The Nose Knows: Dogs Are Being Trained to Detect the Coronavirus

Security workers walk with detection dogs in an airport terminal.
Asher is eccentric and inquisitive. He loves an audience, likes keeping busy, and howls to be let through doors. He is a six-year-old working Cocker Spaniel, who, with five other furry colleagues, has now been trained to sniff body odor samples from humans to detect COVID-19 infections.
As the Delta variant and other new versions of the SARS-CoV-2 virus emerge, public health agencies are once again recommending masking while employers contemplate mandatory vaccination. While PCR tests remain the "gold standard" of COVID-19 tests, they can take hours to flag infections. To accelerate the process, scientists are turning to a new testing tool: sniffer dogs.
At the London School of Hygiene and Tropical Medicine (LSHTM), researchers deployed Asher and five other trained dogs to test sock samples from 200 asymptomatic, infected individuals and 200 healthy individuals. In May, they published the findings of the yearlong study in a preprint, concluding that dogs could identify COVID-19 infections with a high degree of accuracy – they could correctly identify a COVID-positive sample up to 94% of the time and a negative sample up to 92% of the time. The paper has yet to be peer-reviewed.
"Dogs can screen lots of people very quickly – 300 people per dog per hour. This means they could be used in places like airports or public venues like stadiums and maybe even workplaces," says James Logan, who heads the Department of Disease Control at LSHTM, adding that canines can also detect variants of SARS-CoV-2. "We included samples from two variants and the dogs could still detect them."
Detection dogs have been one of the most reliable biosensors for identifying the odor of human disease. According to Gemma Butlin, a spokesperson of Medical Detection Dogs, the UK-based charity that trained canines for the LSHTM study, the olfactory capabilities of dogs have been deployed to detect malaria, Parkinson's disease, different types of cancers, as well as pseudomonas, a type of bacteria known to cause infections in blood, lungs, eyes, and other parts of the human body.
COVID-19 has a distinctive smell — a result of chemicals known as volatile organic compounds released by infected body cells, which give off an odor "fingerprint."
"It's estimated that the percentage of a dog's brain devoted to analyzing odors is 40 times larger than that of a human," says Butlin. "Humans have around 5 million scent receptors dedicated to smell. Dogs have 350 million and can detect odors at parts per trillion. To put this into context, a dog can detect a teaspoon of sugar in a million gallons of water: two Olympic-sized pools full."
According to LSHTM scientists, COVID-19 has a distinctive smell — a result of chemicals known as volatile organic compounds released by infected body cells, which give off an odor "fingerprint." Other studies, too, have revealed that the SARS-CoV-2 virus has a distinct olfactory signature, detectable in the urine, saliva, and sweat of infected individuals. Humans can't smell the disease in these fluids, but dogs can.
"Our research shows that the smell associated with COVID-19 is at least partly due to small and volatile chemicals that are produced by the virus growing in the body or the immune response to the virus or both," said Steve Lindsay, a public health entomologist at Durham University, whose team collaborated with LSHTM for the study. He added, "There is also a further possibility that dogs can actually smell the virus, which is incredible given how small viruses are."
In April this year, researchers from the University of Pennsylvania and collaborators published a similar study in the scientific journal PLOS One, revealing that detection dogs could successfully discriminate between urine samples of infected and uninfected individuals. The accuracy rate of canines in this study was 96%. Similarly, last December, French scientists found that dogs were 76-100% effective at identifying individuals with COVID-19 when presented with sweat samples.
Grandjean Dominique, a professor at France's National Veterinary School of Alfort, who led the French study, said that the researchers used two types of dogs — search and rescue dogs, as they can sniff sweat, and explosive detection dogs, because they're often used at airports to find bomb ingredients. Dogs may very well be as good as PCR tests, said Dominique, but the goal, he added, is not to replace these tests with canines.
In France, the government gave the green light to train hundreds of disease detection dogs and deploy them in airports. "They will act as mass pre-test, and only people who are positive will undergo a PCR test to check their level of infection and the kind of variant," says Dominique. He thinks the dogs will be able to decrease the amount of PCR testing and potentially save money.
