EXCLUSIVE: The World's First Known Person Who Naturally Beat HIV Goes Public

Loreen Willenberg in her home office in Sacramento in May 2019, wearing the pendant with contact information for donating her body to research.
"You better get your things in order, you probably have about six months to live," the nurse told Loreen Willenberg upon returning test results that showed she was HIV-positive in July 1992.
The test measures antibodies to the virus that the immune system develops several weeks after initial infection. The nurse's words were standard advice at the time, when the epidemic was at its worst in the U.S. and effective treatment was still years away. They created "this emotional fear that I was going to die," which would take years to dissipate in Loreen's mind.
Loreen has not benefited from those drugs; remarkably, she has not had to.
The plague had arrived quietly; only a portion of those infected with the virus show flu-like symptoms when first exposed, and soon even those go away. Initially there was no test to detect the virus; it didn't even have a name. But from the moment HIV enters CD4 T cells -- the key helper cells of the immune system -- it slowly, methodically begins to wipe them out until after several years or even a decade, the body lays vulnerable to a panoply of diseases that a fully functioning immune system might fight off with ease.
The quiet phase of the epidemic had passed by the time Loreen received her test results in 1992. Healthy young men would wither to cadaverous forms wracked with disease over the course of just a few months after an AIDS diagnosis but years after they had become infected. They filled half the beds in San Francisco General Hospital. AIDS had become the leading cause of death of young men in the United States, more than 50,000 that year alone. And so a diagnosis was seen as a death sentence.
Stigma accompanied the disease because it was so prevalent among gay men. Many of the sick were disowned and abandoned by their families. Countless AIDS deaths were attributed to other causes to shield the deceased or their families from shame.
Loreen had taken that same test earlier, in 1988, and it had come back negative. Now, after ending an engagement and considering dating again, she had taken the HIV test a second time. The positive results filled her with terror.
The ensuing 27 years have seen a complete change in the epidemic and in Loreen. The introduction of anti-HIV drugs have allowed patients to rise like Lazarus from their death beds, and better yet, keep them from becoming sick, not just in rich nations but throughout the world.
Loreen has not benefited from those drugs; remarkably, she has not had to. Over the years, she has learned from leading HIV researchers across the nation that her unique immune biology has been able to control the virus naturally.
"Loreen, I can't find any HIV in your body. I've looked high and low and think you might have cleared it," said the voice on the other end of the line. It was April 2011 and the caller was a prominent HIV researcher at the National Institutes of Health (NIH).
"I was astonished. I thought it was just extraordinary," says Loreen in recalling that moment. "And then my curiosity kicked in. It's like, how the hell did that happen. What is the mechanism? For twenty years I've understood that the virus actually blends itself into your DNA, the literal blueprint of life. So to have a researcher tell you that your immune system might have cleared it, just like it was the flu, it's like, that is astonishing."
It was a landmark moment for Loreen in a personal and scientific journey from a fearful, stigmatized, and isolated patient, through learning of her unique immune biology that is able to control the virus, to becoming an educated and empowered research participant whom some leading HIV researchers have come to see as a colleague and peer. Her cells have led to a better understanding of HIV, and perhaps will lead to a cure.
The Secret Patient
Loreen didn't fit neatly into the demographics of the AIDS epidemic of 1992 when she was diagnosed. She wasn't a gay man and she didn't live in San Francisco but several hours away in Placerville, a small town of less than 10,000 people in the foothills of the Sierra Nevadas. The town had been the epicenter of the California gold rush in the mid-1800s but now was little more than a dot on the map halfway between Sacramento and Lake Tahoe.

Loreen on vacation in Las Vegas in 1992, the year of her diagnosis with HIV.
(Photo courtesy of Willenberg)
She was 38, tall at 5'7", with auburn hair down to the middle of her back that the sun would streak red. She had grown up in a tough part of Los Angeles, a self-described surfer girl who dropped out of UCLA after a few months of college at the age of 17. She was a voracious reader, curious about a thousand things.
More than a decade of wandering had landed Loreen in Placerville where she befriended a local horticulturalist who taught her much of the trade and encouraged her to start her own business. By now she had a small crew designing, building, and maintaining landscapes in surrounding communities. She was strong from digging and planting alongside her crew, never asking them to do what she would not do herself.
The HIV test results shook her (she suspects she acquired the virus from her then fiancée) and she responded in her typical fashion, by quietly hunkering down and learning all she could about the still-new disease. She told no one except family and a few close friends, afraid that others might shun her and her business, or even worse. Children with hemophilia and HIV had been barred from school in some parts of the country; one family even had their home firebombed. Secrecy was a must in a small community where tongues could wag.
The first step was to find a physician she could trust. A call to the Project Inform Hotline, an AIDS education group in San Francisco, identified two doctors in private practice who treated HIV in Sacramento, a good hour drive away. The Hotline volunteers would become a lifeline, her first teachers in what would become a lifetime of learning about the disease.
Bruce Cohn was a young internist then in private practice. Working with HIV patients "became kind of the best thing I ever did," he recalled in a recent interview. "Most of these [patients] were my peers who were getting sick, about the same age, and so it was easy to relate. I identified, oh, that could be me, and so there was a lot of personal connection to the patients."
