Drugs That Could Slow Aging May Hold Promise for Protecting the Elderly from COVID-19

Two recent human studies indicated that rapalogues increased resistance to the flu and decreased the severity of respiratory tract infections in older adults.
Although recent data has shown the coronavirus poses a greater risk to young people than previously understood, the ensuing COVID-19 disease is clearly far more dangerous for older people than it is for the young.
If we want to lower the COVID-19 fatality rate, we must also make fortifying our most vulnerable hosts a central part of our approach.
While our older adults have accrued tremendous knowledge, wisdom, and perspective over the years, their bodies have over time become less able to fight off viruses and other insults. The shorthand name for this increased susceptibility is aging.
We may have different names for the diseases which disproportionately kill us -- cancer, heart disease, and dementia among them – but what is really killing us is age. The older we are, the greater the chance we'll die from one or another of these afflictions. Eliminate any one completely - including cancer - and we won't on average live that much longer. But if we slow aging on a cellular level, we can counter all of these diseases at once, including COVID-19.
Every army needs both offensive and defensive capabilities. In our war against COVID-19, our offense strategy is to fight the virus directly. But strengthening our defense requires making us all more resistant to its danger. That's why everyone needs to be eating well, exercising, and remaining socially connected. But if we want to lower the COVID-19 fatality rate, we must also make fortifying our most vulnerable hosts a central part of our approach. That's where our new fight against this disease and the emerging science of aging intersect.
Once the domain of charlatans and delusionists, the millennia-old fantasy of extending our healthy lifespans has over the past century become real. But while the big jump in longevity around the world over the past hundred years or so is mostly attributable to advances in sanitation, nutrition, basic healthcare, and worker safety, advances over the next hundred will come from our increasing ability to hack the biology of aging itself.
A few decades ago, scientists began recognizing that some laboratory animals on calorie-restricted diets tended to live healthier, longer lives. Through careful experiments derived from these types of insights, scientists began identifying specific genetic, epigenetic, and metabolic pathways that influence how we age. A range of studies have recently suggested that systemic knobs might metaphorically be turned to slow the cellular aging process, making us better able to fight off diseases and viral attacks.
Among the most promising of these systemic interventions is a drug called metformin, which targets many of the hallmarks of aging and extends health span and lifespan in animals. Metformin has been around since the Middle Ages and has been used in Europe for over 60 years to treat diabetes. This five-cent pill became the most prescribed drug in the world after being approved by the FDA in 1994.
With so many people taking it, ever larger studies began suggesting metformin's positive potential effects preventing diabetes, cardiovascular diseases, cancer, and dementia. In fact, elderly people on metformin for their diabetes have around a 20 percent lower mortality than age-matched subjects without diabetes. Results like these led scientists to hypothesize that metformin wasn't just impacting a few individual diseases but instead having a systemic impact on entire organisms.
Another class of drug that seems to slow the systemic process of aging in animal models and very preliminary human trials inhibits a nutrient-sensing cellular protein called mTOR. A new category of drugs called rapalogues has been shown to extend healthspan and lifespan in every type of non-human animal so far tested. Two recent human studies indicated that rapalogues increased resistance to the flu and decreased the severity of respiratory tract infections in older adults.
If COVID-19 is primarily a severe disease of aging, then countering aging should logically go a long way in countering the disease.
These promising early indications have inspired a recently launched long-term study exploring how metformin and rapalogues might delay the onset of multiple, age-related diseases and slow the biological process of aging in humans. Under normal circumstances, studies like this seeking to crack the biological code of aging would continue to proceed slowly and carefully over years, moving from animal experiments to cautious series of human trials. But with deaths rising by the day, particularly of older people, these are not times for half measures. Wartimes have always demanded new ways of doing important things at warp speeds.
If COVID-19 is primarily a severe disease of aging, then countering aging should logically go a long way in countering the disease. We need to find out. Fast.