Since the accuracy rate for bio-detection dogs is fairly high, scientists think they could prove to be a quick diagnosis and mass screening tool, especially at ports, airports, train stations, stadiums, and public gatherings. Countries like Finland, Thailand, UAE, Italy, Chile, India, Australia, Pakistan, Saudi Arabia, Switzerland, and Mexico are already training and deploying canines for COVID-19 detection. The dogs are trained to sniff the area around a person, and if they find the odor of COVID-19 they will sit or stand back from an individual as a signal that they've identified an infection.
While bio-detection dogs seem promising for cheap, large-volume screening, many of the studies that have been performed to date have been small and in controlled environments. The big question is whether this approach work on people in crowded airports, not just samples of shirts and socks in a lab.
"The next step is 'real world' testing where they [canines] are placed in airports to screen people and see how they perform," says Anna Durbin, professor of international health at the John Hopkins Bloomberg School of Public Health. "Testing in real airports with lots of passengers and competing scents will need to be done."
According to Butlin of Medical Detection Dogs, scalability could be a challenge. However, scientists don't intend to have a dog in every waiting room, detecting COVID-19 or other diseases, she said.
"Dogs are the most reliable bio sensors on the planet and they have proven time and time again that they can detect diseases as accurately, if not more so, than current technological diagnostics," said Butlin. "We are learning from them all the time and what their noses know will one day enable the creation an 'E-nose' that does the same job – imagine a day when your mobile phone can tell you that you are unwell."
Scientists search for a universal coronavirus vaccine
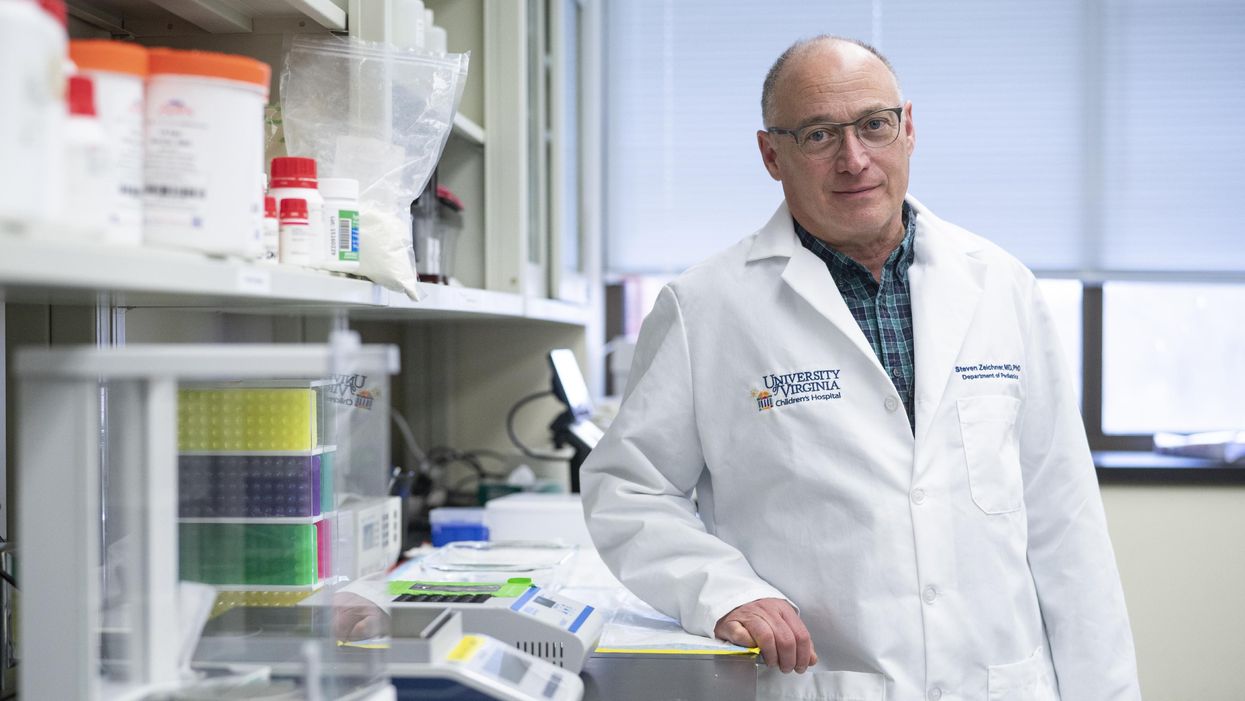
Stephen Zeichner, an infectious disease specialist at the University of Virginia Medical Center, has made progress with an early stage universal coronavirus vaccine.