He also was driven by the intellectual challenge. "I got to learn something new every day if I wanted to; it was learning on steroids." First came new ways to treat opportunistic infections that plagued those with a compromised immune system, and later antiviral drugs to treat HIV itself.
He shielded himself emotionally by thinking of it as "aging and dying compressed; everything just got more intense, shorter. Their illness was a sort of crisis. People would get sick and if we treated them effectively they would get better. Not as good as they were before, but better."
When Loreen started seeing Cohn, her CD4 T cells, the part of the immune system that HIV infects and replicates within, were even higher than what one would expect to see in a normal healthy person and many times higher than the low level that then existing guidelines recommended for beginning treatment. In addition, the few available anti-HIV drugs were not very good -- the virus often mutated resistance to them within a year and so they were reserved for a last-ditch effort. She and Cohn decided to draw blood and monitor the level of her CD4s along with her regular primary care. First every three months, then twice a year, she drove down from Placerville to Sacramento.
Loreen would track the results of every laboratory test from her medical care, and later every research visit and procedure. First they filled a 3x5 index card which she hid; later they would be saved on a computer spreadsheet.
"We didn't believe what we were seeing"
The CD4 count in a typical untreated HIV-infected person declines by 30 to 50 cells a year. But Loreen's didn't budge.
"Maybe there was something goofy going on because your T cells aren't heading south like they should," Cohn told her after a few years. He retested Loreen several times to confirm the original diagnosis and each time the lab results came back antibody positive. There was no doubt that she had been exposed to HIV and her immune system had developed a response to the virus.

Dr. Bruce Cohn in 1994.
(Courtesy of Cohn)
He also ran the newer, more sensitive viral load tests when they became available, which measure the level of the virus itself in blood, and he couldn't find any. But Cohn didn't pay that much mind, chalking it up to the insensitivity of those early assays that were available for use in medical care. He followed the guidelines for treatment at the time, which were based on CD4 count, not viral load. The years ticked by and Loreen remained robustly healthy, working with her crew and the plants she adored.
Meanwhile, researchers were poking around at the left end of the bell curve of response to HIV, identifying a group they inelegantly dubbed long-term non-progressors (LTNPs) most of whom would later be referred to as controllers. People respond differently to all diseases. Most fall in the middle of the curve and that average response is used to define the course of the disease, but there are some to either side who progress more and others less rapidly than average. Studying those outliers often yields insights that help to better understand the disease and develop treatments.
An early paper on HIV LTNPs was published in 1995 and caught Cohn's eye. He told Loreen about it on her next visit and suggested that researchers would probably want to study her someday. "We looked for a study for the next seven or eight years," she says.
New anti-HIV drugs began to come to market in developed nations starting in 1996. They would lift the pall of death that surrounded the disease and turn it into a chronic, manageable one. Curbing the stigma and discrimination associated with HIV would be slower to yield.
But the fear kept nagging at Loreen. Her physical health was excellent; mentally she was a wreck, still fearful and anxious that people might find out her secret, and that she might sicken and die. It was compounded by menopause.
Women had a harder time than men dealing with HIV, says Cohn. "It was more shameful, more stigmatizing for them, and they had less support." Most of the early social services and support groups had been built by and for gay men. "Women just didn't have the people to connect with or share their experiences or stories with."
Loreen had found and was accepted into a support group mainly for gay men in Placerville. "They really teased me and said 'you're our token straight white woman.' God bless them. Really." But Loreen remained healthy as other members of the group sickened and dealt with the problems of their medications. Eventually, they felt her experience was so different that she did not belong and asked her to leave the group.
Not fitting the normal patterns of HIV disease carried its own burdens. Loreen calls it "a double stigmatization" of HIV and "alienation from within the community itself." Other controllers would have a similar experience, and simply keep their unusual condition a secret for decades, as the stress built within.
The internal pressures became so great that she left the anchoring rock of her business and literally ran away, moving in quick succession to Idaho, then Dallas, then Los Angeles. Only years later would she realize and acknowledge that she had been looking for a savior, someone to protect her from the stigma and take care of her if she became sick. "I was like a bum magnet, looking for love in all the wrong places... and pretty screwed up in my head." She returned to Placerville and Cohn helped her realize the problems were about relationships, not health. His understanding and an antidepressant helped Loreen break the cycle and get back on track.
Then in the fall of 2004, Loreen spotted a small, boxed ad in the back of POZ, a magazine launched in New York City in 1994 to educate and build a community for people living with HIV. The ad was from the Partners AIDS Research Center at Massachusetts General Hospital in Boston and was looking for LTNPs.
"I broke down in tears because I knew that they were looking for me. I called Dr. Cohn the very next day" to make the arrangements, Loreen recounts. They wanted samples of her blood to run a series of experiments. She was so eager to help that she even paid close to $650 out of her own pocket to have the blood samples drawn by her physician "because I didn't have insurance," and FedExed eleven vials out in November. And then she waited.
The phone call came in mid-February 2005 from Florencia Pereyra, then a research fellow in the Partners lab of Bruce Walker at Harvard University. "Part of the reason that it has taken us so long to get back to you and Dr. Cohn is that we didn't believe what we were seeing," she told Loreen.
