Why Don’t We Have Artificial Wombs for Premature Infants?
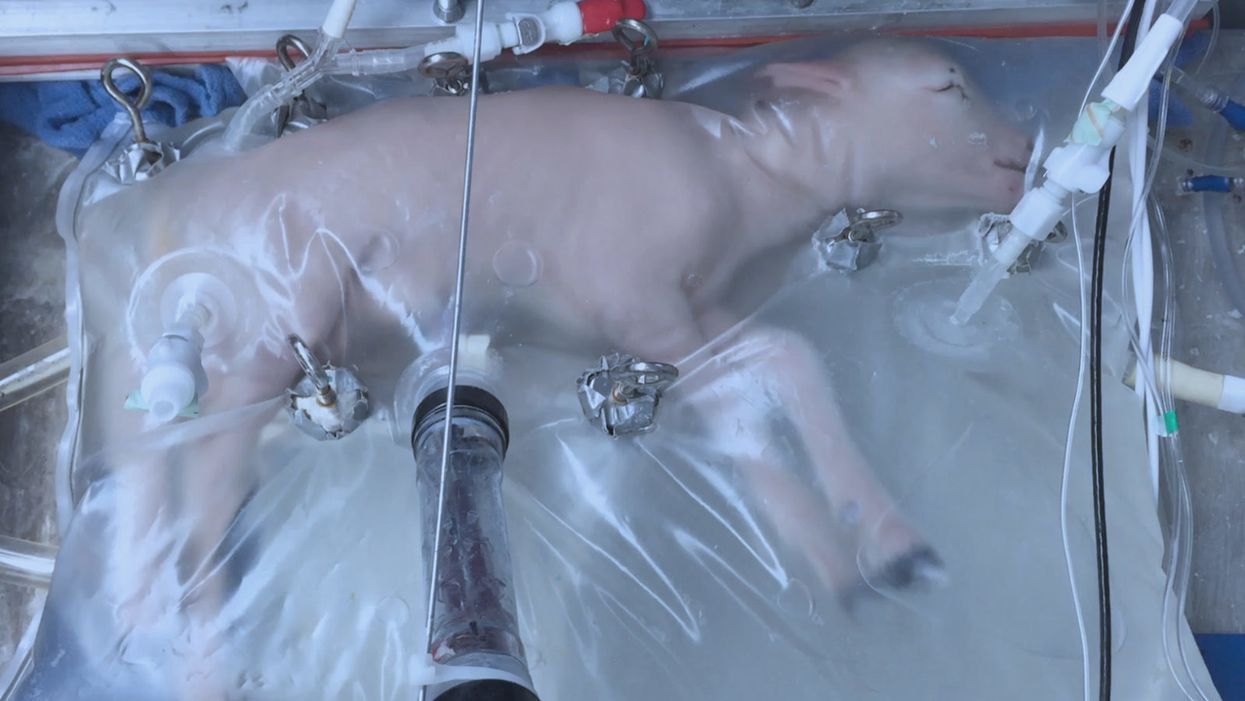
A lamb which was prematurely born at the equivalent of 23 weeks' human gestation, after 28 days of support from an artificial womb.
Ectogenesis, the development of a baby outside of the mother's body, is a concept that dates back to 1923. That year, British biochemist-geneticist J.B.S. Haldane gave a lecture to the "Heretics Society" of the University of Cambridge in which he predicted the invention of an artificial womb by 1960, leading to 70 percent of newborns being born that way by the 2070s. In reality, that's about when an artificial womb could be clinically operational, but trends in science and medicine suggest that such technology would come in increments, each fraught with ethical and social challenges.
An extra-uterine support device could be ready for clinical trials in humans in the next two to four years, with hopes that it could improve survival of very premature infants.
Currently, one major step is in the works, a system called an extra-uterine support device (EUSD) –or sometimes Ex-Vivo uterine Environment (EVE)– which researchers at the Children's Hospital of Philadelphia have been using to support fetal lambs outside the mother. It also has been called an artificial placenta, because it supplies nutrient- and oxygen-rich blood to the developing lambs via the umbilical vein and receives blood full of waste products through the umbilical arteries. It does not do everything that a natural placenta does, yet it does do some things that a placenta doesn't do. It breathes for the fetus like the mother's lungs, and encloses the fetus in sterile fluid, just like the amniotic sac. It represents a solution to one set of technical challenges in the path to an artificial womb, namely how to keep oxygen flowing into a fetus and carbon dioxide flowing out when the fetal lungs are not ready to function.