The Covid-19 pandemic had barely begun when VBI Vaccines, a biopharmaceutical company based in Cambridge, Massachusetts, initiated their search for a universal coronavirus vaccine.
It was March 2020, and while most pharmaceutical companies were scrambling to initiate vaccine programs which specifically targeted the SARS-CoV-2 virus, VBI’s executives were already keen to look at the broader picture.
Having observed the SARS and MERS coronavirus outbreaks over the last two decades, Jeff Baxter, CEO of VBI Vaccines, was aware that SARS-CoV-2 is unlikely to be the last coronavirus to move from an animal host into humans. “It's absolutely apparent that the future is to create a vaccine which gives more broad protection against not only pre-existing coronaviruses, but those that will potentially make the leap into humans in future,” says Baxter.
It was a prescient decision. Over the last two years, more biotechs and pharma companies have joined the search to find a vaccine which might be able to protect against all coronaviruses, along with dozens of academic research groups. Last September, the US National Institutes of Health dedicated $36 million specifically to pan-coronavirus vaccine research, while the global Coalition for Epidemic Preparedness Innovations (CEPI) has earmarked $200 million towards the effort.
Until October 2021, the very concept of whether it might be
theoretically possible to vaccinate against multiple coronaviruses remained an open question. But then a groundbreaking study renewed optimism.
The emergence of new variants of Covid-19 over the past year, particularly the highly mutated Omicron variant, has added greater impetus to find broader spectrum vaccines. But until October 2021, the very concept of whether it might be theoretically possible to vaccinate against multiple coronaviruses remained an open question. After all, scientists have spent decades trying to develop a similar vaccine for influenza with little success.
But then a groundbreaking study from renowned virologist Linfa Wang, who runs the emerging infectious diseases program at Duke-National University of Singapore Medical School, provided renewed optimism.
Wang found that eight SARS survivors who had been injected with the Pfizer/BioNTech Covid-19 vaccine had neutralising antibodies in their blood against SARS, the Alpha, Beta and Delta variants of SARS-CoV-2, and five other coronaviruses which reside in bats and pangolins. He concluded that the combination of past coronavirus infection, and immunization with a messenger RNA vaccine, had resulted in a wider spectrum of protection than might have been expected.
“This is a significant study because it showed that pre-existing immunity to one coronavirus could help with the elicitation of cross-reactive antibodies when immunizing with a second coronavirus,” says Kevin Saunders, Director of Research at the Duke Human Vaccine Institute in North Carolina, which is developing a universal coronavirus vaccine. “It provides a strategy to perhaps broaden the immune response against coronaviruses.”
In the next few months, some of the first data is set to emerge looking at whether this kind of antibody response could be elicited by a single universal coronavirus vaccine. In April 2021, scientists at the Walter Reed Army Institute of Research in Silver Spring, Maryland, launched a Phase I clinical trial of their vaccine, with a spokesman saying that it was successful, and the full results will be announced soon.
The Walter Reed researchers have already released preclinical data, testing the vaccine in non-human primates where it was found to have immunising capabilities against a range of Covid-19 variants as well as the original SARS virus. If the Phase I trial displays similar efficacy, a larger Phase II trial will begin later this year.
Two different approaches
Broadly speaking, scientists are taking two contrasting approaches to the task of finding a universal coronavirus vaccine. The Walter Reed Army Institute of Research, VBI Vaccines – who plan to launch their own clinical trial in the summer – and the Duke Human Vaccine Institute – who are launching a Phase I trial in early 2023 – are using a soccer-ball shaped ferritin nanoparticle studded with different coronavirus protein fragments.