"Your cells were resisting close to 60 percent of all those bad guys instead of the typical 20-30 percent."
She asked if Loreen might fly to Boston to donate more blood cells, because cells "flatten out" when they are shipped and the lab needed fresh cells. Oh, and by the way, they had not been able to secure funding to fly her there.
Loreen asked why it was so important? What did they find in her original blood donation? "'We exposed your fighter cells, your immune cells, to different viral proteins,'" she recalls Pereyra saying. "'And your cells were resisting close to 60 percent of all those bad guys instead of the typical 20-30 percent.' That's when it dawned on me that there was something really unique about me." Her immune cells were unusually good at fighting HIV.
She was hooked. And in her innocence and eagerness to help, she began cold calling local AIDS researchers asking if they might spare some cash to fly her to Boston. It came as a splash of cold water to be told that scientists were not just one big happy collaborative family, but rather a highly competitive lot scrambling for a limited amount of research dollars. Loreen now laughs at her early naiveté.
Gut Feeling
But she did learn of a research study in her own backyard at the University of California at Davis and eagerly jumped in as a donor. Most HIV research is done using blood because it is a relatively accessible, inexpensive, and painless window to the dynamics of the disease.
The big drawback is that only a small percentage of the CD4 T cells that become infected and spew out HIV are found in blood; a far larger portion are found in lymphoid tissue in the gut. This makes sense; most germs we are exposed to come through what we eat and drink every day, so the immune system focuses much of its attention to take on those challenges in the gut.
Barbara Shacklett, at UC Davis, was conducting the first major study of the immune response to HIV that looked at what was going on in both blood and gut at the same time. She wanted volunteers to give not just a sample of blood but also have a colonoscopy. A tube would be inserted up the rectum and small pieces of gut tissue would be pinched off from along the colon for scientists to analyze.
Shacklett has a wide-eyed charm and easy laugh that belie three and a half years of HIV research in Paris and later stints in labs in New York and San Francisco. Then, nearly twenty years ago, she set up her own lab at Davis. The study was important and broke new ground in understanding that there are significant differences in how HIV replicates in the gut and the blood; simply looking at blood gave an incomplete picture of the disease.
"Loreen was one of the very first two HIV controllers that we had the opportunity to study. She was a very willing study participant, kind of the perfect study volunteer," Shacklett recalled in a recent conversation in her office. "But behind that, she was very, very interested in the research itself, wanted to read the papers and attend some of the conferences."
Loreen would return a handful of times for procedures that removed well over a hundred tissue samples. She received a $100 honorarium for each visit, something that not all studies provide.
One thing puzzled Shacklett; Loreen didn't have the strong T cell immune response that was seen in other HIV controllers -- it was modest at best. T cells comprise a major part of the adaptive immune response, the body's second line of immune defense against an invading pathogen. When T cells encounter parts of a bacteria or virus they have been trained to identify, they surround it, expand in numbers and secrete chemicals that kill the invaders or the cells that are infected. Once the job is completed and the foe vanquished, there is no sense in wasting energy and T cells, and so the immune system pulls back, reducing the number of T cells and dozing off to await the next time there is a threat.
Perhaps the immune system had done its job so well that HIV was no longer there, and the T cells could afford to relax. Perhaps somehow Loreen's body had found a way to not simply reduce the number of virus but to do the unimaginable and actually purge it. That seemed like a wild hypothesis, barely considered at the time, but as the years passed and additional studies documented just how unusual her immune system was, the hypothesis became less far-fetched.
Looking Inside the "Black Box" for Clues
Bruce Walker, a Harvard doctor and researcher, initially thought that people like Loreen -- whose immune systems could control the virus better than most others -- were extremely rare. Then one day, speaking in New York at a postgraduate course on HIV, he asked if others had seen such patients and was shocked when more than half the doctors raised their hands. "And I went, Oh my God, this is not that rare," he recounted.
Walker is tall and handsome in the manner of Superman's alter ego Clark Kent, complete with square jaw and glasses. The smooth talker's superpower is building collaborations and what many consider to be the premier HIV research center in the world, now called The Ragon Institute, in honor of its principal benefactors. He was the first HIV researcher among the nearly 300 investigators supported by the Howard Hughes Medical Institute, the fifth largest foundation in the world with an endowment of $22.6 billion.
He had been an intern and resident at Massachusetts General Hospital (MGH) in the 1980s when the first AIDS cases began to appear. It shaped his decision to focus on HIV and particularly the search for a vaccine. Early vaccine failures led him back to basic science and particularly to HIV LTNPs, that small portion of the bell curve of infected persons whose immune systems could control the virus better than most other people.
Walker convinced Wall Street financier Mark Schwartz and his wife Lisa to donate $5 million to underwrite a genome-wide association study (GWAS) to try and unlock the genetics of how some people were controlling their HIV infection. Experts at the Massachusetts Institute of Technology (MIT) would collaborate on the effort.
"When I first encountered Loreen, there was a sense that the answer was right there for us to figure out."
That funding paid to fly Loreen to Boston in December 2005, about a year after she had sent in those original vials of blood. It was the first of many times she would meet with Walker. "He invited me into his office to talk, and was so excited to be building this cohort [of LTNPs]. He told me of the difficulties in finding us because we were so healthy. I was told I was participant number 10," she says.