Capable of supporting fetal lambs physiologically equivalent to a human fetus at 23 weeks' gestation or earlier, the EUSD could be ready for clinical trials in humans in the next two to four years, with hopes that it could improve survival of very premature infants. Existing medical technology can keep human infants alive when born in this 23-week range, or even slightly less —the record is just below 22 weeks. But survival is low, because most of the treatment is directed at the lungs, the last major body system to mature to a functional status. This leads to complications not only in babies born before 24 weeks' gestation, but also in a fairly large number of births up to 28 weeks' gestation.
So, the EUSD is basically an advanced neonatal life support machine that beckons to square off the survival curve for infants born up to the 28th week. That is no doubt a good thing, but given the political prominence of reproductive issues, might any societal obstacles be looming?
"While some may argue that the EUSD system will shift the definition of viability to a point prior to the maturation of the fetus' lungs, ethical and legal frameworks must still recognize the mother's privacy rights as paramount."
Health care attorney and clinical ethicist David N. Hoffman points out that even though the EUSD may shift the concept of fetal viability away from the maturity of developing lungs, it would not change the current relationship of the fetus to the mother during pregnancy.
"Our social and legal frameworks, including Roe v. Wade, invite the view of the embryo-fetus as resembling a parasite. Not in a negative sense, but functionally, since it obtains its life support from the mother, while she does not need the fetus for her own physical health," notes Hoffman, who holds faculty appointments at Columbia University, and at the Benjamin N. Cardozo School of Law and the Albert Einstein College of Medicine, of Yeshiva University. "In contrast, our ethical conception of the relationship is grounded in the nurturing responsibility of parenthood. We prioritize the welfare of both mother and fetus ethically, but we lean toward the side of the mother's legal rights, regarding her health throughout pregnancy, and her right to control her womb for most of pregnancy. While some may argue that the EUSD system will shift the definition of viability to a point prior to the maturation of the fetus' lungs, ethical and legal frameworks must still recognize the mother's privacy rights as paramount, on the basis of traditional notions of personhood and parenthood."
Outside of legal frameworks, religion, of course, is a major factor in how society reacts to new reproductive technologies, and an artificial womb would trigger a spectrum of responses.
"Significant numbers of conservative Christians may oppose an artificial womb in fear that it might harm the central role of marriage in Christianity."
Speaking from the perspective of Lutheran scholarship, Dr. Daniel Deen, Assistant Professor of Philosophy at Concordia University in Irvine, Calif., does not foresee any objections to the EUSD, either theologically, or generally from Lutherans (who tend to be conservative on reproductive issues), since the EUSD is basically an improvement on current management of prematurity. But things would change with the advent of a full-blown artificial womb.
"Significant numbers of conservative Christians may oppose an artificial womb in fear that it might harm the central role of marriage in Christianity," says Deen, who specializes in the philosophy of science. "They may see the artificial womb as a catalyst for strengthening the mechanistic view of reproduction that dominates the thinking of secular society, and of other religious groups, including more liberal Christians."
Judaism, however, appears to be more receptive, even during the research phases.
"Even if researchers strive for a next-generation EUSD aimed at supporting a fetus several weeks earlier than possible with the current system, it still keeps the fetus inside the mother well beyond the 40-day threshold, so there likely are no concerns in terms of Jewish law," says Kalman Laufer, a rabbinical student and executive director of the Medical Ethics Society at Yeshiva University. Referring to a concept from the Babylonian Talmud that an embryo is "like water" until 40 days into pregnancy, at which time it receives a kind of almost-human status warranting protection, Laufer cautions that he's speaking about artificial wombs developed for the sake of rescuing very premature infants. At the same time though, he expects that artificial womb research will eventually trigger a series of complex, legalistic opinions from Jewish scholars, as biotechnology moves further toward supporting fetal growth entirely outside a woman's body.
"Since [the EUSD] gives some justification to end abortion, by transferring fetuses from mother to machine, conservatives will probably rally around it."
While the technology treads into uncomfortable territory for social conservatives at first glance, it's possible that the prospect of taking the abortion debate in a whole new direction could engender support for the artificial womb. "Since [the EUSD] gives some justification to end abortion, by transferring fetuses from mother to machine, conservatives will probably rally around it," says Zoltan Istvan, a transhumanist politician and journalist who ran for U.S. president in 2016. To some extent, Deen agrees with Istvan, provided we get to a point when the artificial womb is already a reality.
