Eight Big Medical and Science Trends to Watch in 2021

Promising developments underway include advancements in gene and cell therapy, better testing for COVID, and a renewed focus on climate change.
The world as we know it has forever changed. With a greater focus on science and technology than before, experts in the biotech and life sciences spaces are grappling with what comes next as SARS-CoV-2, the coronavirus that causes the COVID-19 illness, has spread and mutated across the world.
Even with vaccines being distributed, so much still remains unknown.
Jared Auclair, Technical Supervisor for the Northeastern University's Life Science Testing Center in Burlington, Massachusetts, guides a COVID testing lab that cranks out thousands of coronavirus test results per day. His lab is also focused on monitoring the quality of new cell and gene therapy products coming to the market.
Here are trends Auclair and other experts are watching in 2021.
Better Diagnostic Testing for COVID
Expect improvements in COVID diagnostic testing and the ability to test at home.
There are currently three types of coronavirus tests. The molecular test—also known as the RT-PCR test, detects the virus's genetic material, and is highly accurate, but it can take days to receive results. There are also antibody tests, done through a blood draw, designed to test whether you've had COVID in the past. Finally, there's the quick antigen test that isn't as accurate as the PCR test, but can identify if people are going to infect others.
Last month, Lucira Health secured the U.S. FDA Emergency Use Authorization for the first prescription molecular diagnostic test for COVID-19 that can be performed at home. On December 15th, the Ellume Covid-19 Home Test received authorization as the first over-the-counter COVID-19 diagnostic antigen test that can be done at home without a prescription. The test uses a nasal swab that is connected to a smartphone app and returns results in 15-20 minutes. Similarly, the BinaxNOW COVID-19 Ag Card Home Test received authorization on Dec. 16 for its 15-minute antigen test that can be used within the first seven days of onset of COIVD-19 symptoms.
Home testing has the possibility to impact the pandemic pretty drastically, Auclair says, but there are other considerations: the type and timing of test that is administered, how expensive is the test (and if it is financially feasible for the general public) and the ability of a home test taker to accurately administer the test.
"The vaccine roll-out will not eliminate the need for testing until late 2021 or early 2022."
Ideally, everyone would frequently get tested, but that would mean the cost of a single home test—which is expected to be around $30 or more—would need to be much cheaper, more in the $5 range.
Auclair expects "innovations in the diagnostic space to explode" with the need for more accurate, inexpensive, quicker COVID tests. Auclair foresees innovations to be at first focused on COVID point-of-care testing, but he expects improvements within diagnostic testing for other types of viruses and diseases too.
"We still need more testing to get the pandemic under control, likely over the next 12 months," Auclair says. "The vaccine roll-out will not eliminate the need for testing until late 2021 or early 2022."
Rise of mRNA-based Vaccines and Therapies
A year ago, vaccines weren't being talked about like they are today.
"But clearly vaccines are the talk of the town," Auclair says. "The reason we got a vaccine so fast was there was so much money thrown at it."
A vaccine can take more than 10 years to fully develop, according to the World Economic Forum. Prior to the new COVID vaccines, which were remarkably developed and tested in under a year, the fastest vaccine ever made was for mumps -- and it took four years.
"Normally you have to produce a protein. This is typically done in eggs. It takes forever," says Catherine Dulac, a neuroscientist and developmental biologist at Harvard University who won the 2021 Breakthrough Prize in Life Sciences. "But an mRNA vaccine just enabled [us] to skip all sorts of steps [compared with burdensome conventional manufacturing] and go directly to a product that can be injected into people."
Non-traditional medicines based on genetic research are in their infancy. With mRNA-based vaccines hitting the market for the first time, look for more vaccines to be developed for whatever viruses we don't currently have vaccines for, like dengue virus and Ebola, Auclair says.
"There's a whole bunch of things that could be explored now that haven't been thought about in the past," Auclair says. "It could really be a game changer."
