Drugs That Trick Older People’s Bodies to Behave Younger Might Boost the Effectiveness of a COVID-19 Vaccine

Because vaccination may be less effective in older people, it is imperative to test now whether immune boosters could help the efficacy of a COVID-19 vaccine in the elderly.
In our April 23rd editorial for this magazine, we argued that addressing the COVID-19 pandemic requires that we both fight the SARS-CoV-2 virus and fortify the human hosts who are most vulnerable to it.
Two recent phase 2 studies in older adults have suggested that a new category of drugs called rapalogues can in some cases increase the immunization capacity of older adults.
Because people over 70 account for more than 80 percent of reported COVID-19 deaths globally, this means we must do everything possible to protect our elders.
A range of recent studies have suggested that systemic knobs might metaphorically be turned to slow the cellular aging process, making us better able to fight off the many diseases correlated with aging. These types of systemic changes might be used to stem the specific decline in immunity caused by aging and to increases the biological capacity of elderly people to effectively fight viral infection.
But while helping make older people more resilient in the face of a viral infection is critical, that's not the only way geroscience can help in our fight against this deadly pandemic.
As we move toward hopefully developing one or more COVID-19 vaccines, researchers must more fully appreciate the ways in which traditional vaccines can be less effective in older people than in younger ones.
Repeated studies have shown that the flu vaccine, for example, has lower efficacy in older people than in younger ones. Older people tend to develop fewer antibodies after being vaccinated because a subset of their white blood cells, called T cells, have become less responsive over time. Some inflammatory peptides that increase with aging are also preventing the action of those T cells.
This is why there's a distinct possibility that a future COVD-19 vaccine, particularly one utilizing the traditional attenuated virus approach, could be less effective in older people than in younger ones.
Given the extreme urgency of developing vaccines that work well for everyone, we need to make sure that researchers are exploring all of the ways our elders can be best protected. While generating a vaccine that works equally well for people of all ages would be ideal, we can't count on that.
One way to bridge this gap might be to trick the bodies of older people into behaving as if they are younger just at the moment what a vaccine is delivered by giving them pre-immunization boosters.
Two recent phase 2 studies in older adults have suggested that a new category of drugs called rapalogues can in some cases increase the immunization capacity of older adults. Use of the drug for a short time period before flu shot immunization increased the antibody production for the flu and resulted in a 52 percent decrease in the occurrence of severe diseases needing medical help or hospitalization. This short-term pre-immunization intervention can also decrease the severity of serious respiratory tract infections, the deadliest manifestations of COVID-19, by similar magnitude. These patients also had almost half the incidence of the non-COVID-19 coronaviruses associated with the common cold.
The fact that those people were protected by treatment before hospitalization suggests metformin may have a role in boosting the vaccination of older people.
An inexpensive generic drug called metformin similarly targets the decline in immunity and inflammation (and extends health span and lifespan) in animals and has been used for decades to protect against the flu. A recent paper from a hospital in Wuhan, China showed that mortality of elderly COVID-19 diabetic patients on metformin was 25 percent less than that of patients with diabetes but not on metformin.
Another study from the U.S. showed that COVID-19 patients on metformin had a 20 percent decrease in mortality and lower inflammation. The fact that those people were protected by treatment before hospitalization suggests metformin may have a role in boosting the vaccination of older people.
We don't yet know whether rapalogues or metformin could be used as COVID-19 immunization boosters, not least because we don't have those vaccines. But we can and should make sure that all vaccine trials including older subjects also consider offering a subset of those subjects appropriate doses of rapalogues or metformin to explore whether doing so can boost the efficacy of a given vaccine.
If we weren't in the middle of the worst pandemic in a century, we would have more time to test our vaccines slowly and sequentially. In the context of the current crisis, however, testing whether immunization boosters might increase the efficacy of potential COVID-19 vaccines for older adults is at the very least a hypothesis worth exploring.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
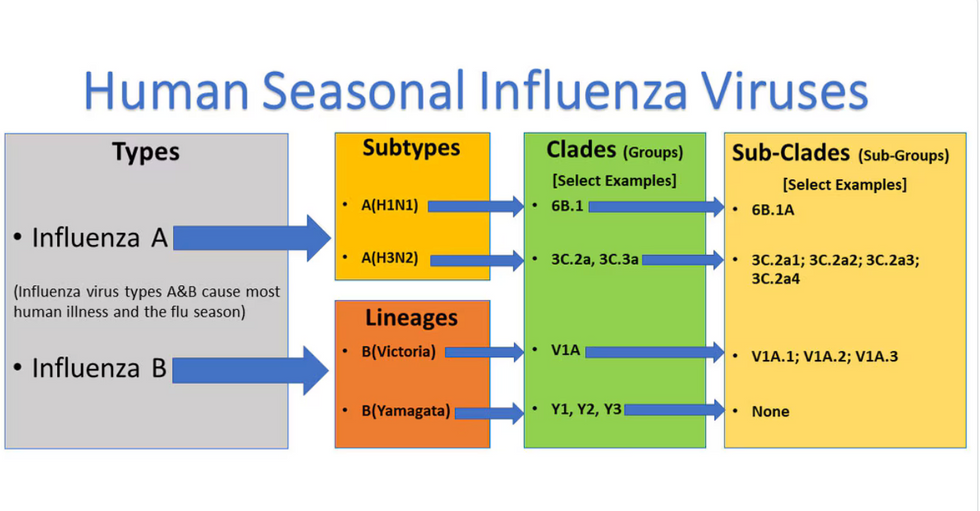
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