"The world has a way of moving forward despite the fear of its inhabitants," Deen notes. "If the technology gets developed, I could not see any Christians, liberal or conservative, arguing that people seeking abortion ought not opt for a 'transfer' versus an abortive procedure."
So then how realistic is a full-blown artificial womb? The researchers at the Children's Hospital of Philadelphia have noted various technical difficulties that would come up in any attempt to connect a very young fetus to the EUSD and maintain life. One issue is the small umbilical cord blood vessels that must be connected to the EUSD as fetuses of decreasing gestational age are moved outside the mother. Current procedures might be barely adequate for integrating a human fetus into the device in the 18 -21 week range, but going to lower gestational ages would require new technology and different strategies. It also would require numerous other factors to cover for fetal body systems that mature ahead of the lungs and that the current EUSD system is not designed to replace. However, biotechnology and tissue engineering strategies on the horizon could be added to later EUSDs. To address the blood vessel size issue, artificial womb research could benefit by drawing on experts in microfluidics, the field concerned with manipulation of tiny amounts of fluid through very small spaces, and which is ushering in biotech innovations like the "lab on a chip".
"The artificial womb might put fathers on equal footing with mothers, since any embryo could potentially achieve personhood without ever seeing the inside of a woman's uterus."
If the technical challenges to an artificial womb are indeed overcome, reproductive policy debates could be turned on their side.
"Evolution of the EUSD into a full-blown artificial external uterus has ramifications for any reproductive rights issues where policy currently assumes that a mother is needed for a fertilized egg to become a person," says Hoffman, the ethicist and legal scholar. "If we consider debates over whether to keep cryopreserved human embryos in storage, destroy them, or utilize them for embryonic stem cell research or therapies, the artificial womb might put fathers on equal footing with mothers, since any embryo could potentially achieve personhood without ever seeing the inside of a woman's uterus."
Such a scenario, of course, depends on today's developments not being curtailed or sidetracked by societal objections before full-blown ectogenesis is feasible. But if this does ever become a reality, the history of other biotechnologies suggests that some segment of society will embrace the new innovation and never look back.
Nobel Prize goes to technology for mRNA vaccines
Katalin Karikó, pictured, and Drew Weissman won the Nobel Prize for advances in mRNA research that led to the first Covid vaccines.
When Drew Weissman received a call from Katalin Karikó in the early morning hours this past Monday, he assumed his longtime research partner was calling to share a nascent, nagging idea. Weissman, a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania, and Karikó, a professor at Szeged University and an adjunct professor at UPenn, both struggle with sleep disturbances. Thus, middle-of-the-night discourses between the two, often over email, has been a staple of their friendship. But this time, Karikó had something more pressing and exciting to share: They had won the 2023 Nobel Prize in Physiology or Medicine.
The work for which they garnered the illustrious award and its accompanying $1,000,000 cash windfall was completed about two decades ago, wrought through long hours in the lab over many arduous years. But humanity collectively benefited from its life-saving outcome three years ago, when both Moderna and Pfizer/BioNTech’s mRNA vaccines against COVID were found to be safe and highly effective at preventing severe disease. Billions of doses have since been given out to protect humans from the upstart viral scourge.
“I thought of going somewhere else, or doing something else,” said Katalin Karikó. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
Unlocking the power of mRNA
Weissman and Karikó unlocked mRNA vaccines for the world back in the early 2000s when they made a key breakthrough. Messenger RNA molecules are essentially instructions for cells’ ribosomes to make specific proteins, so in the 1980s and 1990s, researchers started wondering if sneaking mRNA into the body could trigger cells to manufacture antibodies, enzymes, or growth agents for protecting against infection, treating disease, or repairing tissues. But there was a big problem: injecting this synthetic mRNA triggered a dangerous, inflammatory immune response resulting in the mRNA’s destruction.
While most other researchers chose not to tackle this perplexing problem to instead pursue more lucrative and publishable exploits, Karikó stuck with it. The choice sent her academic career into depressing doldrums. Nobody would fund her work, publications dried up, and after six years as an assistant professor at the University of Pennsylvania, Karikó got demoted. She was going backward.
