Your Questions Answered About Kids, Teens, and Covid Vaccines
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

On May 13th, scientific and medical experts will discuss and answer questions about the vaccine for those under 16.
This virtual event convened leading scientific and medical experts to address the public's questions and concerns about Covid-19 vaccines in kids and teens. Highlight video below.
DATE:
Thursday, May 13th, 2021
12:30 p.m. - 1:45 p.m. EDT
Dr. H. Dele Davies, M.D., MHCM

Senior Vice Chancellor for Academic Affairs and Dean for Graduate Studies at the University of Nebraska Medical (UNMC). He is an internationally recognized expert in pediatric infectious diseases and a leader in community health.
Dr. Emily Oster, Ph.D.

Professor of Economics at Brown University. She is a best-selling author and parenting guru who has pioneered a method of assessing school safety.
Dr. Tina Q. Tan, M.D.

Professor of Pediatrics at the Feinberg School of Medicine, Northwestern University. She has been involved in several vaccine survey studies that examine the awareness, acceptance, barriers and utilization of recommended preventative vaccines.
Dr. Inci Yildirim, M.D., Ph.D., M.Sc.

Associate Professor of Pediatrics (Infectious Disease); Medical Director, Transplant Infectious Diseases at Yale School of Medicine; Associate Professor of Global Health, Yale Institute for Global Health. She is an investigator for the multi-institutional COVID-19 Prevention Network's (CoVPN) Moderna mRNA-1273 clinical trial for children 6 months to 12 years of age.
About the Event Series
This event is the second of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
:
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
You Saw the Grammys, But You Missed the More Important Awards
The 2018 Stem Cell Action Awards, honoring recipients for advocacy, leadership, and inspiration, presented by the Regenerative Medicine Foundation.
Last week in Miami, more than 450 researchers, physicians, lawyers, ethicists, and executives gathered from far-flung corners of the globe to share the latest updates in stem cell research and regenerative medicine. Sure, a science conference might not seem as glamorous as a celebrity-filled Madison Square Garden, but it's the place to be if you care about breakthroughs that could give you a longer and healthier life. Here are our top ten takeaways about what's hot and what's happening worldwide:
"The places you least expect will turn up to produce some really extraordinary things."
1) The future of stem cell treatment may involve the creation of a universal cell line that is genetically modified so every patient's immune system will accept it.
One of the leading scientists at the convention, Japanese stem cell pioneer Dr. Norio Nakatsuji, dubbed this quest a "very hot topic" right now. Being able to produce one safe cell line for everyone would be much cheaper and faster than having to create and grow patient-specific cells. "It is theoretically possible to genetically modify the lines so everyone can accept them," said Nakatsuji. A Seattle-based biotech company aptly named Universal Cells is leading the way in this promising area.
2) Japan was the world leader in stem cell research 10 years ago, but has since fallen behind the United States for reasons that some researchers find frustrating.
Japan is not a particularly religious society, so their culture does not object on principle to using donated human embryos for the creation of stem cells, and federal money can fund such research, unlike in the U.S. But the irony, according to Nakatsuji, is that the regulations for researchers are still very cumbersome. "We need to clear many probably unnecessary steps," he said. For example, before starting work in the field, new graduate students need special training and ethics lectures, and must be cleared by a committee; the process could take six months before an experiment can start, whereas in a country like Britain, scientists can immediately begin.
Also: back in 2006, a Japanese researcher who later won the Nobel Prize managed to reprogram 4 genes in adult cells and essentially turn back time, reversing the cells back to an embryonic state. The implications of this breakthrough were enormous, because destroying an embryo was no longer required to generate blank cells with unlimited potential—and these cells could now be created directly from a patient.
But then "a very unfortunate situation" happened in Japan, says Nakatsuji. There was a fever for these induced pluripotent (iPS) cells, and many Japanese researchers thought embryonic stem cell research was no longer important.