"When I first encountered Loreen, there was a sense that the answer was right there for us to figure out," Walker reminisced. "She harbored the answer, but it was really a black box. And since that first encounter with her, we've gotten now to the point where I believe we understand how she is doing it, and how other people are doing it. And I believe that is something we can act upon."
The GWAS study was a major attempt to figure it out. The surface of immune cells is a messy assemblage of proteins that make up the human leukocyte antigen (HLA) system, which governs immune function. The HLA is genetically determined, so Walker hoped the GWAS study could identify specific genetic variants that were associated with control of HIV infection.
It worked. The analysis identified several genetic variations in the immune system that are strongly associated with control of the virus. But no single HLA is common to all controllers and the presence of specific HLAs does not guarantee that a person can control the virus. As an example, Loreen carries some protective HLA variants but not others. So the match is imperfect. It "only explains 20 to 25 percent" of control, says Walker. "But it pointed us in the direction of these killer cells, cytotoxic T cells [CD8 T cells], being important."
A Powerful Sense of Purpose
That trip to Boston was the first time Loreen had been given a tour of a lab, looked through a microscope, and seen how her cells were being put to use. "A light went off in my brain; I understood what I was seeing. I experienced an epiphany," she recalls. "I really think that was about the time I started to let go of the fear" that had plagued her for 13 years since the HIV diagnosis.
"I was fascinated by the hypothesis of the study and I remember telling Dr. Walker that day, 'you need to find more of us. It is very important that you do and I am going to help you. I don't know exactly how I'm going to do it because I'm still living and hiding as an HIV-positive woman. I'm terrified that I'm going to lose my business if I come out about my status in my highly conservative, small, foothills mountain town.'"
"I promised him then that I am going to do it, I'm going to dedicate the rest of my natural life to the work," she remembers telling Walker. "I'm going to need your help because I don't come from a biomedical background. I'm a landscape designer, I'm a horticulturalist, that's my life. I didn't even finish college." He grinned, and the rest is history.
A few months after that first trip to Boston, driven by a desire to help, Loreen formalized her compulsion into a nonprofit organization she called the Zephyr LTNP Foundation. "Zephyr means the wind from the west," she says. It was the screen name she had hidden behind when she first joined HIV forums on the Internet. She dove into reading the scientific and medical literature.
Zephyr was essentially a one-woman organization where she shared the latest journal articles she found interesting, built a network of fellow HIV controllers, and encouraged them to participate in research. Loreen would spend endless hours on the phone, counseling controllers who felt isolated and alone, helping them to build a positive sense of who they were and what they might contribute.
Learning she had a unique biology that people wanted to study "gave her life some meaning, and that was so awesome," says Cohn, Loreen's personal physician for more than a dozen years as she transitioned into active participation in research studies.
Medical ethics, and particularly the U.S. law known as HIPAA (Health Insurance Portability and Accountability Act of 1996), strictly protects the privacy of patients and study participants. This limits why and how researchers can communicate with those participants. Unfortunately, this also acts as a barrier for people like controllers who feel alone and isolated. Networking and recruiting people for these types of studies is difficult.
Through the public attention she brought to controllers via media coverage and on HIV-oriented websites such as thebody.com, she was able to attract and build a network of controllers and educate them, where researchers might be restricted and generally did not have the money or staff to invest in patient education. That's why they have been so appreciative of Loreen.
"She just completely engaged with us and helped make that early GWAS study possible by basically connecting to people across the country, really in a way serving as a recruiter for us, explaining the study, explaining the importance of it, and getting people to become engaged and contribute blood samples," says Walker.
Travel to research sites and AIDS activism increased to such a tempo for Loreen, every month for one year, that she decided to close her business and reduce her travel burden by moving to Sacramento at the end of 2007. She stitched together a series of part time jobs to pay the bills.
Perhaps the high point of Zephyr was a small conference she organized in the fall of 2009 that brought together a handful of researchers studying controllers and a dozen of these patients from various cities. Never before had so many been in the same room.
Then, in the fall of 2011, Loreen started taking college courses to strengthen her critical thinking on medical research and bioethics, completing two AA degrees with honors in 2017.
Visiting the National Institutes of Health
Loreen is not one for half measures. Soon after her initial trip to Boston, she also joined the HIV cohort at the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH). It follows how the disease progresses in people, how it might affect health more broadly, and possible long-term side effects of the drugs they are on. Visits to the Bethesda, Maryland campus are at least once a year and ongoing. The group also includes 142 LTNPs.
"I think she is a very rare person who is at the tail, the extreme end of the spectrum."
Stephen Migueles is a senior research physician with the cohort and the first of his south Florida family to go to college. As an openly gay man doing his medical residency at Georgetown University Hospital in the early 1990s at the depths of the AIDS epidemic, he was both riveted and terrified by the experience, "struggling to come out and accept myself, my family not accepting me, and then seeing everybody dying. It was a really hard time."
