This Boy Struggled to Walk Before Gene Therapy. Now, Such Treatments Are Poised to Explode.

Conner Curran, now 10 years old, can walk more than two miles after gene therapy treatment for his Duchenne's muscular dystrophy.
Conner Curran was diagnosed with Duchenne's muscular dystrophy in 2015 when he was four years old. It's the most severe form of the genetic disease, with a nearly inevitable progression toward total paralysis. Many Duchenne's patients die in their teens; the average lifespan is 26.
But Conner, who is now 10, has experienced some astonishing improvements in recent years. He can now walk for more than two miles at a time – an impossible journey when he was younger.
In 2018, Conner became the very first patient to receive gene therapy specific to treating Duchenne's. In the initial clinical trial of nine children, nearly 80 percent reacted positively to the treatment). A larger-scale stage 3 clinical trial is currently underway, with initial results expected next year.
Gene therapy involves altering the genes in an individual's cells to stop or treat a disease. Such a procedure may be performed by adding new gene material to existing cells, or editing the defective genes to improve their functionality.
That the medical world is on the cusp of a successful treatment for a crippling and deadly disease is the culmination of more than 35 years of work by Dr. Jude Samulski, a professor of pharmacology at the University of North Carolina School of Medicine in Chapel Hill. More recently, he's become a leading gene therapy entrepreneur.
But Samulski likens this breakthrough to the frustrations of solving a Rubik's cube. "Just because one side is now all the color yellow does not mean that it is completely aligned," he says.
Although Conner's life and future have dramatically improved, he's not cured. The gene therapy tamed but did not extinguish his disorder: Conner is now suffering from the equivalent of Becker's muscular dystrophy, a milder form of the disease with symptoms that appear later in life and progress more slowly. Moreover, the loss of muscle cells Conner suffered prior to the treatment is permanent.
"It will take more time and more innovations," Samulski says of finding an even more effective gene therapy for muscular dystrophy.
Conner's family is still overjoyed with the results. "Jude's grit and determination gave Conner a chance at a new life, one that was not in his cards before gene therapy," says his mother Jessica Curran. She adds that "Conner is more confident than before and enjoys life, even though he has limitations, if compared to his brothers or peers."

Conner Curran holding a football post gene therapy treatment.
Courtesy of the Curran family
For now, the use of gene therapy as a treatment for diseases and disorders remains relatively isolated. On paper at least, progress appears glacially slow. In 2018, there were four FDA-approved gene therapies (excluding those reliant on bone marrow/stem cell transplants or implants). Today, there are 10. One therapy is solely for the cosmetic purpose of reducing facial lines and folds.
Nevertheless, experts in the space believe gene therapy is poised to expand dramatically.
"Certainly in the next three to five years you will see dozens of gene therapies and cell therapies be approved," says Dr. Pavan Cheruvu, who is CEO of Sio Gene Therapies in New York. The company is developing treatments for Parkinson's disease and Tay-Sachs, among other diseases.
Cheruvu's conclusion is supported by NEWDIGS, a think tank at the Massachusetts Institute of Technology that keeps tabs on gene therapy developments. NEWDIGS predicts there will be at least 60 gene therapies approved for use in the U.S. by the end of the decade. That number could be closer to 100 if Chinese researchers and biotech ventures decide the American market is a good fit for the therapies they develop.
"We are watching something of a conditional evolution, like a dot-com, or cellphones that were sizes of shoeboxes that have now matured to the size of wafers. Our space will follow along very similarly."
Dr. Carsten Brunn, a chemist by training and CEO of Selecta Biosciences outside of Boston, is developing ways to reduce the immune responses in patients who receive gene therapy. He observes that there are more than 300 therapies in development and thousands of clinical trials underway. "It's definitely an exciting time in the field," he says.
That's a far cry from the environment of little more than a decade ago. Research and investment in gene therapy had been brought low for years after the death of teenager Jesse Gelsinger in 1999 while he had been enrolled in a clinical trial to treat a liver disease. Gene therapy was a completely novel concept back then, and his death created existential questions about whether it was a proper pathway to pursue. Cheruvu, a cardiologist, calls the years after Gelsinger's death an "ice age" for gene therapy.
However, those dark years eventually yielded to a thaw. And while there have been some recent stumbles, they are considered part of the trial-and-error that has often accompanied medical research as opposed to an ominous "stop" sign.
The deaths of three patients last year receiving gene therapy for myotubular myopathy – a degenerative disease that causes severe muscle weakness – promptly ended the clinical trial in which they were enrolled. However, the incident caused few ripples beyond that. Researchers linked the deaths to dosage sizes that caused liver toxicity, as opposed to the gene therapy itself being an automatic death sentence; younger patients who received lower doses due to a less advanced disease state experienced improvements.
