Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
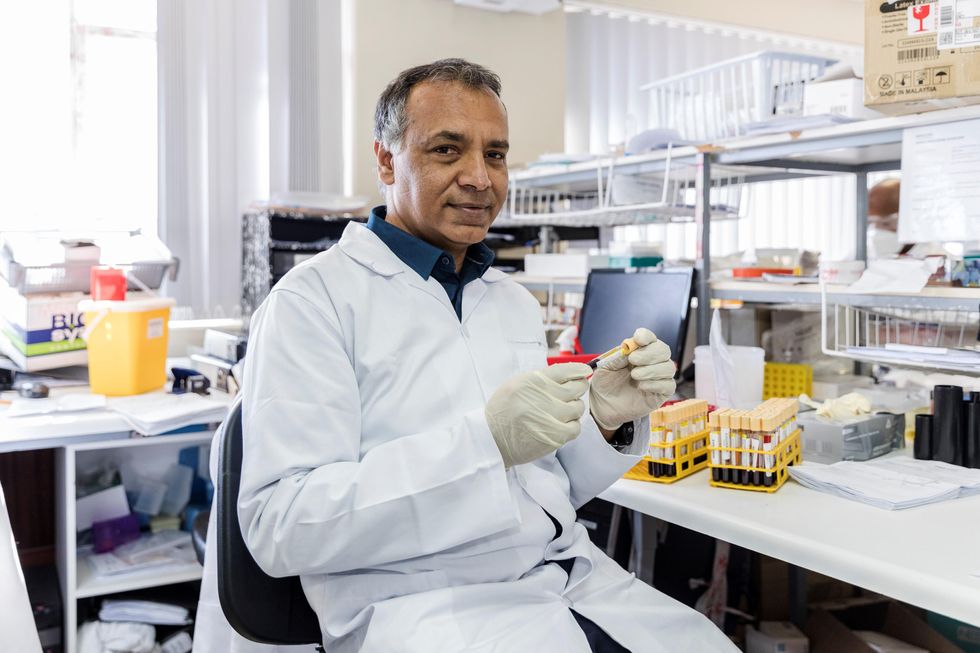
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Real-Time Monitoring of Your Health Is the Future of Medicine
Implantable sensors and other surveillance technologies offer tremendous health benefits -- and ethical challenges.
The same way that it's harder to lose 100 pounds than it is to not gain 100 pounds, it's easier to stop a disease before it happens than to treat an illness once it's developed.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
Bio-engineers working on the next generation of diagnostic tools say today's technology, such as colonoscopies or mammograms, are reactionary; that is, they tell a person they are sick often when it's too late to reverse course. Surveillance medicine — such as implanted sensors — will detect disease at its onset, in real time.
What Is Possible?
Ever since the Human Genome Project — which concluded in 2003 after mapping the DNA sequence of all 30,000 human genes — modern medicine has shifted to "personalized medicine." Also called, "precision health," 21st-century doctors can in some cases assess a person's risk for specific diseases from his or her DNA. The information enables women with a BRCA gene mutation, for example, to undergo more frequent screenings for breast cancer or to pro-actively choose to remove their breasts, as a "just in case" measure.
But your DNA is not always enough to determine your risk of illness. Not all genetic mutations are harmful, for example, and people can get sick without a genetic cause, such as with an infection. Hence the need for a more "real-time" way to monitor health.
Aaron Morris, a postdoctoral researcher in the Department of Biomedical Engineering at the University of Michigan, wants doctors to be able to predict illness with pinpoint accuracy well before symptoms show up. Working in the lab of Dr. Lonnie Shea, the team is building "a tiny diagnostic lab" that can live under a person's skin and monitor for illness, 24/7. Currently being tested in mice, the Michigan team's porous biodegradable implant becomes part of the body as "cells move right in," says Morris, allowing engineered tissue to be biopsied and analyzed for diseases. The information collected by the sensors will enable doctors to predict disease flareups, such as for cancer relapses, so that therapies can begin well before a person comes out of remission. The technology will also measure the effectiveness of those therapies in real time.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
While it may be four or five decades before Morris' sensor becomes mainstream, "the age of surveillance medicine is here," says Jamie Metzl, a technology and healthcare futurist who penned Hacking Darwin: Genetic Engineering and the Future of Humanity. "It will get more effective and sophisticated and less obtrusive over time," says Metzl.