Although it would be a mistake for older people to just begin taking drugs like these without any indication, pushing to massively speed up our process for assessing whether these types of interventions can help protect older people is suddenly critical.
To do this, we need U.S. government agencies like the Department of Health and Human Services' Biomedical Advanced Research and Development Authority (BARDA) to step up. BARDA currently only funds COVID-19 clinical trials of drugs that can be dosed once and provide 60 days of protection. Metformin and rapalogues are not considered for BARDA funding because they are dosed once daily. This makes no sense because a drug that provides 60 days of protection from the coronavirus after a single dose does not yet exist, while metformin and rapalogues have already passed extensive safety tests. Instead, BARDA should consider speeding up trials with currently available drugs that could help at least some of the elderly populations at risk.
Although the U.S. Food and Drug Administration and Centers for Disease Control are ramping up their approval processes and even then needs to prioritize efforts, they too must find a better balance between appropriate regulatory caution and the dire necessities of our current moment. Drugs like metformin and rapalogues that have shown preliminary efficacy ought to be fast-tracked for careful consideration.
One day we will develop a COVID-19 vaccine to help everyone. But that could be at least a year from now, if not more. Until we get there and even after we do, speeding up our process of fortifying our older populations mush be a central component of our wartime strategy.
And when the war is won and life goes back to a more normal state, we'll get the added side benefit of a few more months and ultimately years with our parents and grandparents.
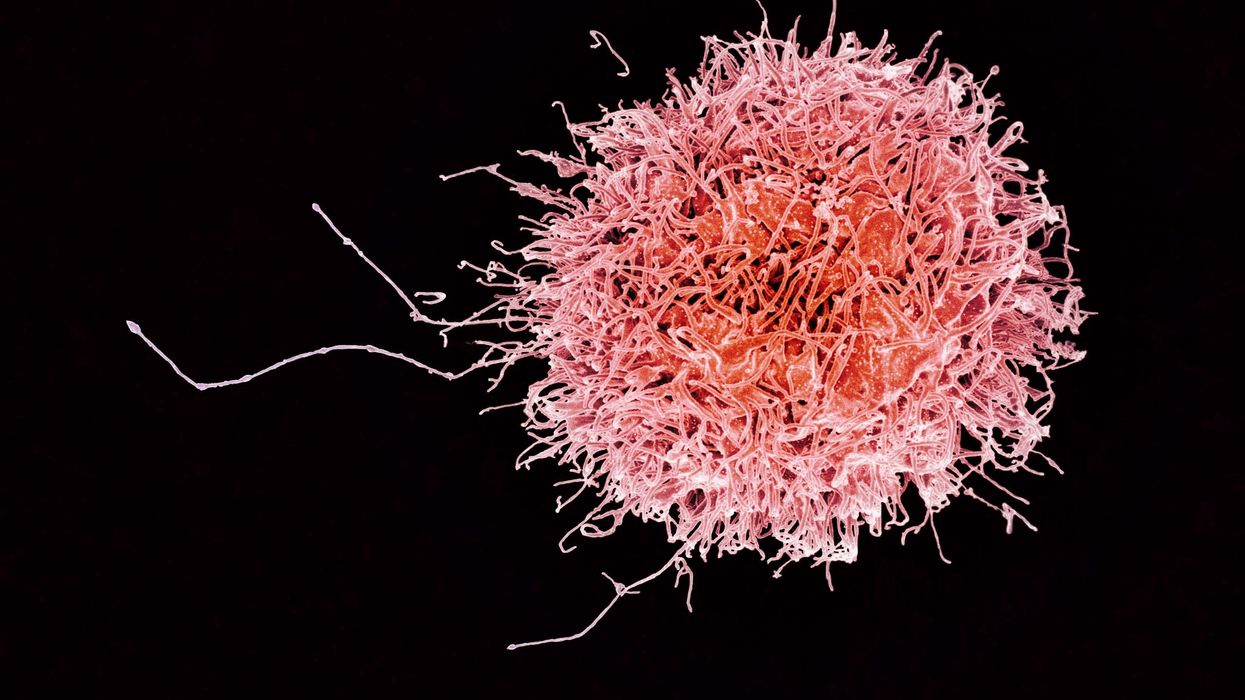
On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business

Is there a robot nanny in your child's future?