VBI Vaccines is looking to elicit broader immune responses by combining SARS, SARS-CoV-2 and MERS spike proteins on the same nanoparticle. Dave Anderson, chief scientific officer at VBI Vaccines, explains that the idea is that by showing the immune system these three spike proteins at the same time, it can help train it to identify and respond to subtle differences between coronavirus strains.
The Duke Human Vaccine Institute is utilising the same method, but rather than including the entire spike proteins from different coronaviruses, they are only including the receptor binding domain (RBD) fragment from each spike protein. “We designed our vaccine to focus the immune system on a site of vulnerability for the virus, which is the receptor binding domain,” says Saunders. “Since the RBD is small, arraying multiple RBDs on a nanoparticle is a straight-forward approach. The goal is to generate immunity to many different subgenuses of viruses so that there will be cross-reactivity with new or unknown coronaviruses.”
But the other strategy is to create a vaccine which contains regions of the viral protein structure which are conserved between all coronavirus strains. This is something which scientists have tried to do for a universal influenza vaccine, but it is thought to be more feasible for coronaviruses because they mutate at a slower rate and are more constrained in the ways that they can evolve.
DIOSynVax, a biotech based in Cambridge, United Kingdom, announced in a press release earlier this month that they are partnering with CEPI to use their computational predictive modelling techniques to identify common structures between all of the SARS coronaviruses which do not mutate, and thus present good vaccine targets.
Stephen Zeichner, an infectious disease specialist at the University of Virginia Medical Center, has created an early stage vaccine using the fusion peptide region – another part of the coronavirus spike protein that aids the virus’s entry into host cells – which so far appears to be highly conserved between all coronaviruses.
So far Zeichner has trialled this version of the vaccine in pigs, where it provided protection against a different coronavirus called porcine epidemic diarrhea virus, which he described as very promising as this virus is from a different family called alphacoronaviruses, while SARS-CoV-2 is a betacoronavirus.
“If a betacoronavirus fusion peptide vaccine designed from SARS-CoV-2 can protect pigs against clinical disease from an alphacoronavirus, then that suggests that an analogous vaccine would enable broad protection against many, many different coronaviruses,” he says.
The road ahead
But while some of the early stage results are promising, researchers are fully aware of the scale of the challenge ahead of them. Although CEPI have declared an aim of having a licensed universal coronavirus vaccine available by 2024-2025, Zeichner says that such timelines are ambitious in the extreme.
“I was incredibly impressed at the speed at which the mRNA coronavirus vaccines were developed for SARS-CoV-2,” he says. “That was faster than just about anybody anticipated. On the other hand, I think a universal coronavirus vaccine is more equivalent to the challenge of developing an HIV vaccine and we're 35 years into that effort without success. We know a lot more now than before, and maybe it will be easier than we think. But I think the route to a universal vaccine is harder than an individual vaccine, so I wouldn’t want to put money on a timeline prediction.”
The major challenge for scientists is essentially designing a vaccine for a future threat which is not even here yet. As such, there are no guidelines on what safety data would be required to license such a vaccine, and how researchers can demonstrate that it truly provides efficacy against all coronaviruses, even those which have not yet jumped to humans.
The teams working on this problem have already devised some ingenious ways of approaching the challenge. VBI Vaccines have taken the genetic sequences of different coronaviruses found in bats and pangolins, from publicly available databases, and inserted them into what virologists call a pseudotype virus – one which has been engineered so it does not have enough genetic material to replicate.
This has allowed them to test the neutralising antibodies that their vaccine produces against these coronaviruses in test tubes, under safe lab conditions. “We have literally just been ordering the sequences, and making synthetic viruses that we can use to test the antibody responses,” says Anderson.
However, some scientists feel that going straight to a universal coronavirus vaccine is likely to be too complex. Instead they say that we should aim for vaccines which are a little more specific. Pamela Bjorkman, a structural biologist at the California Institute of Technology, suggests that pan-coronavirus vaccines which protect against SARS-like betacoronaviruses such as SARS or SARS-CoV-2, or MERS-like betacoronaviruses, may be more realistic.