Already, Google compiles public health data about disease hotspots by amalgamating individual searches for medical symptoms; pill technology can digitally track when and how much medication a patient takes; and, the Apple watch heart app can predict with 85-percent accuracy if an individual using the wrist device has Atrial Fibrulation (AFib) — a condition that causes stroke, blood clots and heart failure, and goes undiagnosed in 700,000 people each year in the U.S.
"We'll never be able to predict everything," says Metzl. "But we will always be able to predict and prevent more and more; that is the future of healthcare and medicine."
Morris believes that within ten years there will be surveillance tools that can predict if an individual has contracted the flu well before symptoms develop.
At City College of New York, Ryan Williams, assistant professor of biomedical engineering, has built an implantable nano-sensor that works with a florescent wand to scope out if cancer cells are growing at the implant site. "Instead of having the ovary or breast removed, the patient could just have this [surveillance] device that can say 'hey we're monitoring for this' in real-time… [to] measure whether the cancer is maybe coming back,' as opposed to having biopsy tests or undergoing treatments or invasive procedures."
Not all surveillance technologies that are being developed need to be implanted. At Case Western, Colin Drummond, PhD, MBA, a data scientist and assistant department chair of the Department of Biomedical Engineering, is building a "surroundable." He describes it as an Alexa-style surveillance system (he's named her Regina) that will "tell" the user, if a need arises for medication, how much to take and when.
Bioethical Red Flags
"Everyone should be extremely excited about our move toward what I call predictive and preventive health care and health," says Metzl. "We should also be worried about it. Because all of these technologies can be used well and they can [also] be abused." The concerns are many layered:
Discriminatory practices
For years now, bioethicists have expressed concerns about employee-sponsored wellness programs that encourage fitness while also tracking employee health data."Getting access to your health data can change the way your employer thinks about your employability," says Keisha Ray, assistant professor at the University of Texas Health Science Center at Houston (UTHealth). Such access can lead to discriminatory practices against employees that are less fit. "Surveillance medicine only heightens those risks," says Ray.
Who owns the data?
Surveillance medicine may help "democratize healthcare" which could be a good thing, says Anita Ho, an associate professor in bioethics at both the University of California, San Francisco and at the University of British Columbia. It would enable easier access by patients to their health data, delivered to smart phones, for example, rather than waiting for a call from the doctor. But, she also wonders who will own the data collected and if that owner has the right to share it or sell it. "A direct-to-consumer device is where the lines get a little blurry," says Ho. Currently, health data collected by Apple Watch is owned by Apple. "So we have to ask bigger ethical questions in terms of what consent should be required" by users.
Insurance coverage
"Consumers of these products deserve some sort of assurance that using a product that will predict future needs won't in any way jeopardize their ability to access care for those needs," says Hastings Center bioethicist Carolyn Neuhaus. She is urging lawmakers to begin tackling policy issues created by surveillance medicine, now, well ahead of the technology becoming mainstream, not unlike GINA, the Genetic Information Nondiscrimination Act of 2008 -- a federal law designed to prevent discrimination in health insurance on the basis of genetic information.
And, because not all Americans have insurance, Ho wants to know, who's going to pay for this technology and how much will it cost?
Trusting our guts
Some bioethicists are concerned that surveillance technology will reduce individuals to their "risk profiles," leaving health care systems to perceive them as nothing more than a "bundle of health and security risks." And further, in our quest to predict and prevent ailments, Neuhaus wonders if an over-reliance on data could damage the ability of future generations to trust their gut and tune into their own bodies?