He had wanted to be a doctor ever since he could remember and wasn't particularly interested in research because he didn't think he was smart enough. But during a rotation at NIH he caught the eye of senior staff who convinced him to give it a try; that was 22 years ago. He has advanced in the U.S. Public Health Service to wear the eagle of a naval Captain on his collar. "The NIH feels like a family to me and a place where I can do something meaningful ... advancing the science to help find a cure," he says humbly. In an earlier age he might have become a priest loyally serving his parish.
The raw materials that Migueles and others work with are immune cells residing in the body. Researchers gather them through a procedure called leukapheresis. Blood is drawn off through a needle, fed through tubes into a special machine that spins off about 100 million immune cells, and returns the rest of the depleted blood complex to the body, over the course of several hours. The immune cells are then taken to a lab where they are further divided into specific subsets that are closely studied.

Loreen undergoing a leukopheresis at NIH in November 2009. The machine to the right is separating immune cells from the rest of her blood for further analysis.
(Photo Credit: Bob Roehr)
The procedure always leaves Loreen feeling exhausted for the rest of that day and the next. She came down with the flu early this spring, soon after the last time she went through a leukapheresis. Was it because so many of her immune cells had been siphoned off by the procedure that she was less able to fight off the infection? Researchers claim not, that the cells should replace themselves in a day or two, but the question is not well studied. And just to be safe, most research protocols allow that type of donation only once every three or six months.
Scores of different procedures over the years at various research centers have left Loreen's thin veins so scarred that NIH has stopped asking her to undergo any more leukapheresis for science. They realize she may need ready access to those veins for her own medical care at some point in the future.
Migueles' work focuses on CD8 T cells, "the assassins of the immune system." He says the cells of people who control the virus don't necessarily recognize the virus any better than do others; instead, the cells function better. Typically CD8 T cells surround a CD4 T cell that is infected with HIV, proliferate in numbers, then use a protein called perforin to puncture the outside membrane of the cell, and pour in granzyme B, an enzyme that kills the cell.
Typical progressors don't even do a very good job at the stage of proliferation, he says, while controllers are very efficient at every step of the process. Interestingly, with the HIV vaccine candidates that have been developed, the CD8 cells "proliferate really exuberantly, they load their killing granules very efficiently, but then they can't get them out" and into an infected CD4 cell to kill it. A successful vaccine will have to solve this puzzle.
"I knew from our exchanges before she got here that Loreen was going to be a big personality," says Migueles. "A lot of her questions are very much like, 'what do you think is going on with me?' but there are bigger-picture issues, which always makes it very admirable to me.... She would come back at follow up visits and pull out of her bag a bunch of papers with highlighting, and dog-eared, and notes written, which is a lot like me."
Loreen had found another kindred soul and mentor in Migueles, united in scientific curiosity and a sense of service. It was apparent during her latest visit to NIH in June 2019, when the pair would interrupt and complete each other's sentences just as an old married couple might.
After her initial visit in 2006, Loreen had been back home only about a week when Migueles called again, asking how soon she could come back, a recurring motif in her story. A few months later, she was back at NIH watching in awe as a movie played before her eyes of her own CD8 cells destroying cells infected with HIV. "I was saying things like, wow, this is like science fiction."
Loreen's CD8 cells did that job very well indeed. "I think she is a very rare person who is at the tail, the extreme end of the spectrum," Migueles says. "I don't think she's controlling by a different mechanism, but maybe her CD8s have a little more of a kick earlier on and it helped to really knock things down so much that she just doesn't have a lot of replication competent virus around." Perhaps it's like compounding interest in saving for retirement, where a little bit of difference early on in controlling the virus might have a huge effect down the road.
A Cure?
Then in early 2011, Migueles made the astonishing phone call saying that some of her results suggested she might have actually cleared the virus from her body. He needed Loreen to come back and donate tissue from her gut to see if they could find any HIV lingering there. Loreen didn't have to think twice; she traveled to Bethesda over her birthday for the procedure.
The paper came out in April 2012 in the journal Blood. It was a series of four case studies of unnamed HIV elite controllers, a label affixed to those who are best able to control their virus. Elite controllers comprise less than half of one percent of those infected with HIV. One of Migueles' colleagues had made a heroic effort to find HIV in CD4 T cells taken from Loreen's blood and gut tissue, but couldn't detect any complete virus integrated into the 184 million CD4 T cell genomes sampled.
Migueles didn't explicitly say in the paper that, unlike the other three people in the study, he thought Loreen had completely purged the virus -- he's much too cautious a scientist. He knows the only way to absolutely prove that is through an autopsy looking for traces of the virus in every tissue compartment including her brain. But reading between the lines, it was clear that he believes it is a plausible hypothesis.
Researchers called it a "functional cure" of the disease. Loreen recognized all of the data points as hers.
The paper didn't make much of a splash at the time. Scientists were still reluctant to accept that Timothy Ray Brown, the "Berlin Patient," might have been cured of the infection. Brown had been doing well on anti-HIV drugs until he also developed leukemia, a cancer of the blood system. The treatment for leukemia is a brutal regimen of radiation and chemotherapy, which carries a high rate of mortality, to kill off the immune system and replace it with a bone marrow transplant containing stem cells to grow a replacement immune system.
Previously, researchers had isolated CCR5 as a coreceptor that HIV uses to enter and infect CD4 T cells. They later identified a small group of people who carry a genetic mutation, the delta32 deletion, who do not express the CCR5 receptor on the surface of their cells. As a result, people who carry a double version of this mutation, inherited from both parents, are virtually impervious to HIV infection.
