How Will the New Strains of COVID-19 Affect Our Vaccination Plans?

The mutated strains that first arose in the U.K. and South Africa and have now spread to many countries are prompting urgent studies on the effectiveness of current vaccines to neutralize the new strains.
When the world's first Covid-19 vaccine received regulatory approval in November, it appeared that the end of the pandemic might be near. As one by one, the Pfizer/BioNTech, Moderna, AstraZeneca, and Sputnik V vaccines reported successful Phase III results, the prospect of life without lockdowns and restrictions seemed a tantalizing possibility.
But for scientists with many years' worth of experience in studying how viruses adapt over time, it remained clear that the fight against the SARS-CoV-2 virus was far from over. "The more virus circulates, the more it is likely that mutations occur," said Professor Beate Kampmann, director of the Vaccine Centre at the London School of Hygiene & Tropical Medicine. "It is inevitable that new variants will emerge."
Since the start of the pandemic, dozens of new variants of SARS-CoV-2 – containing different mutations in the viral genome sequence - have appeared as it copies itself while spreading through the human population. The majority of these mutations are inconsequential, but in recent months, some mutations have emerged in the receptor binding domain of the virus's spike protein, increasing how tightly it binds to human cells. These mutations appear to make some new strains up to 70 percent more transmissible, though estimates vary and more lab experiments are needed. Such new strains include the B.1.1.7 variant - currently the dominant strain in the UK – and the 501Y.V2 variant, which was first found in South Africa.
"I'm quite optimistic that even with these mutations, immunity is not going to suddenly fail on us."
Because so many more people are becoming infected with the SARS-CoV-2 virus as a result, vaccinologists point out that these new strains will prolong the pandemic.
"It may take longer to reach vaccine-induced herd immunity," says Deborah Fuller, professor of microbiology at the University of Washington School of Medicine. "With a more transmissible variant taking over, an even larger percentage of the population will need to get vaccinated before we can shut this pandemic down."
That is, of course, as long as the vaccinations are still highly protective. The South African variant, in particular, contains a mutation called E484K that is raising alarms among scientists. Emerging evidence indicates that this mutation allows the virus to escape from some people's immune responses, and thus could potentially weaken the effectiveness of current vaccines.
What We Know So Far
Over the past few weeks, manufacturers of the approved Covid-19 vaccines have been racing to conduct experiments, assessing whether their jabs still work well against the new variants. This process involves taking blood samples from people who have already been vaccinated and assessing whether the antibodies generated by those people can neutralize the new strains in a test tube.
Pfizer has just released results from the first of these studies, declaring that their vaccine was found to still be effective at neutralizing strains of the virus containing the N501Y mutation of the spike protein, one of the mutations present within both the UK and South African variants.
However, the study did not look at the full set of mutations contained within either of these variants. Earlier this week, academics at the Fred Hutchinson Cancer Research Center in Seattle suggested that the E484K spike protein mutation could be most problematic, publishing a study which showed that the efficacy of neutralizing antibodies against this region dropped by more than ten-fold because of the mutation.
Thankfully, this development is not expected to make vaccines useless. One of the Fred Hutch researchers, Jesse Bloom, told STAT News that he did not expect this mutation to seriously reduce vaccine efficacy, and that more harmful mutations would need to accrue over time to pose a very significant threat to vaccinations.
"I'm quite optimistic that even with these mutations, immunity is not going to suddenly fail on us," Bloom told STAT. "It might be gradually eroded, but it's not going to fail on us, at least in the short term."
While further vaccine efficacy data will emerge in the coming weeks, other vaccinologists are keen to stress this same point: At most, there will be a marginal drop in efficacy against the new variants.
"Each vaccine induces what we call polyclonal antibodies targeting multiple parts of the spike protein," said Fuller. "So if one antibody target mutates, there are other antibody targets on the spike protein that could still neutralize the virus. The vaccine platforms also induce T-cell responses that could provide a second line of defense. If some virus gets past antibodies, T-cell responses can find and eliminate infected cells before the virus does too much damage."
She estimates that if vaccine efficacy decreases, for example from 95% to 85%, against one of the new variants, the main implications will be that some individuals who might otherwise have become severely ill, may still experience mild or moderate symptoms from an infection -- but crucially, they will not end up in intensive care.
