original code. So Zador argues that we have to start giving robots a genome.
How does one do that? Zador has an idea. We can’t really equip machines with real biological nucleotide-based genes, but we can mimic the neuronal blueprint those genes create. Genomes lay out rules for brain development. Specifically, the genome encodes blueprints for wiring up our nervous system—the details of which neurons are connected, the strength of those connections and other specs that will later hold the information learned throughout life. “Our genomes serve as blueprints for building our nervous system and these blueprints give rise to a human brain, which contains about 100 billion neurons,” Zador says.
If you think what a genome is, he explains, it is essentially a very compact and compressed form of information storage. Conceptually, genomes are similar to CliffsNotes and other study guides. When students read these short summaries, they know about what happened in a book, without actually reading that book. And that’s how we should be designing the next generation of robots if we ever want them to act like humans, Zador says. “We should give them a set of behavioral CliffsNotes, which they can then unwrap into brain-like structures.” Robots that have such brain-like structures will acquire a set of basic rules to generate basic behaviors and use them to learn more complex ones.
Currently Zador is in the process of developing algorithms that function like simple rules that generate such behaviors. “My algorithms would write these CliffsNotes, outlining how to solve a particular problem,” he explains. “And then, the neural networks will use these CliffsNotes to figure out which ones are useful and use them in their behaviors.” That’s how all living beings operate. They use the pre-programmed info from their genetics to adapt to their changing environments and learn what’s necessary to survive and thrive in these settings.
For example, a robot’s neural network could draw from CliffsNotes with “genetic” instructions for how to be aware of its own body or learn to adjust its movements. And other, different sets of CliffsNotes may imbue it with the basics of physical safety or the fundamentals of speech.
At the moment, Zador is working on algorithms that are trying to mimic neuronal blueprints for very simple organisms—such as earthworms, which have only 302 neurons and about 7000 synapses compared to the millions we have. That’s how evolution worked, too—expanding the brains from simple creatures to more complex to the Homo Sapiens. But if it took millions of years to arrive at modern humans, how long would it take scientists to forge a robot with human intelligence? That’s a billion-dollar question. Yet, Zador is optimistic. “My hypotheses is that if you can build simple organisms that can interact with the world, then the higher level functions will not be nearly as challenging as they currently are.”
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