The doctor treating Brown decided to do an experiment. Since he had to replace Brown's immune system in treating the cancer, why not try and do it with a version that might also protect him from HIV? Germany has the world's largest registry of bone marrow donors, but still, among those millions of potential donors, only two were a close enough overall HLA genetic match to use with Brown and also contained the double delta32 mutation he sought.
Brown's leukemia recurred and the series of procedures had to be repeated, but eventually he was declared both cancer free and cured of HIV. Controversy remains over the necessity and importance of various aspects of the treatment. However, over time, the medical community has come to accept that he was the first person to be cured of HIV. Other attempts at similar treatments have not been successful, though some believe the "London Patient," announced in early 2019, might also represent a cure.
But back in 2012, when Migueles' paper came out, the first session of the International AIDS Conference that used the word "cure" was still some months away. So to think that someone might have achieved a cure on her own -- without drugs or any of the other miracles of modern medicine -- was unimaginable to most researchers. Still, the paper has stuck in the back of the minds of several scientists and they mention it in conversation whenever Migueles presents his research at a conference.
Talk of a cure came roaring back this spring in a paper from the Ragon Institute team in Boston. It laid out a topographic map of how the various HIV proteins are linked together. Some nodes contain only a few connections while others contain many more. The simpler nodes can more easily change shape when under attack from the immune system and still carry out their functions, while the more complex nodes are less flexible; they can't mutate and still function. The immune systems of HIV controllers focus their energies on those key connections where the virus can't mutate and don't waste their efforts on less important nodes.
"This is the first time we've been able to differentiate controllers from progressors on the basis of an immunologic parameter," says Walker. "And what's very exciting about that is it's not just that we've made an observation, it's an observation that is actionable, we can now try and replicate that in other people." He acknowledges they still don't understand how some people can do this naturally, and is grappling with how they might stimulate others to do it too.
Then this July, at a big international AIDS conference in Mexico City, Ragon researchers compared the cells of a "San Francisco patient" with another elite controller and found scant evidence of HIV. There were a few fragments of HIV RNA as evidence of past infection, but no complete virus capable of replication. They called it a "functional cure" of the disease. Loreen recognized all of the data points as hers; she was the mislabeled San Francisco patient. But she didn't mind, it meant a few more weeks out of the spotlight leading a normal life.
A "Difficult and Ambiguous Moral Space"
Medical research is based upon the foundation of informed consent, where a volunteer is told of the potential risks and benefits of participating in a study and does so willingly, under no pressure. Loreen became very familiar with this process in reading the informed consent documents for each of the dozen or so studies she has participated in. It sparked a growing interest in bioethics.
Another spark came from the outside. "The Immortal Life of Henrietta Lacks" is a landmark and best selling book by Rebecca Skloot that was published in early 2010. It told the story of a poor black woman who in 1951 unknowingly was the source of cervical cancer cells that were turned into a perpetual cell line (HeLa), which is an important tool used in much of biomedical research to this day. Lacks was never told of or benefited from that contribution before she died. The book dug deep into issues of race, class, and medical ethics that underlay what was once accepted practice, and still resonates today.
An HIV controller Loreen had befriended through the Zephyr Foundation sent her a digital version of the book almost as soon as it came out. But reading on a screen didn't suit her and Loreen purchased a hardcover version, pouring through the chapters and filling them with multiple Post-it notes.
"While my donations (and those from my community) have all been made from an altruistic perspective, I can't help but think that my community has signed away our rights to future compensation (for minimal stipends of $200 or less, depending upon the donation procedure and the institution) for extremely valuable data that may contribute to cures for HIV/AIDS, and other diseases," Loreen wrote Skloot in an email the following year.
"The donors are expected to be 100-percent altruistic, when in fact no one else is 100-percent altruistic."
The book also led Loreen to Mark Yarborough, a bioethicist at UC Davis, who would become a mentor in this area. "Not to demonize, but to a certain extent people are in biomedical research for the money," says Yarborough. The pharmaceutical industry wants to bring lucrative new products to market, researchers want to advance their careers and increasingly to form companies to commercialize their work, and even universities stake a claim to patents from the research.
"The expectation is that the donors will do things entirely out of the goodness of their hearts, when everyone else is in it for very good intentions, but also have a lot of self-interest at stake," he says. "The donors are expected to be 100-percent altruistic, when in fact no one else is 100-percent altruistic."
Yarborough has been impressed with the dedication and work Loreen has done on her own and through the Zephyr Foundation. She has struggled with the question, "If I do have this unique biological characteristic that might make an important contribution to finding a vaccine, a cure, an effective treatment, how do I dare not say yes to anyone and everything?"
"You feel compelled to help. You feel like it would be selfish not to help. But at the same time, it's hey, I'm a human person," Yarborough says. "She was always very measured in the way she described things, but she was struggling with, am I being treated appropriately?...She had a strong sense that she was supposed to be treated in a certain way, but she was unclear what that way was. I think that to this day she remains unclear. I remain unclear as well."