"This is a misconception," Nakatsuji lamented. "You do need both cell types." Embryonic stem cells, unlike their artificially made alternatives, are still safer and more reliable. A symbolic example, he said, is that groups in the U.S. and Europe are starting trials for Parkinson's disease that require dopamine-secreting neurons from stem cells. The researchers could have chosen iPS cells, but went with embryonic stem cells.
The main advantage now of iPS cells, Nakatsuji said, is not for therapeutic purposes, but for drug discovery and creating models of disease based on specific patient profiles.

Dr. Norio Nakatsuji receiving an award for international leadership from Bernard Siegel, the founder and director of the Regenerative Medicine Foundation.
3) In China, rampant stem cell tourism in 2009 led to disaster and a total government shutdown, from which the research field is only recently starting to recover.
Stem cell therapy in China "used to be totally unethical but then took a shock and is still recovering from that shock," said Dr. Wenchun Qu, a physician-researcher at the Mayo Clinic. Scam clinics profited off unapproved and unproven treatments which killed some patients until the total ban set in. Now, the research field is slowly coming back on board under strict regulation; there were only 35 clinical trial with stem cells in 2016, whereas in the U.S, there were more than 2000.
"A lack of public trust and deception is the number one factor" in China's falling behind, said Dr. Yen-Michael Hsu of Weill Cornell. "China is catching up trying to rebuild trust with the taxpayers."
As of last November, 102 designated institutions in China can conduct stem cell research only--not offer commercialized treatments. Bottom line: China is advancing fast in basic science and even leading in some areas, yet is trailing other countries in translational studies and clinical practice.
4) The Bahamas is emerging as a hub of legitimate research that is attracting innovative new trials.
A regulatory framework and National Stem Cell Ethics Committee were established around 2013, and since then, clinical research in the Bahamas has begun; the focus is on safety and efficacy, with standards high enough to satisfy the FDA, but also streamlined enough to allow for trials to proceed faster than they might in other countries.
One U.S.-based company, Advanced Regen Medical Technologies, is pursuing a proprietary cell culture that rejuvenates old cells by exposing them to young donor cells, with the goal of extending healthy living. On May 24th, 2017, the company presented to the National Stem Cell Ethics Committee, and on December 15th, they treated their first patient.
"Here's an indication that would be frankly impossible to get through the FDA and certainly not without many years of pain," said Marc Penn, a leader of the company's executive team. "We were able to get through the National Stem Cell Ethics Committee with all of us feeling good about the level of rigor within a seven-to-eight month span."
Desiree Cox, the chairwoman of the Committee, stressed the selectiveness and rigor with which the Bahamas is approaching new trial applications. Of 20 proposed stem cell trials, they have approved only four.
"We're interested in first-in-man studies, things that are breaking the boundaries, going beyond what is already done elsewhere, linking to predictive analytics," she said. "The places you least expect will turn up to produce some really extraordinary things."
Another active clinical trial there is a phase 1 study for Aging Frailty run by a Miami-based start-up called Longeveron. "Our experience is it comes as a huge relief to many people to have the opportunity to go to such a program rather than wait for a drug to be approved in the U.S.," said Dr. Joshua Hare, the director of the Interdisciplinary Stem Cell Institute at the University of Miami and the co-founder and Chief Science Officer at Longeveron.
"The challenge right now is the effective translation and development of viable stem-cell based therapies."
5) Researchers are working on building an artificial heart with stem cells, but technology is not the only hurdle.
A group at the Texas Heart Institute in Houston is experimenting with this strategy: stripping a real heart organ of its cells, then repopulating it with blood-forming stem cells, and implanting it. In cows, this approach has worked successfully. But one problem, said Dr. Doris Taylor, the director of Regenerative Medicine Research at the Institute, is educating regulators, since this kind of treatment is not a drug and not a device.
That said, when will we see someone order a heart off the shelf?