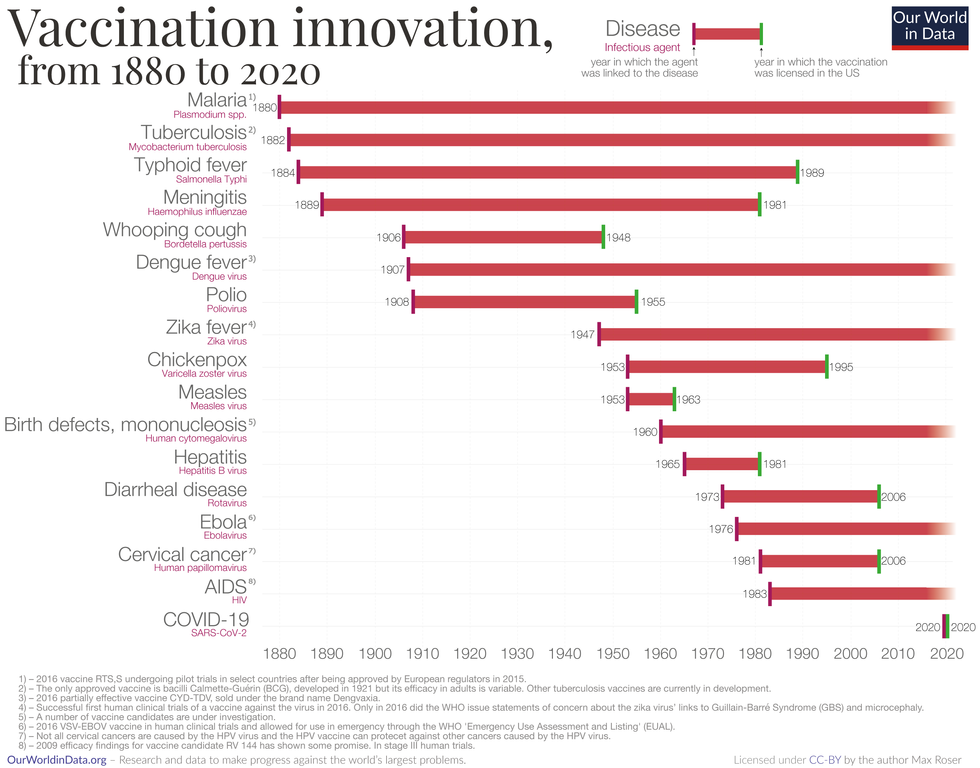
Vaccine Innovation over the last 140 years.
Max Roser/Our World in Data (Creative Commons license)
Advancements in Cell and Gene Therapies
CRISPR, a type of gene editing, is going to be huge in 2021, especially after the Nobel Prize in Chemistry was awarded to Emmanuelle Charpentier and Jennifer Doudna in October for pioneering the technology.
Right now, CRISPR isn't completely precise and can cause deletions or rearrangements of DNA.
"It's definitely not there yet, but over the next year it's going to get a lot closer and you're going to have a lot of momentum in this space," Auclair says. "CRISPR is one of the technologies I'm most excited about and 2021 is the year for it."
Gene therapies are typically used on rare genetic diseases. They work by replacing the faulty dysfunctional genes with corrected DNA codes.
"Cell and gene therapies are really where the field is going," Auclair says. "There is so much opportunity....For the first time in our life, in our existence as a species, we may actually be able to cure disease by using [techniques] like gene editing, where you cut in and out of pieces of DNA that caused a disease and put in healthy DNA," Auclair says.
For example, Spinal Muscular Atrophy is a rare genetic disorder that leads to muscle weakness, paralysis and death in children by age two. As of last year, afflicted children can take a gene therapy drug called Zolgensma that targets the missing or nonworking SMN1 gene with a new copy.