"It's almost like a duty to me," Loreen once said while she was laying in a hospital bed at the NIH during a leukapheresis in 2009. "I'm lying here today and I'm thinking about the 40 million people in the world who are living with HIV and who suffer. Who need the medications, who have the side effects from them. And here I am, basically untouched by it physically. That's why I call it a duty...I'm convinced we're going to beat it."
For the last several years, Yarborough has invited Loreen to speak at a required medical school course in ethics he teaches in a graduate degree program that prepares people for a career in biomedical research: the students include medical and PhD research students and junior faculty. "The room is very quiet when Loreen is speaking because people quickly get caught up in her stories. They value the opportunity to ask her questions and there is good discussion afterwards."
"She comes across very much as a peer, and light years ahead of the students in many ways. [She] has been involved in twelve clinical trials and can give you every publication that her samples have contributed to," he continues. "Whereas these people, even if they are junior faculty, may not have been in their first clinical trial yet. So they view Loreen very much as a peer, as opposed to someone who is not on that equal playing field."

Mark Yarborough, a bioethicist at UC Davis, invites Loreen to speak at a medical school course on research ethics.
(Courtesy Yarborough)
"What stands out for me is just how Loreen is living with the difficult and ambiguous moral space that she is living in," says Yarborough. "And the journey that has been for her, the evolution in her own mind and her own thinking."
Going Public
Loreen had seen the media circus that surrounded Tim Brown when his name was made public in 2010 as the first person to be cured of HIV and she wanted no part of it. "I watched every single thing about Tim Brown and I'm not going there. I don't want to live like Timothy Brown does now. I don't want the attention. I live a very quiet private life, and I like it."
What changed her mind was another call from NIH. Documentary filmmakers were shooting a series that would eventually run in the summer of 2017 on The Discovery Channel as "First In Human: The Trials of Building 10," narrated by the ultimate TV science nerd, "The Big Bang Theory" star Jim Parsons. After much soul-searching, she agreed to be filmed.
But the segment didn't make the final cut, perhaps because Loreen represents a mystery that has not yet been translated into a cure for others. She was disappointed. But a psychological barrier had been crossed and she came to see that telling her story was a way to draw attention to controllers and the contribution they might make to finding a cure and perhaps a preventive vaccine for HIV.
Loreen also came to realize, and more importantly internalize, that she was no longer the same person she was in 1992. She knows through meticulously kept records that over the years she has donated to science more than the equivalent of every drop of blood that courses through her body: 91 billion immune cells through leukapharesis; 371 gut tissue samples gathered through more than a dozen colonoscopies and endoscopies; and countless swabbings, poking, and proddings associated with medical examinations.
Those experiences, plus years of reading scientific journals and going to conferences, engaging with researchers, and educating other controllers, have changed her from a scared patient to an empowered participant in the research process.
Loreen donating blood at her most recent visit to NIH, in June 2019. (Photo Credit: Bob Roehr)

Loreen donating blood at her most recent visit to NIH, in June 2019.
(Photo Credit: Bob Roehr)
She realizes that her life is likely to change after her full story becomes public, as the first known person to actually conquer HIV without any medical intervention. And she is resigned to paying that price to help advance the search for a cure.
Researchers believe they have figured out major pieces, but likely not all, of how Loreen's immune system controls HIV. They have hypotheses of how they might generate this same capacity within others using a therapeutic vaccine. But HIV has proven a wily adversary over the last four decades and their success is not assured.
The one thing they can say for certain is that Loreen will be there by their sides, even after death. She has willed her body to research and wears a pendant around her neck indicating the protocol on how it should be handled, so that Migueles can look in every organ for complete copies of the virus. Then science may finally lay to rest any doubts that her immune system has completely overcome HIV.
[Ed.Note: This article was originally published on October 16, 2019.]
Bobby Brooke Herrera, the co-founder and CEO of e25Bio, demonstrates the company's rapid paper-strip test for detecting the coronavirus.
You're lying in bed late at night, the foggy swirl of the pandemic's 8th month just beginning to fall behind you, when you detect a slight tickle at the back of your throat.
"If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can."
Suddenly fully awake, a jolt of panicked electricity races through your body. Has COVID-19 come for you? In the U.S., answering this simple question is incredibly difficult.
Now, you might have to wait for hours in line in your car to get a test for $100, only to find out your result 10-14 days later -- much too late to matter in stopping an outbreak. Due to such obstacles, a recent report in JAMA Internal Medicine estimated that 9 out of 10 infections in the U.S. are being missed.
But what if you could use a paper strip in the privacy of your own home, like a pregnancy test, and find out if you are contagious in real time?
e25 Bio, a small company in Cambridge, Mass., has already created such a test and it has been sitting on a lab bench, inaccessible, since April. It is an antigen test, which looks for proteins on the outside of a virus, and can deliver results in about 15 minutes. Also like an over-the-counter pregnancy test, e25 envisions its paper strips as a public health screening tool, rather than a definitive diagnostic test. People who see a positive result would be encouraged to then seek out a physician-administered, gold-standard diagnostic test: the more sensitive PCR.
Typically, hospitals and other health facilities rely on PCR tests to diagnose viruses. This test can detect small traces of genetic material that a virus leaves behind in the human body, which tells a clinician that the patient is either actively infected with or recently cleared that virus. PCR is quite sensitive, meaning that it is able to detect the presence of a virus' genetic material very accurately.