"I think in the next two years," she said, "you will see exciting things happening at least at the level of congenital heart disease, if not adult hearts."
6) Cost is a major barrier to regenerative medicine's success.
"It's not about whether you can get enough of the cells you need, it's about whether you can get them for less than one million dollars," Taylor said wryly.
Cell therapies intended for patients must be manufactured in a special facility to generate the quantity necessary for treatment. Some experts expressed concerned that these bio-manufacturing facilities are like "the Wild West" right now because there is no standard for pricing.
Some companies are "getting away with murder," said Dr. Camillo Ricordi, director of the Diabetes Research Institute. "This doesn't happen in most of the rest of the world."
7) Media hype has caused the premature (and potentially dangerous) commercialization of unproven stem cell therapies.
There are now over 570 such clinics operating in the U.S., with hot spots in Florida and California, which offer up stem cells for everything from sports medicine and vitamins to beauty products and pet health.
In fact, according to the FDA, the only stem cell-based products currently approved for use consist of blood-forming stem cells derived from cord blood. Everything else, for now, is still experimental.
While plenty of legitimate research is moving ahead in clinical trials, consumers may be confused by the plethora of scam clinics. But since last August, the FDA has begun cracking down, issuing three enforcement actions.
Also worth noting: what the marketplace refers to as "stem cells" are in fact products that contain a very low amount of concentrated adult stem cells derived from fat or bone marrow. There are no pure stem cell products out there.
"The challenge right now is the effective translation and development of viable stem-cell based therapies," said Dr. Shane Shapiro, a sports medicine physician at the Mayo Clinic.
What constitutes a genetically modified organism? Europe is in the process of deciding.
8) An exciting coming trend is induced tissue regeneration.
The company AgeX, run by gerontologist and stem cell pioneer Dr. Mike West, is in preclinical trials for a treatment that can reset the regenerative potential of mature tissue.
This ability is lost in the early stages of life to help prevent cancer, but AgeX is interested in figuring out a way to restore it with pluripotent stem cells in adult tissue, to correct the damage incurred by aging. West said he expects the program to reach human clinical trials in the next five years.
9) Stem cells alone are not the whole story.
The future of cell therapy will involve cell derivatives—the things that cells secrete, like exosomes, microRNA, and viruses, that can be better controlled than the cells themselves.
Exosomes, which are extracellular vesicles released from cells, act as fingerprints that are useful for diagnosis and therapy, said Dr. Li Chen, the head of the Human Liver Cell Lab at the University of California-San Diego. Because exosomes are smaller than cells, they can also cross the blood-brain barrier.
Europe is the leading place for exosome research. Recently, a 21-year-old boy suffering from brain cancer there was treated with stem cell therapy, which failed, but then subsequently he received surgery with exosomes applied to his tumor, and he survived.
10) The European Union is in the process of deciding what legally constitutes a "genetically modified organism" – and the stakes are high.
The European Court of Justice, the EU's highest court, is considering this question: If a modification brought about by genetic engineering technology could also have occurred naturally, should the resulting organism be considered a GMO?
Just last week, an advocate general of the court proposed that whenever an organism is manmade that could theoretically occur naturally, it should not be considered a GMO, and therefore should not be subjected to such regulations.
If the Court agrees with the advice of its advocate general later this year, then the decision would have huge implications for biotech agriculture across Europe, paving the way for gene-edited crops to hit the market.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Aubrey de Grey at the World Stem Cell Summit in Miami on January 25, 2018.
Aging is not a mystery, says famed researcher Dr. Aubrey de Grey, perhaps the world's foremost advocate of the provocative view that medical technology will one day allow humans to control the aging process and live healthily into our hundreds—or even thousands.
"The cultural attitudes toward all of this are going to be completely turned upside down by sufficiently promising results in the lab, in mice."
He likens aging to a car wearing down over time; as the body operates normally, it accumulates damage which can be tolerated for a while, but eventually sends us into steep decline. The most promising way to escape this biological reality, he says, is to repair the damage as needed with precise scientific tools.
