Elizabeth Holmes Through the Director’s Lens
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Elizabeth Holmes.
"The Inventor," a chronicle of Theranos's storied downfall, premiered recently on HBO. Leapsmag reached out to director Alex Gibney, whom The New York Times has called "one of America's most successful and prolific documentary filmmakers," for his perspective on Elizabeth Holmes and the world she inhabited.
Do you think Elizabeth Holmes was a charismatic sociopath from the start — or is she someone who had good intentions, over-promised, and began the lies to keep her business afloat, a "fake it till you make it" entrepreneur like Thomas Edison?
I'm not qualified to say if EH was or is a sociopath. I don't think she started Theranos as a scam whose only purpose was to make money. If she had done so, she surely would have taken more money for herself along the way. I do think that she had good intentions and that she, as you say, "began the lies to keep her business afloat." ([Reporter John] Carreyrou's book points out that those lies began early.) I think that the Edison comparison is instructive for a lot of reasons.
First, Edison was the original "fake-it-till-you-make-it" entrepreneur. That puts this kind of behavior in the mainstream of American business. By saying that, I am NOT endorsing the ethic, just the opposite. As one Enron executive mused about the mendacity there, "Was it fraud or was it bad marketing?" That gives you a sense of how baked-in the "fake it" sensibility is.
"Having a thirst for fame and a noble cause enabled her to think it was OK to lie in service of those goals."
I think EH shares one other thing with Edison, which is a huge ego coupled with a talent for storytelling as long as she is the heroic, larger-than-life main character. It's interesting that EH calls her initial device "Edison." Edison was the world's most famous "inventor," both because of the devices that came out of his shop and and for his ability for "self-invention." As Randall Stross notes in "The Wizard of Menlo Park," he was the first celebrity businessman. In addition to her "good intentions," EH was certainly motivated by fame and glory and many of her lies were in service to those goals.
Having a thirst for fame and a noble cause enabled her to think it was OK to lie in service of those goals. That doesn't excuse the lies. But those noble goals may have allowed EH to excuse them for herself or, more perniciously, to make believe that they weren't lies at all. This is where we get into scary psychological territory.
But rather than thinking of it as freakish, I think it's more productive to think of it as an exaggeration of the way we all lie to others and to ourselves. That's the point of including the Dan Ariely experiment with the dice. In that experiment, most of the subjects cheated more when they thought they were doing it for a good cause. Even more disturbing, that "good cause" allowed them to lie much more effectively because they had come to believe they weren't doing anything wrong. As it turns out, economics isn't a rational practice; it's the practice of rationalizing.
Where EH and Edison differ is that Edison had a firm grip on reality. He knew he could find a way to make the incandescent lightbulb work. There is no evidence that EH was close to making her "Edison" work. But rather than face reality (and possibly adjust her goals) she pretended that her dream was real. That kind of "over-promising" or "bold vision" is one thing when you are making a prototype in the lab. It's a far more serious matter when you are using a deeply flawed system on real patients. EH can tell herself that she had to do that (Walgreens was ready to walk away if she hadn't "gone live") or else Theranos would have run out of money.
But look at the calculation she made: she thought it was worth putting lives at risk in order to make her dream come true. Now we're getting into the realm of the sociopath. But my experience leads me to believe that -- as in the case of the Milgram experiment -- most people don't do terrible things right away, they come to crimes gradually as they become more comfortable with bigger and bigger rationalizations. At Theranos, the more valuable the company became, the bigger grew the lies.
The two whistleblowers come across as courageous heroes, going up against the powerful and intimidating company. The contrast between their youth and lack of power and the old elite backers of Theronos is staggering, and yet justice triumphed. Were the whistleblowers hesitant or afraid to appear in the film, or were they eager to share their stories?
By the time I got to them, they were willing and eager to tell their stories, once I convinced them that I would honor their testimony. In the case of Erika and Tyler, they were nudged to participate by John Carreyrou, in whom they had enormous trust.
"It's simply crazy that no one demanded to see an objective demonstration of the magic box."
Why do you think so many elite veterans of politics and venture capitalism succumbed to Holmes' narrative in the first place, without checking into the details of its technology or financials?
The reasons are all in the film. First, Channing Robertson and many of the old men on her board were clearly charmed by her and maybe attracted to her. They may have rationalized their attraction by convincing themselves it was for a good cause! Second, as Dan Ariely tells us, we all respond to stories -- more than graphs and data -- because they stir us emotionally. EH was a great storyteller. Third, the story of her as a female inventor and entrepreneur in male-dominated Silicon Valley is a tale that they wanted to invest in.
