COVID Variants Are Like “a Thief Changing Clothes” – and Our Camera System Barely Exists

Being able to track variants of concern in real time is crucial to our ability to stay ahead of the virus.
Whether it's "natural selection" as Darwin called it, or it's "mutating" as the X-Men called it, living organisms change over time, developing thumbs or more efficient protein spikes, depending on the organism and the demands of its environment. The coronavirus that causes COVID-19, SARS-CoV-2, is not an exception, and now, after the virus has infected millions of people around the globe for more than a year, scientists are beginning to see those changes.
The notorious variants that have popped up include B.1.1.7, sometimes called the UK variant, as well as P.1 and B.1.351, which seem to have emerged in Brazil and South Africa respectively. As vaccinations are picking up pace, officials are warning that now
is not the time to become complacent or relax restrictions because the variants aren't well understood.
Some appear to be more transmissible, and deadlier, while others can evade the immune system's defenses better than earlier versions of the virus, potentially undermining the effectiveness of vaccines to some degree. Genomic surveillance, the process of sequencing the genetic code of the virus widely to observe changes and patterns, is a critical way that scientists can keep track of its evolution and work to understand how the variants might affect humans.
"It's like a thief changing clothes"
It's important to note that viruses mutate all the time. If there were funding and personnel to sequence the genome of every sample of the virus, scientists would see thousands of mutations. Not every variant deserves our attention. The vast majority of mutations are not important at all, but recognizing those that are is a crucial tool in getting and staying ahead of the virus. The work of sequencing, analyzing, observing patterns, and using public health tools as necessary is complicated and confusing to those without years of specialized training.
Jeremy Kamil, associate professor of microbiology and immunology at LSU Health Shreveport, in Louisiana, says that the variants developing are like a thief changing clothes. The thief goes in your house, steals your stuff, then leaves and puts on a different shirt and a wig, in the hopes you won't recognize them. Genomic surveillance catches the "thief" even in those different clothes.
One of the tricky things about variants is recognizing the point at which they move from interesting, to concerning at a local level, to dangerous in a larger context.
Understanding variants, both the uninteresting ones and the potentially concerning ones, gives public health officials and researchers at different levels a useful set of tools. Locally, knowing which variants are circulating in the community helps leaders know whether mask mandates and similar measures should be implemented or discontinued, or whether businesses and schools can open relatively safely.
There's more to it than observing new variants
Analysis is complex, particularly when it comes to understanding which variants are of concern. "So the question is always if a mutation becomes common, is that a random occurrence?" says Phoebe Lostroh, associate professor of molecular biology at Colorado College. "Or is the variant the result of some kind of selection because the mutation changes some property about the virus that makes it reproduce more quickly than variants of the virus that don't have that mutation? For a virus, [mutations can affect outcomes like] how much it replicates inside a person's body, how much somebody breathes it out, whether the particles that somebody might breathe in get smaller and can lead to greater transmission."
Along with all of those factors, accurate and useful genomic surveillance requires an understanding of where variants are occurring, how they are related, and an examination of why they might be prevalent.
For example, if a potentially worrisome variant appears in a community and begins to spread very quickly, it's not time to raise a public health alarm until several important questions have been answered, such as whether the variant is spreading due to specific events, or if it's happening because the mutation has allowed the virus to infect people more efficiently. Kamil offered a hypothetical scenario to explain: Imagine that a member of a community became infected and the virus mutated. That person went to church and three more people were infected, but one of them went to a karaoke bar and while singing infected 100 other people. Examining the conditions under which the virus has spread is, therefore, an essential part of untangling whether a mutation itself made the virus more transmissible or if an infected person's behaviors contributed to a local outbreak.
One of the tricky things about variants is recognizing the point at which they move from interesting, to concerning at a local level, to dangerous in a larger context. Genomic sequencing can help with that, but only when it's coordinated. When the same mutation occurs frequently, but is localized to one region, it's a concern, but when the same mutation happens in different places at the same time, it's much more likely that the "virus is learning that's a good mutation," explains Kamil.
The process is called convergent evolution, and it was a fascinating topic long before COVID. Just as your heritage can be traced through DNA, so can that of viruses, and when separate lineages develop similar traits it's almost like scientists can see evolution happening in real time. A mutation to SARS-CoV-2 that happens in more than one place at once is a mutation that makes it easier in some way for the virus to survive and that is when it may become alarming. The widespread, documented variants P.1 and B.1.351 are examples of convergence because they share some of the same virulent mutations despite having developed thousands of miles apart.