“I thought of going somewhere else, or doing something else,” Karikó told Stat in 2020. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
A tale of tenacity
Collaborating with Drew Weissman, a new professor at the University of Pennsylvania, in the late 1990s helped provide Karikó with the tenacity to continue. Weissman nurtured a goal of developing a vaccine against HIV-1, and saw mRNA as a potential way to do it.
“For the 20 years that we’ve worked together before anybody knew what RNA is, or cared, it was the two of us literally side by side at a bench working together,” Weissman said in an interview with Adam Smith of the Nobel Foundation.
In 2005, the duo made their 2023 Nobel Prize-winning breakthrough, detailing it in a relatively small journal, Immunity. (Their paper was rejected by larger journals, including Science and Nature.) They figured out that chemically modifying the nucleoside bases that make up mRNA allowed the molecule to slip past the body’s immune defenses. Karikó and Weissman followed up that finding by creating mRNA that’s more efficiently translated within cells, greatly boosting protein production. In 2020, scientists at Moderna and BioNTech (where Karikó worked from 2013 to 2022) rushed to craft vaccines against COVID, putting their methods to life-saving use.
The future of vaccines
Buoyed by the resounding success of mRNA vaccines, scientists are now hurriedly researching ways to use mRNA medicine against other infectious diseases, cancer, and genetic disorders. The now ubiquitous efforts stand in stark contrast to Karikó and Weissman’s previously unheralded struggles years ago as they doggedly worked to realize a shared dream that so many others shied away from. Katalin Karikó and Drew Weissman were brave enough to walk a scientific path that very well could have ended in a dead end, and for that, they absolutely deserve their 2023 Nobel Prize.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.
Scientists turn pee into power in Uganda
With conventional fuel cells as their model, researchers learned to use similar chemical reactions to make a fuel from microbes in pee.
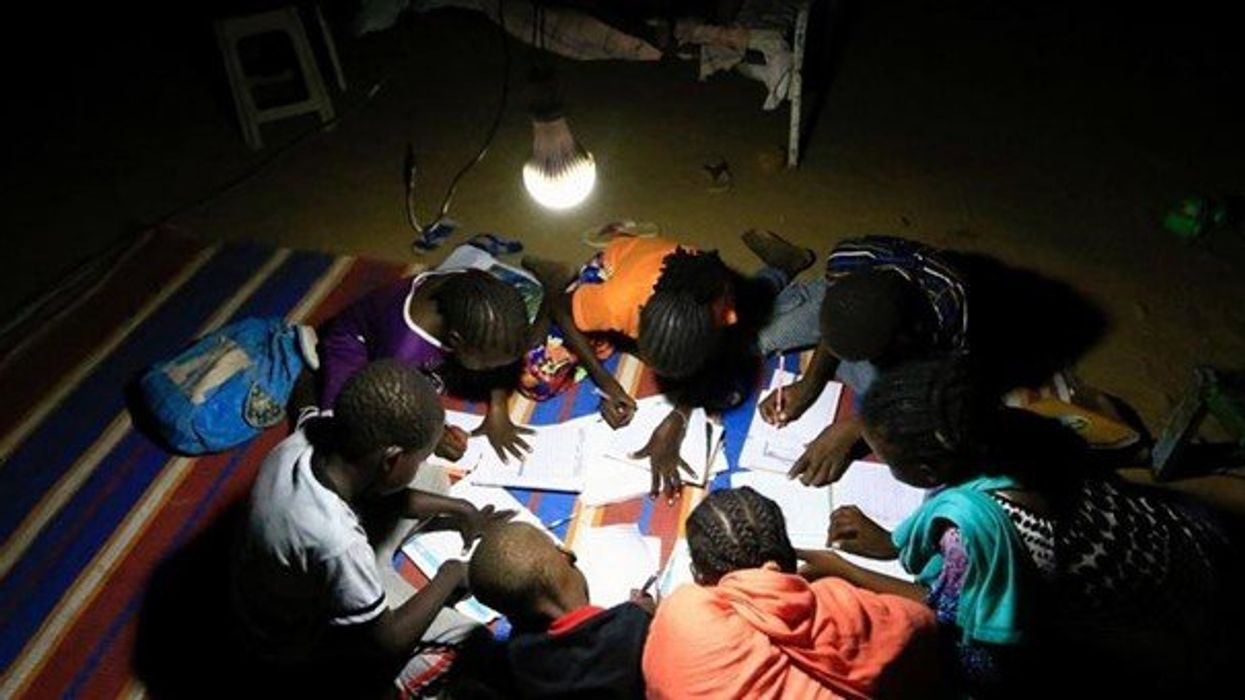
At the edge of a dirt road flanked by trees and green mountains outside the town of Kisoro, Uganda, sits the concrete building that houses Sesame Girls School, where girls aged 11 to 19 can live, learn and, at least for a while, safely use a toilet. In many developing regions, toileting at night is especially dangerous for children. Without electrical power for lighting, kids may fall into the deep pits of the latrines through broken or unsteady floorboards. Girls are sometimes assaulted by men who hide in the dark.