It "sounds kind of hippy-dippy and feel-goodie," she admits. But in our culture of medicine where efficiency is highly valued, there's "a tendency to not value and appreciate what one feels inside of their own body … [because] it's easier to look at data than to listen to people's really messy stories of how they 'felt weird' the other day. It takes a lot less time to look at a sheet, to read out what the sensor implanted inside your body or planted around your house says."
Ho, too, worries about lost narratives. "For surveillance medicine to actually work we have to think about how we educate clinicians about the utility of these devices and how to how to interpret the data in the broader context of patients' lives."
Over-diagnosing
While one of the goals of surveillance medicine is to cut down on doctor visits, Ho wonders if the technology will have the opposite effect. "People may be going to the doctor more for things that actually are benign and are really not of concern yet," says Ho. She is also concerned that surveillance tools could make healthcare almost "recreational" and underscores the importance of making sure that the goals of surveillance medicine are met before the technology is unleashed.
"We can't just assume that any of these technologies are inherently technologies of liberation."
AI doesn't fix existing healthcare problems
"Knowing that you're going to have a fall or going to relapse or have a disease isn't all that helpful if you have no access to the follow-up care and you can't afford it and you can't afford the prescription medication that's going to ward off the onset," says Neuhaus. "It may still be worth knowing … but we can't fool ourselves into thinking that this technology is going to reshape medicine in America if we don't pay attention to … the infrastructure that we don't currently have."
Race-based medicine
How surveillances devices are tested before being approved for human use is a major concern for Ho. In recent years, alerts have been raised about the homogeneity of study group participants — too white and too male. Ho wonders if the devices will be able to "accurately predict the disease progression for people whose data has not been used in developing the technology?" COVID-19 has killed Black people at a rate 2.5 time greater than white people, for example, and new, virtual clinical research is focused on recruiting more people of color.
The Biggest Question
"We can't just assume that any of these technologies are inherently technologies of liberation," says Metzl.
Especially because we haven't yet asked the 64-thousand dollar question: Would patients even want to know?
Jenny Ahlstrom is an IT professional who was diagnosed at 43 with multiple myeloma, a blood cancer that typically attacks people in their late 60s and 70s and for which there is no cure. She believes that most people won't want to know about their declining health in real time. People like to live "optimistically in denial most of the time. If they don't have a problem, they don't want to really think they have a problem until they have [it]," especially when there is no cure. "Psychologically? That would be hard to know."
Ahlstrom says there's also the issue of trust, something she experienced first-hand when she launched her non-profit, HealthTree, a crowdsourcing tool to help myeloma patients "find their genetic twin" and learn what therapies may or may not work. "People want to share their story, not their data," says Ahlstrom. "We have been so conditioned as a nation to believe that our medical data is so valuable."
Metzl acknowledges that adoption of new technologies will be uneven. But he also believes that "over time, it will be abundantly clear that it's much, much cheaper to predict and prevent disease than it is to treat disease once it's already emerged."
Beyond cost, the tremendous potential of these technologies to help us live healthier and longer lives is a game-changer, he says, as long as we find ways "to ultimately navigate this terrain and put systems in place ... to minimize any potential harms."
How Smallpox Was Wiped Off the Planet By a Vaccine and Global Cooperation
The world's last recorded case of endemic smallpox was in Ali Maow Maalin, of Merka, Somalia, in October 1977. He made a full recovery.
For 3000 years, civilizations all over the world were brutalized by smallpox, an infectious and deadly virus characterized by fever and a rash of painful, oozing sores.
Doctors had to contend with wars, floods, and language barriers to make their campaign a success.
Smallpox was merciless, killing one third of people it infected and leaving many survivors permanently pockmarked and blind. Although smallpox was more common during the 18th and 19th centuries, it was still a leading cause of death even up until the early 1950s, killing an estimated 50 million people annually.