“I think a vaccine to protect against all coronaviruses is likely impossible since there are so many varieties,” she says. “Perhaps trying to narrow down the scope is advisable.”
But if the mission to develop a universal coronavirus vaccine does succeed, it will be one of the most remarkable feats in the annals of medical science. In January, US chief medical advisor Anthony Fauci urged for greater efforts to be devoted towards this goal, one which scientists feel would be the biological equivalent of the race to develop the first atomic bomb
“The development of an effective universal coronavirus vaccine would be equally groundbreaking, as it would have global applicability and utility,” says Saunders. “Coronaviruses have caused multiple deadly outbreaks, and it is likely that another outbreak will occur. Having a vaccine that prevents death from a future outbreak would be a tremendous achievement in global health.”
He agrees that it will require creativity on a remarkable scale: “The universal coronavirus vaccine will also require ingenuity and perseverance comparable to that needed for the Manhattan project.”
This month, Matt Fuchs becomes the new Editor-in-Chief of Leaps.org.
This month, Kira Peikoff passes the torch to me as editor-in-chief of Leaps.org. I’m excited to assume leadership of this important platform.
Leaps.org caught my eye back in 2018. I was in my late 30s and just starting to wake up to the reality that the people I care most about were getting older and more vulnerable to health problems. At the same time, three critical shifts were becoming impossible to ignore. First, the average age in the U.S. is getting older, a trend known as the “gray tsunami.” Second, healthcare expenses are escalating and becoming unsustainable. And third, our sedentary, stress-filled lifestyles are leading to devastating consequences.
These trends pointed to a future filled with disease, suffering and economic collapse. But whenever I visited Leaps.org, my outlook turned from gloomy to solution-oriented. I became just as fascinated in a fourth trend, one that stands to revolutionize our world: rapid, mind-bending innovations in health and medicine.
Brain atlases, genome sequencing and editing, AI, protein mapping, synthetic biology, 3-D printing—these technologies are yielding new opportunities for health, longevity and human thriving. COVID-19 has caused many setbacks, but it has accelerated scientific breakthroughs. History suggests we will see even more innovation—in digital health and virtual first care, for example—after the pandemic.
In 2020, I began covering these developments with articles for Leaps.org about clocks that measure biological aging, gene therapies for cystic fibrosis, and other seemingly futuristic concepts that are transforming the present. I wrote about them partly because I think most people aren’t aware of them—and meaningful progress can’t happen without public engagement. A broader set of stakeholders and society at large, not just the experts, must inform these changes to ensure that they reflect our values and ethics. Everyone should get the chance to participate in the conversation—and they must have the opportunity to benefit equally from the innovations we decide to move forward with. By highlighting cutting-edge advances, Leaps.org is helping to realize this important goal.
Meanwhile, as I wrote freelance pieces on health and wellness for outlets such as the Washington Post and Time Magazine, I kept seeing an intersect between the breakthroughs in research labs and our expanding knowledge about the science of well-being. Take, for example, emerging technologies designed to stop illnesses in their tracks and new research on the benefits of taking in natural daylight. These two areas, lab innovations and healthy lifestyles, both shift the focus from disease treatment to disease prevention and optimal health. It’s the only sensible, financially feasible way forward.
When Kira suggested that I consider a leadership role with Leaps.org, it struck me how much the platform’s ideals have informed my own perspectives. The frontpage gore of mainstream media outlets can feel like a daily dose of pessimism, with cynicism sometimes dressed up as wisdom. Leaps.org’s world view is rooted in something very different: rational optimism about the present moment and the possibility of human flourishing.
That’s why I’m proud to lead this platform, including our podcast, Making Sense of Science, and hope you’ll keep coming to Leaps.org to learn and join the conversation about scientific gamechangers through our sponsored events, our popular Instagram account and other social channels. Think critically about the breakthroughs and their ethical challenges. Help usher in the health and prosperity that could be ours if we stay open-minded to it.
Yours truly,
Matt Fuchs
Editor-in-Chief