Some researchers argue that active, playful engagement with a "robot nanny" for a few hours a day is better than several hours in front of a TV or with an iPad.
From ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold. Copyright © 2024 by the author and reprinted by permission of St. Martin’s Publishing Group.
Could the use of robots take some of the workload off teachers, add engagement among students, and ultimately invigorate learning by taking it to a new level that is more consonant with the everyday experiences of young people? Do robots have the potential to become full-fledged educators and further push human teachers out of the profession? The preponderance of opinion on this subject is that, just as AI and medical technology are not going to eliminate doctors, robot teachers will never replace human teachers. Rather, they will change the job of teaching.
A 2017 study led by Google executive James Manyika suggested that skills like creativity, emotional intelligence, and communication will always be needed in the classroom and that robots aren’t likely to provide them at the same level that humans naturally do. But robot teachers do bring advantages, such as a depth of subject knowledge that teachers can’t match, and they’re great for student engagement.
The teacher and robot can complement each other in new ways, with the teacher facilitating interactions between robots and students. So far, this is the case with teaching “assistants” being adopted now in China, Japan, the U.S., and Europe. In this scenario, the robot (usually the SoftBank child-size robot NAO) is a tool for teaching mainly science, technology, engineering, and math (the STEM subjects), but the teacher is very involved in planning, overseeing, and evaluating progress. The students get an entertaining and enriched learning experience, and some of the teaching load is taken off the teacher. At least, that’s what researchers have been able to observe so far.
To be sure, there are some powerful arguments for having robots in the classroom. A not-to-be-underestimated one is that robots “speak the language” of today’s children, who have been steeped in technology since birth. These children are adept at navigating a media-rich environment that is highly visual and interactive. They are plugged into the Internet 24-7. They consume music, games, and huge numbers of videos on a weekly basis. They expect to be dazzled because they are used to being dazzled by more and more spectacular displays of digital artistry. Education has to compete with social media and the entertainment vehicles of students’ everyday lives.
Another compelling argument for teaching robots is that they help prepare students for the technological realities they will encounter in the real world when robots will be ubiquitous. From childhood on, they will be interacting and collaborating with robots in every sphere of their lives from the jobs they do to dealing with retail robots and helper robots in the home. Including robots in the classroom is one way of making sure that children of all socioeconomic backgrounds will be better prepared for a highly automated age, when successfully using robots will be as essential as reading and writing. We’ve already crossed this threshold with computers and smartphones.
Students need multimedia entertainment with their teaching. This is something robots can provide through their ability to connect to the Internet and act as a centralized host to videos, music, and games. Children also need interaction, something robots can deliver up to a point, but which humans can surpass. The education of a child is not just intended to make them technologically functional in a wired world, it’s to help them grow in intellectual, creative, social, and emotional ways. When considered through this perspective, it opens the door to questions concerning just how far robots should go. Robots don’t just teach and engage children; they’re designed to tug at their heartstrings.
It’s no coincidence that many toy makers and manufacturers are designing cute robots that look and behave like real children or animals, says Turkle. “When they make eye contact and gesture toward us, they predispose us to view them as thinking and caring,” she has written in The Washington Post. “They are designed to be cute, to provide a nurturing response” from the child. As mentioned previously, this nurturing experience is a powerful vehicle for drawing children in and promoting strong attachment. But should children really love their robots?
ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold (January 9, 2024).