There may have been other factors. EH was very clever about the way she put together an ensemble of credibility. How could Channing Robertson, George Shultz, Henry Kissinger and Jim Mattis all be wrong? And when Walgreens put the Wellness Centers in stores, investors like Rupert Murdoch assumed that Walgreens must have done its due diligence. But they hadn't!
It's simply crazy that no one demanded to see an objective demonstration of the magic box. But that blind faith, as it turns out, is more a part of capitalism than we have been taught.
Do you think that Roger Parloff deserves any blame for the glowing Fortune story on Theranos, since he appears in the film to blame himself? Or was he just one more victim of Theranos's fraud?
He put her on the cover of Fortune so he deserves some blame for the fraud. He still blames himself. That willingness to hold himself to account shows how seriously he takes the job of a journalist. Unlike Elizabeth, Roger has the honesty and moral integrity to admit that he made a mistake. He owned up to it and published a mea culpa. That said, Roger was also a victim because Elizabeth lied to him.
Do you think investors in Silicon Valley, with their FOMO attitudes and deep pockets, are vulnerable to making the same mistake again with a shiny new startup, or has this saga been a sober reminder to do their due diligence first?
Many of the mistakes made with Theranos were the same mistakes made with Enron. We must learn to recognize that we are, by nature, trusting souls. Knowing that should lead us to a guiding slogan: "trust but verify."
The irony of Holmes dancing to "I Can't Touch This" is almost too perfect. How did you find that footage?
It was leaked to us.
"Elizabeth Holmes is now famous for her fraud. Who better to host the re-boot of 'The Apprentice.'"
Holmes is facing up to 20 years in prison for federal fraud charges, but Vanity Fair recently reported that she is seeking redemption, taking meetings with filmmakers for a possible documentary to share her "real" story. What do you think will become of Holmes in the long run?
It's usually a mistake to handicap a trial. My guess is that she will be convicted and do some prison time. But maybe she can convince jurors -- the way she convinced journalists, her board, and her investors -- that, on account of her noble intentions, she deserves to be found not guilty. "Somewhere, over the rainbow…"
After the trial, and possibly prison, I'm sure that EH will use her supporters (like Tim Draper) to find a way to use the virtual currency of her celebrity to rebrand herself and launch something new. Fitzgerald famously said that "there are no second acts in American lives." That may be the stupidest thing he ever said.
Donald Trump failed at virtually every business he ever embarked on. But he became a celebrity for being a fake businessman and used that celebrity -- and phony expertise -- to become president of the United States. Elizabeth Holmes is now famous for her fraud. Who better to host the re-boot of "The Apprentice." And then?
"You Can't Touch This!"
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
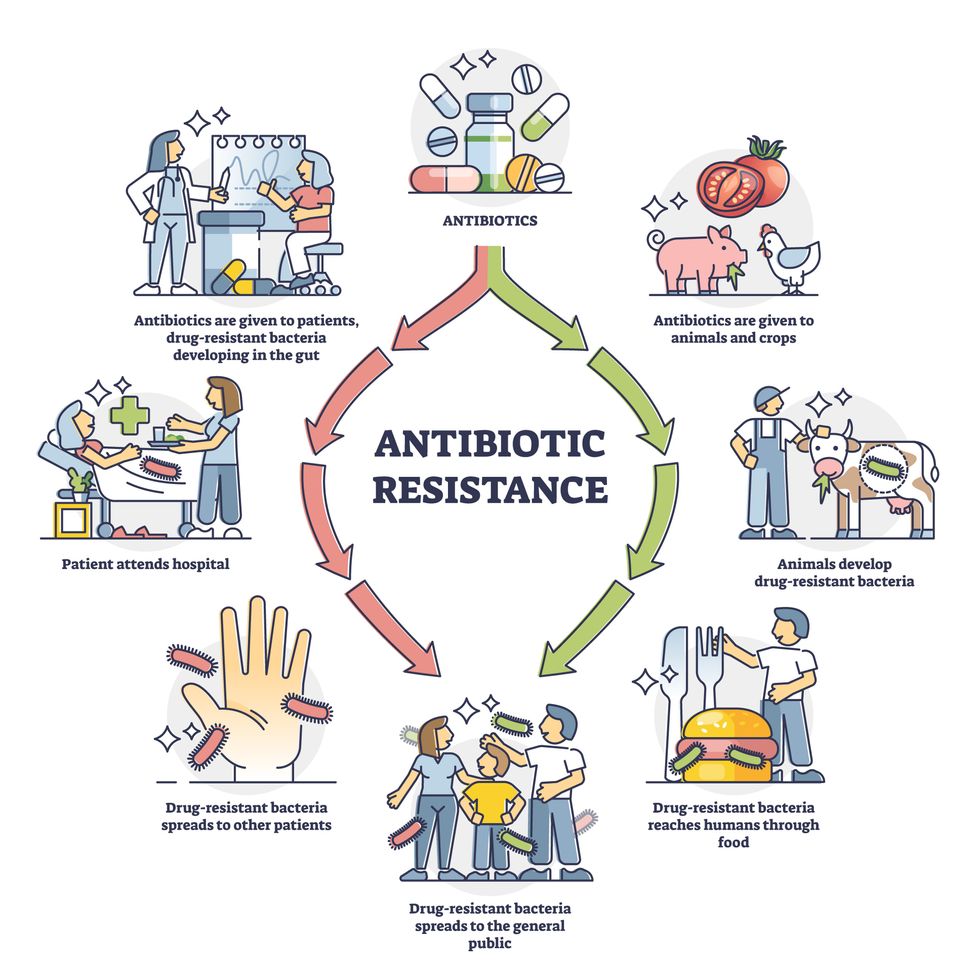
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”
Meet Dr. Renee Wegrzyn, the first Director of President Biden's new health agency, ARPA-H