The bad news is that doing this groundbreaking research takes a long time and a lot of money, which has not always been readily available, in part due to a cultural phenomenon he terms "the pro-aging trance." Cultural attitudes have long been fatalistic about the inevitability of aging; many people balk at the seemingly implausible prospect of indefinite longevity.
But the good news for de Grey—and those who are cheering him on—is that his view is becoming less radical these days. Both the academic and private sectors are racing to tackle aging; his own SENS Research Foundation, for one, has spun out into five different companies. Defeating aging, he says, "is not just a future industry; it's an industry now that will be both profitable and extremely good for your health."
De Grey sat down with Editor-in-Chief Kira Peikoff at the World Stem Cell Summit in Miami to give LeapsMag the latest scoop on his work. Here is an edited and condensed version of our conversation.
Since your book Ending Aging was published a decade ago, scientific breakthroughs in stem cell research, genome editing, and other fields have taken the world by storm. Which of these have most affected your research?
They have all affected it a lot in one way, and hardly at all in another way. They have speeded it up--facilitated short cuts, ways to get where we're already trying to go. What they have not done is identified any fundamental changes to the overall strategy. In the book, we described the seven major types of damage, and particular ways of going about fixing each of them, and that hasn't changed.
"Repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells."
Has any breakthrough specifically made the biggest impact?
It's not just the obvious things, like iPS (induced pluripotent stem cells) and CRISPR (a precise tool for editing genes). It's also the more esoteric things that applied specifically to certain of our areas, but most people don't really know about them. For example, the identification of how to control something called co-translational mitochondrial protein import.
How much of the future of anti-aging treatments will involve regeneration of old tissue, or wholesale growth of new organs?
The more large-scale ones, regenerating whole new organs, are probably only going to play a role in the short-term and will be phased out relatively rapidly, simply because, in order to be useful, one has to employ surgery, which is really invasive. We'll want to try to get around that, but it seems quite likely that in the very early stages, the techniques we have for repairing things at the molecular and cellular level in situ will be insufficiently comprehensive, and so we will need to do the more sledgehammer approach of building a whole new organ and sticking it in.
Every time you are in a position where you're replacing an organ, you have the option, in principle, of repairing the organ, without replacing it. And repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells or whatever. That would be something one would expect to be able to apply to someone much closer to death's door and much more safely in general, and probably much more cheaply. One would expect that subsequent generations of these therapies would move in that direction.
Your foundation is working on an initiative requiring $50 million in funding—
Well, if we had $50 million per year in funding, we could go about three times faster than we are on $5 million per year.
And you're looking at a 2021 timeframe to start human trials?
That's approximate. Remember, because we accumulate in the body so many different types of damage, that means we have many different types of therapy to repair that damage. And of course, each of those types has to be developed independently. It's very much a divide and conquer therapy. The therapies interact with each other to some extent; the repair of one type of damage may slow down the creation of another type of damage, but still that's how it's going to be.
And some of these therapies are much easier to implement than others. The easier components of what we need to do are already in clinical trials—stem cell therapies especially, and immunotherapy against amyloid in the brain, for example. Even in phase III clinical trials in some cases. So when I talk about a timeframe like 2021, or early 20s shall we say, I'm really talking about the most difficult components.
What recent strides are you most excited about?
Looking back over the past couple of years, I'm particularly proud of the successes we've had in the very most difficult areas. If you go through the 7 components of SENS, there are two that have absolutely been stuck in a rut and have gotten nowhere for 15 to 20 years, and we basically fixed that in both cases. We published two years ago in Science magazine that essentially showed a way forward against the stiffening of the extracellular matrix, which is responsible for things like wrinkles and hypertension. And then a year ago, we published a real breakthrough paper with regard to placing copies of the mitochondria DNA in the nuclear DNA modified in such a way that they still work, which is an idea that had been around for 30 years; everyone had given up on it, some a long time ago, and we basically revived it.