The gene sequencing and editing that helped create vaccines for COVID-19 in record time also bolstered the argument for more investment in research and development. Cheruvu notes that the field has usually been the domain of investors with significant expertise in the field; these days, more money is flowing in from generalists.
The Challenges Ahead
What will be the next step in gene therapy's evolution? Many of Samulski's earliest innovations came in the laboratory, for example. Then that led to him forming a company called AskBio in collaboration with the Muscular Dystrophy Association. AskBio sold its gene therapy to Pfizer five years ago to assure that enough could be manufactured for stage 3 clinical trials and eventually reach the market.
Cheruvu suggests that many future gene therapy innovations will be the result of what he calls "congruent innovation." That means publicly funded laboratories and privately funded companies might develop treatments separately or in collaboration. Or, university scientists may depend on private ventures to solve one of gene therapy's most vexing issues: producing enough finished material to test and treat on a large scale. "Manufacturing is a real bottleneck right now," Brunn says.
The alternative is referred to in the sector as the "valley of death": a lab has found a promising treatment, but is not far enough along in development to submit an investigational new drug application with the FDA. The promise withers away as a result. But the new abundance of venture capital for gene therapy has made this scenario less of an issue for private firms, some of which have received hundreds of millions of dollars in funding.
There are also numerous clinical challenges. Many gene therapies use what are known as adeno-associated virus vectors (AAVs) to deliver treatments. They are hollowed-out husks of viruses that can cause a variety of mostly mild maladies ranging from colds to pink eye. They are modified to deliver the genetic material used in the therapy. Most of these vectors trigger an antibody reaction that limits treatments to a single does or a handful of smaller ones. That can limit the potential progress for patients – an issue referred to as treatment "durability."
Although vectors from animals such as horses trigger far less of an antibody reaction in patients -- and there has been significant work done on using artificial vectors -- both are likely years away from being used on a large scale. "For the foreseeable future, AAV is the delivery system of choice," Brunn says.
Also, there will likely be demand for concurrent gene therapies that can lead to a complete cure – not only halting the progress of Duchenne's in kids like Conner Curran, but regenerating their lost muscle cells, perhaps through some form of stem cell therapy or another treatment that has yet to be devised.
Nevertheless, Samulski believes demand for imperfect treatments will be high – particularly with a disease such as muscular dystrophy, where many patients are mere months from spending the remainder of their lives in wheelchairs. But Samulski believes those therapies will also inevitably evolve into something far more effective.
"We are watching something of a conditional evolution, like a dot-com, or cellphones that were sizes of shoeboxes that have now matured to the size of wafers," he says. "Our space will follow along very similarly."
Jessica Curran will remain forever grateful for what her son has received: "Jude gave us new hope. He gave us something that is priceless – a chance to watch Conner grow up and live out his own dreams."
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
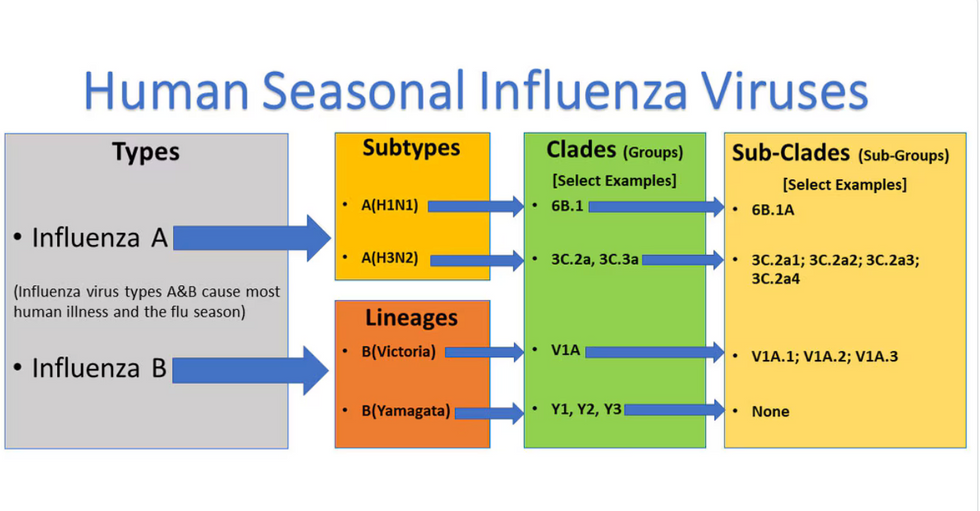
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