"Plug and Play" Vaccine Platforms
One of the advantages of the technologies which have been pioneered to create the Covid-19 vaccines is that they are relatively straightforward to update with a new viral sequence. The mRNA technology used in the Pfizer/BioNTech and Moderna vaccines, and the adenovirus vectors used in the Astra Zeneca and Sputnik V vaccines, are known as 'plug and play' platforms, meaning that a new form of the vaccine can be rapidly generated against any emerging variant.
"With a rapid pipeline for manufacture established, these new vaccine technologies could enable production and distribution within 1-3 months of a new variant emerging."
While the technology for the seasonal influenza vaccines is relatively inefficient, requiring scientists to grow and cultivate the new strain in the lab before vaccines can be produced - a process that takes nine months - mRNA and adenovirus-based vaccines can be updated within a matter of weeks. According to BioNTech CEO Uğur Şahin, a new version of their vaccine could be produced in six weeks.
"With a rapid pipeline for manufacture established, these new vaccine technologies could enable production and distribution within 1-3 months of a new variant emerging," says Fuller.
Fuller predicts that more new variants of the virus are almost certain to emerge within the coming months and years, potentially requiring the public to receive booster shots. This means there is one key advantage the mRNA-based vaccines have over the adenovirus technologies. mRNA vaccines only express the spike protein, while the AstraZeneca and Sputnik V vaccines use adenoviruses - common viruses most of us are exposed to - as a delivery mechanism for genes from the SARS-CoV-2 virus.
"For the adenovirus vaccines, our bodies make immune responses against both SARS-CoV-2 and the adenovirus backbone of the vaccine," says Fuller. "That means if you update the adenovirus-based vaccine with the new variant and then try to boost people, they may respond less well to the new vaccine, because they already have antibodies against the adenovirus that could block the vaccine from working. This makes mRNA vaccines more amenable to repeated use."
Regulatory Unknowns
One of the key questions remains whether regulators would require new versions of the vaccine to go through clinical trials, a hurdle which would slow down the response to emerging strains, or whether the seasonal influenza paradigm will be followed, whereby a new form of the vaccine can be released without further clinical testing.
Regulators are currently remaining tight-lipped on which process they will choose to follow, until there is more information on how vaccines respond against the new variants. "Only when such information becomes available can we start the scientific evaluation of what data would be needed to support such a change and assess what regulatory procedure would be required for that," said Rebecca Harding, communications officer for the European Medicines Agency.
The Food and Drug Administration (FDA) did not respond to requests for comment before press time.
While vaccinologists feel it is unlikely that a new complete Phase III trial would be required, some believe that because these are new technologies, regulators may well demand further safety data before approving an updated version of the vaccine.
"I would hope if we ever have to update the current vaccines, regulatory authorities will treat it like influenza," said Drew Weissman, professor of medicine at the University of Pennsylvania, who was involved in developing the mRNA technology behind the Pfizer/BioNTech and Moderna vaccines. "I would guess, at worst, they may want a new Phase 1 or 1 and 2 clinical trials."
Others suggest that rather than new trials, some bridging experiments may suffice to demonstrate that the levels of neutralizing antibodies induced by the new form of the vaccine are comparable to the previous one. "Vaccines have previously been licensed by this kind of immunogenicity data only, for example meningitis vaccines," said Kampmann.
While further mutations and strains of SARS-CoV-2 are inevitable, some scientists are concerned that the vaccine rollout strategy being employed in some countries -- of distributing a first shot to as many people as possible, and potentially delaying second shots as a result -- could encourage more new variants to emerge. Just today, the Biden administration announced its intention to release nearly all vaccine doses on hand right away, without keeping a reserve for second shots. This plan risks relying on vaccine manufacturing to ramp up quickly to keep pace if people are to receive their second shots at the right intervals.
"I am not very happy about this change as it could lead to a large number of people out there with partial immunity and this could select new mutations, and escalate the potential problem of vaccine escape."