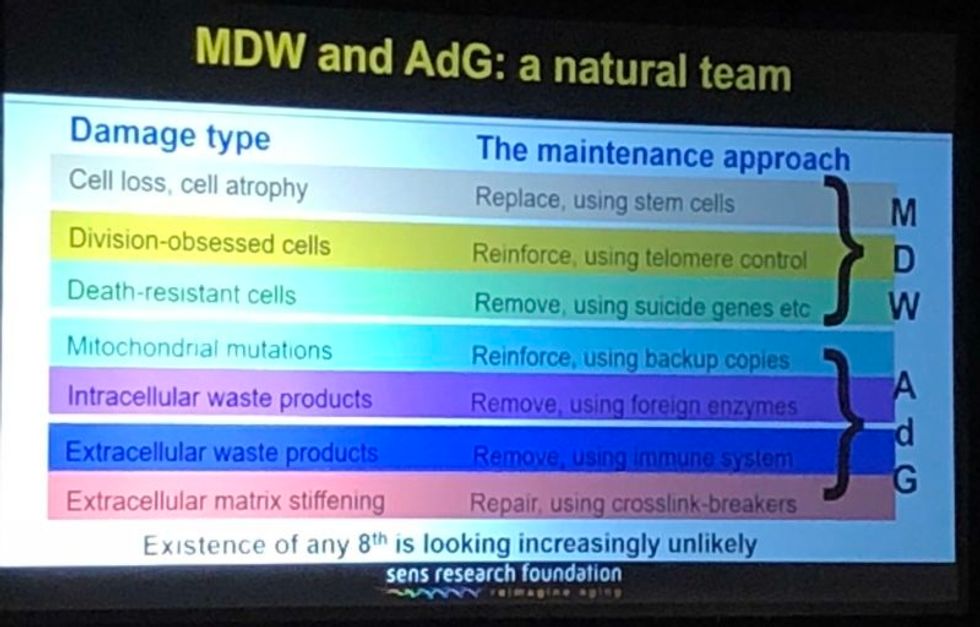
A slide presented by Aubrey de Grey, referencing his collaboration with Mike West at AgeX, showing the 7 types of damage that he believes must be repaired to end aging.
(Courtesy Kira Peikoff)
That's exciting. What do you think are the biggest barriers to defeating aging today: the technological challenges, the regulatory framework, the cost, or the cultural attitude of the "pro-aging" trance?
One can't really address those independently of each other. The technological side is one thing; it's hard, but we know where we're going, we've got a plan. The other ones are very intertwined with each other. A lot of people are inclined to say, the regulatory hurdle will be completely insurmountable, plus people don't recognize aging as a disease, so it's going to be a complete nonstarter. I think that's nonsense. And the reason is because the cultural attitudes toward all of this are going to be completely turned upside down before we have to worry about the regulatory hurdles. In other words, they're going to be turned upside down by sufficiently promising results in the lab, in mice. Once we get to be able to rejuvenate actually old mice really well so they live substantially longer than they otherwise would have done, in a healthy state, everyone's going to know about it and everyone's going to demand – it's not going to be possible to get re-elected unless you have a manifesto commitment to turn the FDA completely upside down and make sure this happens without any kind of regulatory obstacle.
I've been struggling away all these years trying to bring little bits of money in the door, and the reason I have is because of the skepticism as to regards whether this could actually work, combined with the pro-aging trance, which is a product of the skepticism – people not wanting to get their hopes up, so finding excuses about aging being a blessing in disguise, so they don't have to think about it. All of that will literally disintegrate pretty much overnight when we have the right kind of sufficiently impressive progress in the lab. Therefore, the availability of money will also [open up]. It's already cracking: we're already seeing the beginnings of the actual rejuvenation biotechnology industry that I've been talking about with a twinkle in my eye for some years.