However, even variants that are emerging in different places at the same time don't present the kind of threat SARS-CoV-2 did in 2019. "This is nature," says Kamil. "It just means that this virus will not easily be driven to extinction or complete elimination by vaccines." Although a person who has already had COVID-19 can be reinfected with a variant, "it is almost always much milder disease" than the original infection, Kamil adds. Rather than causing full-fledged disease, variants have the potiental to "penetrate herd immunity, spreading relatively quietly among people who have developed natural immunity or been vaccinated, until the virus finds someone who has no immunity yet, and that person would be at risk of hospitalization-grade severe disease or death."
Surveillance and predictions
According to Lostroh, genomic surveillance can help scientists predict what's going to happen. "With the British strain, for instance, that's more transmissible, you can measure how fast it's doubling in the population and you can sort of tell whether we should take more measures against this mutation. Should we shut things down a little longer because that mutation is present in the population? That could be really useful if you did enough sampling in the population that you knew where it was," says Lostroh. If, for example, the more transmissible strain was present in 50 percent of cases, but in another county or state it was barely present, it would allow for rolling lockdowns instead of sweeping measures.
Variants are also extremely important when it comes to the development, manufacture, and distribution of vaccines. "You're also looking at medical countermeasures, such as whether your vaccine is still effective, or if your antiviral needs to be updated," says Lane Warmbrod, a senior analyst and research associate at Johns Hopkins Center for Health Security.
Properly funded and extensive genomic surveillance could eventually help control endemic diseases, too, like the seasonal flu, or other common respiratory infections. Kamil says he envisions a future in which genomic surveillance allows for prediction of sickness just as the weather is predicted today. "It's a 51 for infection today at the San Francisco Airport. There's been detection of some respiratory viruses," he says, offering an example. He says that if you're a vulnerable person, if you're immune-suppressed for some reason, you may want to wear a mask based on the sickness report.
The U.S. has the ability, but lacks standards
The benefits of widespread genomic surveillance are clear, and the United States certainly has the necessary technology, equipment, and personnel to carry it out. But, it's not happening at the speed and extent it needs to for the country to gain the benefits.
"The numbers are improving," said Kamil. "We're probably still at less than half a percent of all the samples that have been taken have been sequenced since the beginning of the pandemic."
Although there's no consensus on how many sequences is ideal for a robust surveillance program, modeling performed by the company Illumina suggests about 5 percent of positive tests should be sequenced. The reasons the U.S. has lagged in implementing a sequencing program are complex and varied, but solvable.
Perhaps the most important element that is currently missing is leadership. In order to conduct an effective genomic surveillance program, there need to be standards. The Johns Hopkins Center for Health Security recently published a paper with recommendations as to what kinds of elements need to be standardized in order to make the best use of sequencing technology and analysis.
"Along with which bioinformatic pipelines you're going to use to do the analyses, which sequencing strategy protocol are you going to use, what's your sampling strategy going to be, how is the data is going to be reported, what data gets reported," says Warmbrod. Currently, there's no guidance from the CDC on any of those things. So, while scientists can collect and report information, they may be collecting and reporting different information that isn't comparable, making it less useful for public health measures and vaccine updates.
Globally, one of the most important tools in making the information from genomic surveillance useful is GISAID, a platform designed for scientists to share -- and, importantly, to be credited for -- their data regarding genetic sequences of influenza. Originally, it was launched as a database of bird flu sequences, but has evolved to become an essential tool used by the WHO to make flu vaccine virus recommendations each year. Scientists who share their credentials have free access to the database, and anyone who uses information from the database must credit the scientist who uploaded that information.
Safety, logistics, and funding matter
Scientists at university labs and other small organizations have been uploading sequences to GISAID almost from the beginning of the pandemic, but their funding is generally limited, and there are no standards regarding information collection or reporting. Private, for-profit labs haven't had motivation to set up sequencing programs, although many of them have the logistical capabilities and funding to do so. Public health departments are understaffed, underfunded, and overwhelmed.
University labs may also be limited by safety concerns. The SARS-CoV-2 virus is dangerous, and there's a question of how samples should be transported to labs for sequencing.