Another recent breakthrough uses gene editing for sickle cell disease. Victoria Gray, a mom from Mississippi who was exclusively followed by NPR, was the first person in the United States to be successfully treated for the genetic disorder with the help of CRISPR. She has continued to improve since her landmark treatment on July 2, 2019 and her once-debilitating pain has greatly eased.
"This is really a life-changer for me," she told NPR. "It's magnificent."
"You are going to see bigger leaps in gene therapies."
Look out also for improvements in cell therapies, but on a much lesser scale.
Cell therapies remove immune cells from a person or use cells from a donor. The cells are modified or cultured in lab, multiplied by the millions and then injected back into patients. These include stem cell therapies as well as CAR-T cell therapies, which are typically therapies of last resort and used in cancers like leukemia, Auclair says.
"You are going to see bigger leaps in gene therapies," Auclair says. "It's being heavily researched and we understand more about how to do gene therapies. Cell therapies will lie behind it a bit because they are so much more difficult to work with right now."
More Monoclonal Antibody Therapies
Look for more customized drugs to personalize medicine even more in the biotechnology space.
In 2019, the FDA anticipated receiving more than 200 Investigational New Drug (IND) applications in 2020. But with COVID, the number of INDs skyrocketed to 6,954 applications for the 2020 fiscal year, which ended September 30, 2020, according to the FDA's online tracker. Look for antibody therapies to play a bigger role.
Monoclonal antibodies are lab-grown proteins that mimic or enhance the immune system's response to fight off pathogens, like viruses, and they've been used to treat cancer. Now they are being used to treat patients with COVID-19.
President Donald Trump received a monoclonal antibody cocktail, called REGEN-COV2, which later received FDA emergency use authorization.
A newer type of monoclonal antibody therapy is Antibody-Drug Conjugates, also called ADCs. It's something we're going to be hearing a lot about in 2021, Auclair says.
"Antibody-Drug Conjugates is a monoclonal antibody with a chemical, we consider it a chemical warhead on it," Auclair says. "The monoclonal antibody binds to a specific antigen in your body or protein and delivers a chemical to that location and kills the infected cell."
Moving Beyond Male-Centric Lab Testing
Scientific testing for biology has, until recently, focused on testing males. Dulac, a Howard Hughes Medical Investigator and professor of molecular and cellular biology at Harvard University, challenged that idea to find brain circuitry behind sex-specific behaviors.
"For the longest time, until now, all the model systems in biology, are male," Dulac says. "The idea is if you do testing on males, you don't need to do testing on females."
Clinical models are done in male animals, as well as fundamental research. Because biological research is always done on male models, Dulac says the outcomes and understanding in biology is geared towards understanding male biology.
"All the drugs currently on the market and diagnoses of diseases are biased towards the understanding of male biology," Dulac says. "The diagnostics of diseases is way weaker in women than men."
That means the treatment isn't necessarily as good for women as men, she says, including what is known and understood about pain medication.
"So pain medication doesn't work well in women," Dulac says. "It works way better in men. It's true for almost all diseases that I know. Why? because you have a science that is dominated by males."
Although some in the scientific community challenge that females are not interesting or too complicated with their hormonal variations, Dulac says that's simply not true.
"There's absolutely no reason to decide 50% of life forms are interesting and the other 50% are not interesting. What about looking at both?" says Dulac, who was awarded the $3 million Breakthrough Prize in Life Sciences in September for connecting specific neural mechanisms to male and female parenting behaviors.
Disease Research on Single Cells
To better understand how diseases manifest in the body's cell and tissues, many researchers are looking at single-cell biology. Cells are the most fundamental building blocks of life. Much still needs to be learned.
"A remarkable development this year is the massive use of analysis of gene expression and chromosomal regulation at the single-cell level," Dulac says.
Much is focused on the Human Cell Atlas (HCA), a global initiative to map all cells in healthy humans and to better identify which genes associated with diseases are active in a person's body. Most estimates put the number of cells around 30 trillion.