The Biden administration's shift appears to conflict with the FDA's recent position that second doses should be given on a strict schedule, without any departure from the three- and four-week intervals established in clinical trials. Two top FDA officials said in a statement that changing the dosing schedule "is premature and not rooted solidly in the available evidence. Without appropriate data supporting such changes in vaccine administration, we run a significant risk of placing public health at risk, undermining the historic vaccination efforts to protect the population from COVID-19."
"I understand the argument of trying to get at least partial protection to as many people as possible, but I am concerned about the increased interval between the doses that is now being proposed," said Kampmann. "I am not very happy about this change as it could lead to a large number of people out there with partial immunity and this could select new mutations, and escalate the potential problem of vaccine escape."
But it's worth emphasizing that the virus is unlikely for now to accumulate enough harmful mutations to render the current vaccines completely ineffective.
"It will be very hard for the virus to evolve to completely evade the antibody responses the vaccines induce," said Fuller. "The parts of the virus that are targeted by vaccine-induced antibodies are essential for the virus to infect our cells. If the virus tries to mutate these parts to evade antibodies, then it could compromise its own fitness or even abort its ability to infect. To be sure, the virus is developing these mutations, but we just don't see these variants emerge because they die out."
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
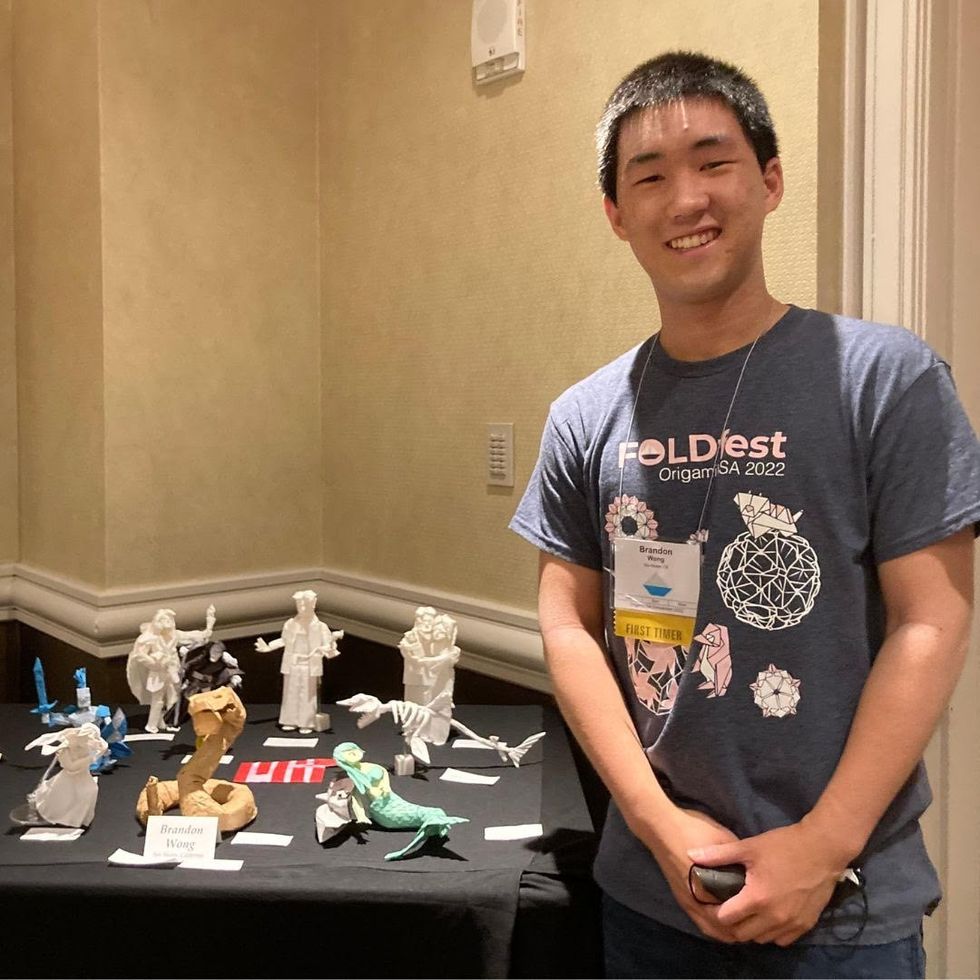
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