For the Sesame School girls, though, bright LED lights, connected to tiny gadgets, chased the fears away. They got to use new, clean toilets lit by the power of their own pee. Some girls even used the light provided by the latrines to study.
Urine, whether animal or human, is more than waste. It’s a cheap and abundant resource. Each day across the globe, 8.1 billion humans make 4 billion gallons of pee. Cows, pigs, deer, elephants and other animals add more. By spending money to get rid of it, we waste a renewable resource that can serve more than one purpose. Microorganisms that feed on nutrients in urine can be used in a microbial fuel cell that generates electricity – or "pee power," as the Sesame girls called it.
Plus, urine contains water, phosphorus, potassium and nitrogen, the key ingredients plants need to grow and survive. Human urine could replace about 25 percent of current nitrogen and phosphorous fertilizers worldwide and could save water for gardens and crops. The average U.S. resident flushes a toilet bowl containing only pee and paper about six to seven times a day, which adds up to about 3,500 gallons of water down per year. Plus cows in the U.S. produce 231 gallons of the stuff each year.
Pee power
A conventional fuel cell uses chemical reactions to produce energy, as electrons move from one electrode to another to power a lightbulb or phone. Ioannis Ieropoulos, a professor and chair of Environmental Engineering at the University of Southampton in England, realized the same type of reaction could be used to make a fuel from microbes in pee.
Bacterial species like Shewanella oneidensis and Pseudomonas aeruginosa can consume carbon and other nutrients in urine and pop out electrons as a result of their digestion. In a microbial fuel cell, one electrode is covered in microbes, immersed in urine and kept away from oxygen. Another electrode is in contact with oxygen. When the microbes feed on nutrients, they produce the electrons that flow through the circuit from one electrod to another to combine with oxygen on the other side. As long as the microbes have fresh pee to chomp on, electrons keep flowing. And after the microbes are done with the pee, it can be used as fertilizer.
These microbes are easily found in wastewater treatment plants, ponds, lakes, rivers or soil. Keeping them alive is the easy part, says Ieropoulos. Once the cells start producing stable power, his group sequences the microbes and keeps using them.
Like many promising technologies, scaling these devices for mass consumption won’t be easy, says Kevin Orner, a civil engineering professor at West Virginia University. But it’s moving in the right direction. Ieropoulos’s device has shrunk from the size of about three packs of cards to a large glue stick. It looks and works much like a AAA battery and produce about the same power. By itself, the device can barely power a light bulb, but when stacked together, they can do much more—just like photovoltaic cells in solar panels. His lab has produced 1760 fuel cells stacked together, and with manufacturing support, there’s no theoretical ceiling, he says.
Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofit into urban wastewater utilities.
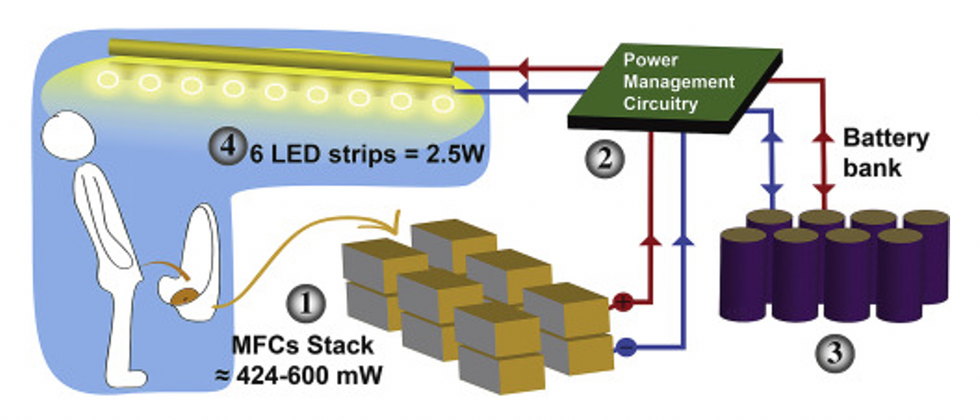
This image shows how the pee-powered system works. Pee feeds bacteria in the stack of fuel cells (1), which give off electrons (2) stored in parallel cylindrical cells (3). These cells are connected to a voltage regulator (4), which smooths out the electrical signal to ensure consistent power to the LED strips lighting the toilet.