Today's podcast guest, Dr. Renee Wegrzyn, directs ARPA-H, a new agency formed last year to spearhead health innovations. Time will tell if ARPA-H will produce advances on the level of its fellow agency, DARPA.
In today’s podcast episode, I talk with Renee Wegrzyn, appointed by President Biden as the first director of a health agency created last year, the Advanced Research Projects Agency for Health, or ARPA-H. It’s inspired by DARPA, the agency that develops innovations for the Defense department and has been credited with hatching world-changing technologies such as ARPANET, which became the internet.
Time will tell if ARPA-H will lead to similar achievements in the realm of health. That’s what President Biden and Congress expect in return for funding ARPA-H at 2.5 billion dollars over three years.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
How will the agency figure out which projects to take on, especially with so many patient advocates for different diseases demanding moonshot funding for rapid progress?
I talked with Dr. Wegrzyn about the opportunities and challenges, what lessons ARPA-H is borrowing from Operation Warp Speed, how she decided on the first ARPA-H project that was announced recently, why a separate agency was needed instead of reforming HHS and the National Institutes of Health to be better at innovation, and how ARPA-H will make progress on disease prevention in addition to treatments for cancer, Alzheimer’s and diabetes, among many other health priorities.
Dr. Wegrzyn’s resume leaves no doubt of her suitability for this role. She was a program manager at DARPA where she focused on applying gene editing and synthetic biology to the goal of improving biosecurity. For her work there, she received the Superior Public Service Medal and, in case that wasn’t enough ARPA experience, she also worked at another ARPA that leads advanced projects in intelligence, called I-ARPA. Before that, she ran technical teams in the private sector working on gene therapies and disease diagnostics, among other areas. She has been a vice president of business development at Gingko Bioworks and headed innovation at Concentric by Gingko. Her training and education includes a PhD and undergraduate degree in applied biology from the Georgia Institute of Technology and she did her postdoc as an Alexander von Humboldt Fellow in Heidelberg, Germany.
Dr. Wegrzyn told me that she’s “in the hot seat.” The pressure is on for ARPA-H especially after the need and potential for health innovation was spot lit by the pandemic and the unprecedented speed of vaccine development. We'll soon find out if ARPA-H can produce gamechangers in health that are equivalent to DARPA’s creation of the internet.
Show links:
ARPA-H - https://arpa-h.gov/
Dr. Wegrzyn profile - https://arpa-h.gov/people/renee-wegrzyn/
Dr. Wegrzyn Twitter - https://twitter.com/rwegrzyn?lang=en
President Biden Announces Dr. Wegrzyn's appointment - https://www.whitehouse.gov/briefing-room/statement...
Leaps.org coverage of ARPA-H - https://leaps.org/arpa/
ARPA-H program for joints to heal themselves - https://arpa-h.gov/news/nitro/ -
ARPA-H virtual talent search - https://arpa-h.gov/news/aco-talent-search/

Dr. Renee Wegrzyn was appointed director of ARPA-H last October.