Larger, for-profit organizations often have the tools and distribution capabilities to safely collect and sequence samples, but there hasn't been a profit motive. Genomic sequencing is less expensive now than ever before, but even at $100 per sample, the cost adds up -- not to mention the cost of employing a scientist with the proper credentials to analyze the sequence.
The path forward
The recently passed COVID-19 relief bill does have some funding to address genomic sequencing. Specifically, the American Rescue Plan Act includes $1.75 billion in funding for the Centers for Disease Control and Prevention's Advanced Molecular Detection (AMD) program. In an interview last month, CDC Director Rochelle Walensky said that the additional funding will be "a dial. And we're going to need to dial it up." AMD has already announced a collaboration called the Sequencing for Public Health Emergency Response, Epidemiology, and Surveillance (SPHERES) Initiative that will bring together scientists from public health, academic, clinical, and non-profit laboratories across the country with the goal of accelerating sequencing.
Such a collaboration is a step toward following the recommendations in the paper Warmbrod coauthored. Building capacity now, creating a network of labs, and standardizing procedures will mean improved health in the future. "I want to be optimistic," she says. "The good news is there are a lot of passionate, smart, capable people who are continuing to work with government and work with different stakeholders." She cautions, however, that without a national strategy we won't succeed.
"If we maximize the potential and create that framework now, we can also use it for endemic diseases," she says. "It's a very helpful system for more than COVID if we're smart in how we plan it."
The U.S. must fund more biotech innovation – or other countries will catch up faster than you think
In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

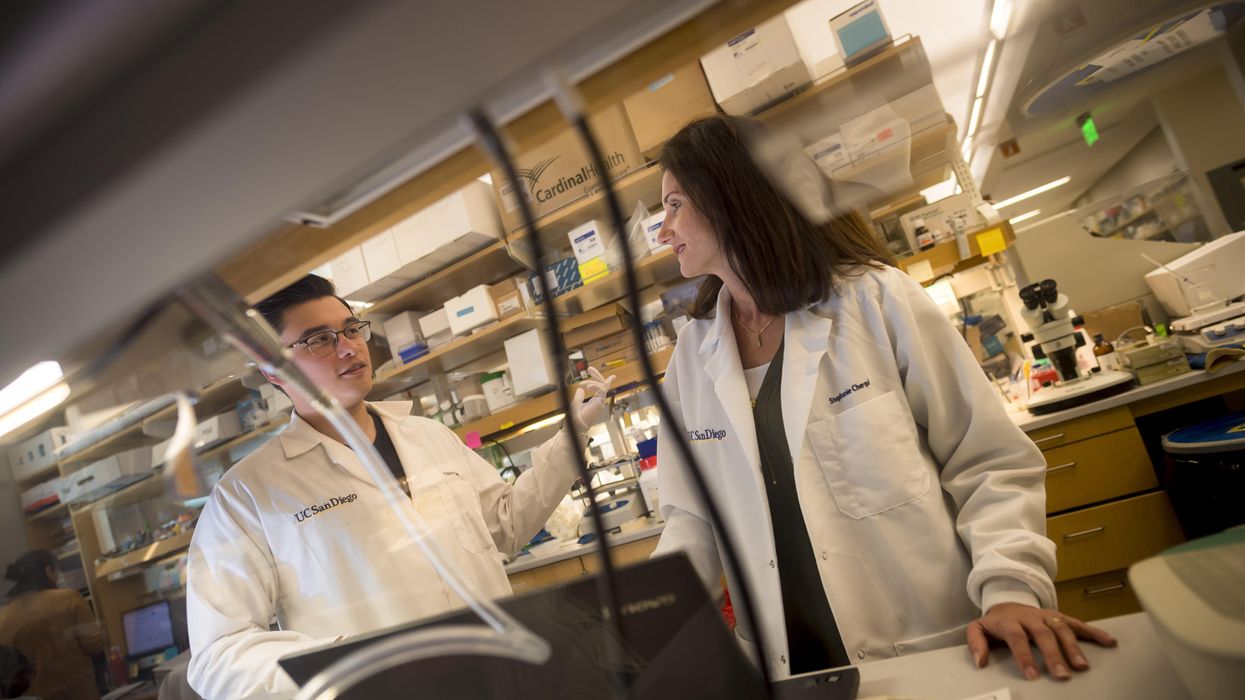
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.