A Primitive Cure
Sometime during the 10th century, Chinese physicians figured out that exposing people to a tiny bit of smallpox would sometimes result in a milder infection and immunity to the disease afterward (if the person survived). Desperate for a cure, people would huff powders made of smallpox scabs or insert smallpox pus into their skin, all in the hopes of getting immunity without having to get too sick. However, this method – called inoculation – didn't always work. People could still catch the full-blown disease, spread it to others, or even catch another infectious disease like syphilis in the process.
A Breakthrough Treatment
For centuries, inoculation – however imperfect – was the only protection the world had against smallpox. But in the late 18th century, an English physician named Edward Jenner created a more effective method. Jenner discovered that inoculating a person with cowpox – a much milder relative of the smallpox virus – would make that person immune to smallpox as well, but this time without the possibility of actually catching or transmitting smallpox. His breakthrough became the world's first vaccine against a contagious disease. Other researchers, like Louis Pasteur, would use these same principles to make vaccines for global killers like anthrax and rabies. Vaccination was considered a miracle, conferring all of the rewards of having gotten sick (immunity) without the risk of death or blindness.
Scaling the Cure
As vaccination became more widespread, the number of global smallpox deaths began to drop, particularly in Europe and the United States. But even as late as 1967, smallpox was still killing anywhere from 10 to 15 million people in poorer parts of the globe. The World Health Assembly (a decision-making body of the World Health Organization) decided that year to launch the first coordinated effort to eradicate smallpox from the planet completely, aiming for 80 percent vaccine coverage in every country in which the disease was endemic – a total of 33 countries.
But officials knew that eradicating smallpox would be easier said than done. Doctors had to contend with wars, floods, and language barriers to make their campaign a success. The vaccination initiative in Bangladesh proved the most challenging, due to its population density and the prevalence of the disease, writes journalist Laurie Garrett in her book, The Coming Plague.
In one instance, French physician Daniel Tarantola on assignment in Bangladesh confronted a murderous gang that was thought to be spreading smallpox throughout the countryside during their crime sprees. Without police protection, Tarantola confronted the gang and "faced down guns" in order to immunize them, protecting the villagers from repeated outbreaks.
Because not enough vaccines existed to vaccinate everyone in a given country, doctors utilized a strategy called "ring vaccination," which meant locating individual outbreaks and vaccinating all known and possible contacts to stop an outbreak at its source. Fewer than 50 percent of the population in Nigeria received a vaccine, for example, but thanks to ring vaccination, it was eradicated in that country nonetheless. Doctors worked tirelessly for the next eleven years to immunize as many people as possible.
The World Health Organization declared smallpox officially eradicated on May 8, 1980.
A Resounding Success
In November 1975, officials discovered a case of variola major — the more virulent strain of the smallpox virus — in a three-year-old Bangladeshi girl named Rahima Banu. Banu was forcibly quarantined in her family's home with armed guards until the risk of transmission had passed, while officials went door-to-door vaccinating everyone within a five-mile radius. Two years later, the last case of variola major in human history was reported in Somalia. When no new community-acquired cases appeared after that, the World Health Organization declared smallpox officially eradicated on May 8, 1980.
Because of smallpox, we now know it's possible to completely eliminate a disease. But is it likely to happen again with other diseases, like COVID-19? Some scientists aren't so sure. As dangerous as smallpox was, it had a few characteristics that made eradication possibly easier than for other diseases. Smallpox, for instance, has no animal reservoir, meaning that it could not circulate in animals and resurge in a human population at a later date. Additionally, a person who had smallpox once was guaranteed immunity from the disease thereafter — which is not the case for COVID-19.
In The Coming Plague, Japanese physician Isao Arita, who led the WHO's Smallpox Eradication Unit, admitted to routinely defying orders from the WHO, mobilizing to parts of the world without official approval and sometimes even vaccinating people against their will. "If we hadn't broken every single WHO rule many times over, we would have never defeated smallpox," Arita said. "Never."
Still, thanks to the life-saving technology of vaccines – and the tireless efforts of doctors and scientists across the globe – a once-lethal disease is now a thing of the past.