Dulac points to work being conducted by the Cell Census Network (BICCN) Brain Initiative, an initiative by the National Institutes of Health to come up with an atlas of cell types in mouse, human and non-human primate brains, and the Chan Zuckerberg Initiative's funding of single-cell biology projects, including those focused on single-cell analysis of inflammation.
"Our body and our brain are made of a large number of cell types," Dulac says. "The ability to explore and identify differences in gene expression and regulation in massively multiplex ways by analyzing millions of cells is extraordinarily important."
Converting Plastics into Food
Yep, you heard it right, plastics may eventually be turned into food. The Defense Advanced Research Projects Agency, better known as DARPA, is funding a project—formally titled "Production of Macronutrients from Thermally Oxo-Degraded Wastes"—and asking researchers how to do this.
"When I first heard about this challenge, I thought it was absolutely absurd," says Dr. Robert Brown, director of the Bioeconomy Institute at Iowa State University and the project's principal investigator, who is working with other research partners at the University of Delaware, Sandia National Laboratories, and the American Institute of Chemical Engineering (AIChE)/RAPID Institute.
But then Brown realized plastics will slowly start oxidizing—taking in oxygen—and microorganisms can then consume it. The oxidation process at room temperature is extremely slow, however, which makes plastics essentially not biodegradable, Brown says.
That changes when heat is applied at brick pizza oven-like temperatures around 900-degrees Fahrenheit. The high temperatures get compounds to oxidize rapidly. Plastics are synthetic polymers made from petroleum—large molecules formed by linking many molecules together in a chain. Heated, these polymers will melt and crack into smaller molecules, causing them to vaporize in a process called devolatilization. Air is then used to cause oxidation in plastics and produce oxygenated compounds—fatty acids and alcohols—that microorganisms will eat and grow into single-cell proteins that can be used as an ingredient or substitute in protein-rich foods.
"The caveat is the microorganisms must be food-safe, something that we can consume," Brown says. "Like supplemental or nutritional yeast, like we use to brew beer and to make bread or is used in Australia to make Vegemite."
What do the microorganisms look like? For any home beer brewers, it's the "gunky looking stuff you'd find at the bottom after the fermentation process," Brown says. "That's cellular biomass. Like corn grown in the field, yeast or other microorganisms like bacteria can be harvested as macro-nutrients."
Brown says DARPA's ReSource program has challenged all the project researchers to find ways for microorganisms to consume any plastics found in the waste stream coming out of a military expeditionary force, including all the packaging of food and supplies. Then the researchers aim to remake the plastic waste into products soldiers can use, including food. The project is in the first of three phases.
"We are talking about polyethylene, polypropylene, like PET plastics used in water bottles and converting that into macronutrients that are food," says Brown.
Renewed Focus on Climate Change
The Union of Concerned Scientists say carbon dioxide levels are higher today than any point in at least 800,000 years.
"Climate science is so important for all of humankind. It is critical because the quality of life of humans on the planet depends on it."
Look for technology to help locate large-scale emitters of carbon dioxide, including sensors on satellites and artificial intelligence to optimize energy usage, especially in data centers.
Other technologies focus on alleviating the root cause of climate change: emissions of heat-trapping gasses that mainly come from burning fossil fuels.
Direct air carbon capture, an emerging effort to capture carbon dioxide directly from ambient air, could play a role.
The technology is in the early stages of development and still highly uncertain, says Peter Frumhoff, director of science and policy at Union of Concerned Scientists. "There are a lot of questions about how to do that at sufficiently low costs...and how to scale it up so you can get carbon dioxide stored in the right way," he says, and it can be very energy intensive.
One of the oldest solutions is planting new forests, or restoring old ones, which can help convert carbon dioxide into oxygen through photosynthesis. Hence the Trillion Trees Initiative launched by the World Economic Forum. Trees are only part of the solution, because planting trees isn't enough on its own, Frumhoff says. That's especially true, since 2020 was the year that human-made, artificial stuff now outweighs all life on earth.