"For humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years."
Why do you think the culture is starting to shift?
There's no one thing yet. There will be that tipping point I mentioned, perhaps five years from now when we get a real breakthrough, decisive results in mice that make it simply impossible to carry on being fatalistic about all this. Prior to that, what we're already seeing is the impact of sheer old-school repeat advertising—me going out there, banging away and saying the same fucking thing again and again, and nobody saying anything that persuasively knocks me down. … And it's also the fact that we are making incremental amounts of progress, not just ourselves, but the scientific community generally. It has become incrementally more plausible that what I say might be true.
I'm sure you hate getting the timeline question, but if we're five years away from this breakthrough in mice, it's hard to resist asking—how far is that in terms of a human cure?
When I give any kind of timeframes, the only real care I have to take is to emphasize the variance. In this case I think we have got a 50-50 chance of getting to that tipping point in mice within five years from now, certainly it could be 10 or 15 years if we get unlucky. Similarly, for humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years.
"I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction."
What would you tell skeptical people are the biggest benefits of a very long-lived population?
Any question about the longevity of people is the wrong question. Because the longevity that people fixate about so much will only ever occur as a side effect of health. However long ago you were born or however recently, if you're sick, you're likely to die fairly soon unless we can stop you being sick. Whereas if you're healthy, you're not. So if we do as well as we think we can do in terms of keeping people healthy and youthful however long ago they were born, then the side effect in terms of longevity and life expectancy is likely to be very large. But it's still a side effect, so the way that people actually ought to be—in fact have a requirement to be—thinking, is about whether they want people to be healthy.
Now I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction, they like to sweep it under the carpet and say, oh yeah, aging is totally a good thing.
People will never actually admit to the fact that what they are fundamentally saying is medicine for the elderly, if it actually works, would be bad, but still that is what they are saying.
Shifting gears a bit, I'm curious to find out which other radical visionaries in science and tech today you most admire?
Fair question. One is Mike West. I have the great privilege that I now work for him part-time with Age X. I have looked up to him very much for the past ten years, because what he did over the past 20 years starting with Geron is unimaginable today. He was working in an environment where I would not have dreamt of the possibility of getting any private money, any actual investment, in something that far out, that far ahead of its time, and he did it, again and again. It's insane what he managed to do.
What about someone like Elon Musk?
Sure, he's another one. He is totally impervious to the caution and criticism and conservatism that pervades humanity, and he's getting on making these bloody self-driving cars, space tourism, and so on, making them happen. He's thinking just the way I'm thinking really.
"You can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time."
You famously said ten years ago that you think the first person to live to 1000 is already alive. Do you think that's still the case?
Definitely, yeah. I can't see how it could not be. Again, it's a probabilistic thing. I said there's at least a 10 percent chance that we won't get to what I call Longevity Escape Velocity for 100 years and if that's true, then the statement about 1000 years being alive already is not going to be the case. But for sure, I believe that the beneficiaries of what we may as well call SENS 1.0, the point where we get to LEV, those people are exceptionally unlikely ever to suffer from any kind of ill health correlated with their age. Because we will never fall below Longevity Escape Velocity once we attain it.
Could someone who was just born today expect—
I would say people in middle age now have a fair chance. Remember – a 50/50 chance of getting to LEV within 20 years, and when you get there, you don't just stay at biologically 70 or 80, you are rejuvenated back to biologically 30 or 40 and you stay there, so your risk of death each year is not related to how long ago you were born, it's the same as a young adult. Today, that's less than 1 in 1000 per year, and that number is going to go down as we get self-driving cars and all that, so actually 1000 is a very conservative number.
So you would be able to choose what age you wanted to go back to?
Oh sure, of course, it's just like a car. What you're doing is you're repairing damage, and the damage is still being created by the body's metabolism, so you can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time.
What would be your perfect age?
I have no idea. That's something I don't have an opinion about, because I could change it whenever I like.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