Courtesy Ioannis Ieropoulos
Key to the long-term success of any urine reclamation effort, says Orner, is avoiding what he calls “parachute engineering”—when well-meaning scientists solve a problem with novel tech and then abandon it. “The way around that is to have either the need come from the community or to have an organization in a community that is committed to seeing a project operate and maintained,” he says.
Success with urine reclamation also depends on the economy. “If energy prices are low, it may not make sense to recover energy,” says Orner. “But right now, fertilizer prices worldwide are generally pretty high, so it may make sense to recover fertilizer and nutrients.” There are obstacles, too, such as few incentives for builders to incorporate urine recycling into new construction. And any hiccups like leaks or waste seepage will cost builders money and reputation. Right now, Orner says, the risks are just too high.
Despite the challenges, Ieropoulos envisions a future in which urine is passed through microbial fuel cells at wastewater treatment plants, retrofitted septic tanks, and building basements, and is then delivered to businesses to use as agricultural fertilizers. Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofitted into urban wastewater utilities where they can make electricity from the effluent. And unlike solar cells, which are a common target of theft in some areas, nobody wants to steal a bunch of pee.
When Ieropoulos’s team returned to wrap up their pilot project 18 months later, the school’s director begged them to leave the fuel cells in place—because they made a major difference in students’ lives. “We replaced it with a substantial photovoltaic panel,” says Ieropoulos, They couldn’t leave the units forever, he explained, because of intellectual property reasons—their funders worried about theft of both the technology and the idea. But the photovoltaic replacement could be stolen, too, leaving the girls in the dark.
The story repeated itself at another school, in Nairobi, Kenya, as well as in an informal settlement in Durban, South Africa. Each time, Ieropoulos vowed to return. Though the pandemic has delayed his promise, he is resolute about continuing his work—it is a moral and legal obligation. “We've made a commitment to ourselves and to the pupils,” he says. “That's why we need to go back.”
Urine as fertilizer
Modern day industrial systems perpetuate the broken cycle of nutrients. When plants grow, they use up nutrients the soil. We eat the plans and excrete some of the nutrients we pass them into rivers and oceans. As a result, farmers must keep fertilizing the fields while our waste keeps fertilizing the waterways, where the algae, overfertilized with nitrogen, phosphorous and other nutrients grows out of control, sucking up oxygen that other marine species need to live. Few global communities remain untouched by the related challenges this broken chain create: insufficient clean water, food, and energy, and too much human and animal waste.
The Rich Earth Institute in Vermont runs a community-wide urine nutrient recovery program, which collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms.
One solution to this broken cycle is reclaiming urine and returning it back to the land. The Rich Earth Institute in Vermont is one of several organizations around the world working to divert and save urine for agricultural use. “The urine produced by an adult in one day contains enough fertilizer to grow all the wheat in one loaf of bread,” states their website.
Notably, while urine is not entirely sterile, it tends to harbor fewer pathogens than feces. That’s largely because urine has less organic matter and therefore less food for pathogens to feed on, but also because the urinary tract and the bladder have built-in antimicrobial defenses that kill many germs. In fact, the Rich Earth Institute says it’s safe to put your own urine onto crops grown for home consumption. Nonetheless, you’ll want to dilute it first because pee usually has too much nitrogen and can cause “fertilizer burn” if applied straight without dilution. Other projects to turn urine into fertilizer are in progress in Niger, South Africa, Kenya, Ethiopia, Sweden, Switzerland, The Netherlands, Australia, and France.
Eleven years ago, the Institute started a program that collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms. By 2021, the program included 180 donors producing over 12,000 gallons of urine each year. This urine is helping to fertilize hay fields at four partnering farms. Orner, the West Virginia professor, sees it as a success story. “They've shown how you can do this right--implementing it at a community level scale."