More research is also going into artificial photosynthesis for solar fuels. The U.S. Department of Energy awarded $100 million in 2020 to two entities that are conducting research. Look also for improvements in battery storage capacity to help electric vehicles, as well as back-up power sources for solar and wind power, Frumhoff says.
Another method to combat climate change is solar geoengineering, also called solar radiation management, which reflects sunlight back to space. The idea stems from a volcanic eruption in 1991 that released a tremendous amount of sulfate aerosol particles into the stratosphere, reflecting the sunlight away from Earth. The planet cooled by a half degree for nearly a year, Frumhoff says. However, he acknowledges, "there's a lot of things we don't know about the potential impacts and risks" involved in this controversial approach.
Whatever the approach, scientific solutions to climate change are attracting renewed attention. Under President Trump, the White House Office of Science and Technology Policy didn't have an acting director for almost two years. Expect that to change when President-elect Joe Biden takes office.
"Climate science is so important for all of humankind," Dulac says. "It is critical because the quality of life of humans on the planet depends on it."
Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.
Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
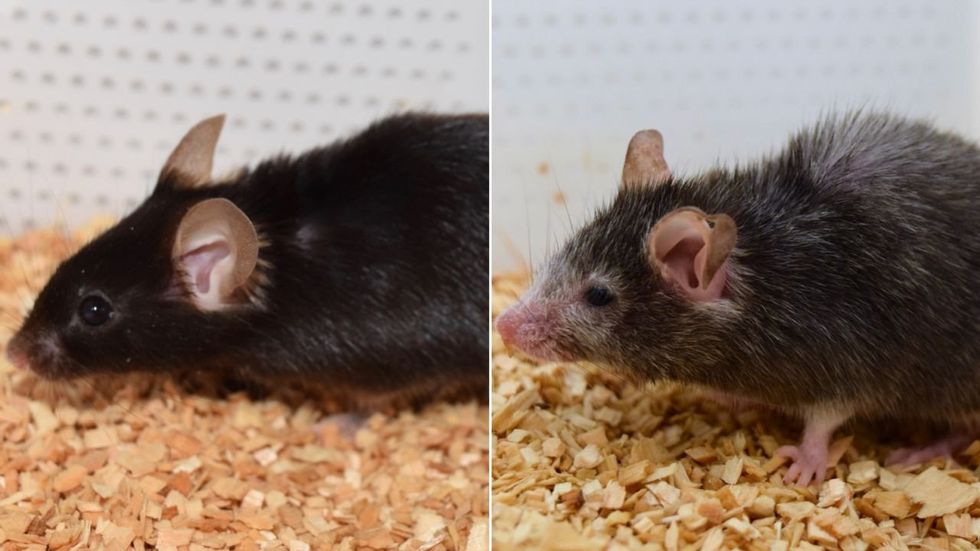
Last month, a paper published in Cell by Harvard biologist David Sinclair explored root cause of aging, as well as examining whether this process can be controlled. We talked with Dr. Sinclair about this new research.
What causes aging? In a paper published last month, Dr. David Sinclair, Professor in the Department of Genetics at Harvard Medical School, reports that he and his co-authors have found the answer. Harnessing this knowledge, Dr. Sinclair was able to reverse this process, making mice younger, according to the study published in the journal Cell.
I talked with Dr. Sinclair about his new study for the latest episode of Making Sense of Science. Turning back the clock on mouse age through what’s called epigenetic reprogramming – and understanding why animals get older in the first place – are key steps toward finding therapies for healthier aging in humans. We also talked about questions that have been raised about the research.
Show links:
Dr. Sinclair's paper, published last month in Cell.
Recent pre-print paper - not yet peer reviewed - showing that mice treated with Yamanaka factors lived longer than the control group.
Dr. Sinclair's podcast.
Previous research on aging and DNA mutations.
Dr. Sinclair's book, Lifespan.

Harvard Medical School