St. Martin’s Publishing Group
The problem, once again, is that a child can be lulled into thinking that she’s in an actual relationship, when a robot can’t possibly love her back. If adults have these vulnerabilities, what might such asymmetrical relationships do to the emotional development of a small child? Turkle notes that while we tend to ascribe a mind and emotions to a socially interactive robot, “simulated thinking may be thinking, but simulated feeling is never feeling, and simulated love is never love.”
Always a consideration is the fact that in the first few years of life, a child’s brain is undergoing rapid growth and development that will form the foundation of their lifelong emotional health. These formative experiences are literally shaping the child’s brain, their expectations, and their view of the world and their place in it. In Alone Together, Turkle asks: What are we saying to children about their importance to us when we’re willing to outsource their care to a robot? A child might be superficially entertained by the robot while his self-esteem is systematically undermined.
Research has emerged showing that there are clear downsides to child-robot relationships.
Still, in the case of robot nannies in the home, is active, playful engagement with a robot for a few hours a day any more harmful than several hours in front of a TV or with an iPad? Some, like Xiong, regard interacting with a robot as better than mere passive entertainment. iPal’s manufacturers say that their robot can’t replace parents or teachers and is best used by three- to eight-year-olds after school, while they wait for their parents to get off work. But as robots become ever-more sophisticated, they’re expected to perform more of the tasks of day-to-day care and to be much more emotionally advanced. There is no question children will form deep attachments to some of them. And research has emerged showing that there are clear downsides to child-robot relationships.
Some studies, performed by Turkle and fellow MIT colleague Cynthia Breazeal, have revealed a darker side to the child-robot bond. Turkle has reported extensively on these studies in The Washington Post and in her book Alone Together. Most children love robots, but some act out their inner bully on the hapless machines, hitting and kicking them and otherwise trying to hurt them. The trouble is that the robot can’t fight back, teaching children that they can bully and abuse without consequences. As in any other robot relationship, such harmful behavior could carry over into the child’s human relationships.
And, ironically, it turns out that communicative machines don’t actually teach kids good communication skills. It’s well known that parent-child communication in the first three years of life sets the stage for a very young child’s intellectual and academic success. Verbal back-and-forth with parents and care-givers is like fuel for a child’s growing brain. One article that examined several types of play and their effect on children’s communication skills, published in JAMA Pediatrics in 2015, showed that babies who played with electronic toys—like the popular robot dog Aibo—show a decrease in both the quantity and quality of their language skills.
Anna V. Sosa of the Child Speech and Language Lab at Northern Arizona University studied twenty-six ten- to sixteen- month-old infants to compare the growth of their language skills after they played with three types of toys: electronic toys like a baby laptop and talking farm; traditional toys like wooden puzzles and building blocks; and books read aloud by their parents. The play that produced the most growth in verbal ability was having books read to them by a caregiver, followed by play with traditional toys. Language gains after playing with electronic toys came dead last. This form of play involved the least use of adult words, the least conversational turntaking, and the least verbalizations from the children. While the study sample was small, it’s not hard to extrapolate that no electronic toy or even more abled robot could supply the intimate responsiveness of a parent reading stories to a child, explaining new words, answering the child’s questions, and modeling the kind of back- and-forth interaction that promotes empathy and reciprocity in relationships.
***
Most experts acknowledge that robots can be valuable educational tools. But they can’t make a child feel truly loved, validated, and valued. That’s the job of parents, and when parents abdicate this responsibility, it’s not only the child who misses out on one of life’s most profound experiences.
We really don’t know how the tech-savvy children of today will ultimately process their attachments to robots and whether they will be excessively predisposed to choosing robot companionship over that of humans. It’s possible their techno literacy will draw for them a bold line between real life and a quasi-imaginary history with a robot. But it will be decades before we see long-term studies culminating in sufficient data to help scientists, and the rest of us, to parse out the effects of a lifetime spent with robots.
This is an excerpt from ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold. The book will be published on January 9, 2024.