But although PCR is the gold-standard for diagnostics, it's also the most labor-intensive way to test for a virus and takes a relatively long time to produce results. That's not a good match for stopping super-spreader events during an unchecked pandemic. PCR is also not great at identifying the infected people when they are most at risk of potentially transmitting the virus to others.
That's because the viral threshold at which PCR can detect a positive result is so low, that it's actually too sensitive for the purposes of telling whether someone is contagious.
"The majority of time someone is PCR positive, those [genetic] remnants do not indicate transmissible virus," epidemiologist Michael Mina recently Tweeted. "They indicate remnants of a recently cleared infection."
To stop the chain of transmission for COVID-19, he says, "We need a more accurate test than PCR, that turns positive when someone is able to transmit."
In other words, we need a test that is better at detecting whether a person is contagious, as opposed to whether a small amount of virus can be detected in their nose or saliva. This kind of test is especially critical given the research showing that asymptomatic and pre-symptomatic people have high viral loads and are spreading the virus undetected.
The critical question for contagiousness testing, then, is how big a dose of SARS-CoV-2, the virus that causes COVID, does it take to infect most people? Researchers are still actively trying to answer this. As Angela Rasmussen, a coronavirus expert at Columbia University, told STAT: "We don't know the amount that is required to cause an infection, but it seems that it's probably not a really, really small amount, like measles."
Amesh Adalja, an infectious disease physician and a senior scholar at the Johns Hopkins University Center for Health Security, told LeapsMag: "It's still unclear what viral load is associated with contagiousness but it is biologically plausible that higher viral loads, in general, are associated with more efficient transmission especially in symptomatic individuals. In those without symptoms, however, the same relationship may not hold and this may be one of the reasons young children, despite their high viral loads, are not driving outbreaks."
"Antigen tests work best when there's high viral loads. They're catching people who are super spreaders."
Mina and colleagues estimate that widespread use of weekly cheap, rapid tests that are 100 times less sensitive than PCR tests would prevent outbreaks -- as long as the people who are positive self-isolate.
So why can't we buy e25Bio's test at a drugstore right now? Ironically, it's barred for the very reason that it's useful in the first place: Because it is not sensitive enough to satisfy the U.S. Food and Drug Administration, according to the company.
"We're ready to go," says Carlos-Henri Ferré, senior associate of operations and communications at e25. "We've applied to FDA, and now it's in their hands."
The problem, he said, is that the FDA is evaluating applications for antigen tests based on criteria for assessing diagnostics, like PCR, even when the tests serve a different purpose -- as a screening tool.
"Antigen tests work best when there's high viral loads," Ferré says. "They're catching people who are super spreaders, that are capable of continuing the spread of disease … FDA criteria is for diagnostics and not this."
FDA released guidance on July 29th -- 140 days into the pandemic -- recommending that at-home tests should perform with at least 80 percent sensitivity if ordered by prescription, and at least 90 percent sensitivity if purchased over the counter. "The danger of a false negative result is that it can contribute to the spread of COVID-19," according to an FDA spokesperson. "However, oversight of a health care professional who reviews the results, in combination with the patient's symptoms and uses their clinical judgment to recommend additional testing, if needed, among other things, can help mitigate some risks."
Crucially, the 90 percent sensitivity recommendation is judged upon comparison to PCR tests, meaning that if a PCR test is able to detect virus in 100 samples, the at-home antigen test would need to detect virus in at least 90 of those samples. Since antigen tests only detect high viral loads, frustrated critics like Mina say that such guidance is "unreasonable."
"The FDA at this moment is not understanding the true potential for wide-scale frequent testing. In some ways this is not their fault," Mina told LeapsMag. "The FDA does not have any remit to evaluate tests that fall outside of medical diagnostic testing. The proposal I have put forth is not about diagnostic testing (leave that for symptomatic cases reporting to their physician and getting PCR tests)....Daily rapid tests are not about diagnosing people and they are not about public health surveillance and they are not about passports to go to school, out to dinner or into the office. They are about reducing population-level transmission given a similar approach as vaccines."
A reasonable standard, he added, would be to follow the World Health Organization's Target Product Profiles, which are documents to help developers build desirable and minimally acceptable testing products. "A decent limit," Mina says, "is a 70% or 80% sensitivity (if they truly require sensitivity as a metric) to detect virus at Ct values less than 25. This coincides with detection of the most transmissible people, which is important."
(A Ct value is a type of measurement that corresponds inversely to the amount of viral load in a given sample. Researchers have found that Ct values of 13-17 indicate high viral load, whereas Ct values greater than 34 indicate a lack of infectious virus.)
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics."
"We believe that population screening devices have an immediate place and use in helping beat the virus," says Ferré. "You can have a significant impact even with a test at 60% sensitivity if you are testing frequently."
When presented with criticism of its recommendations, the FDA indicated that it will not automatically deny any at-home test that fails to meet the 90 percent sensitivity guidance.
"FDA is always open to alternative proposals from developers, including strategies for serial testing with less sensitive tests," a spokesperson wrote in a statement. "For example, it is possible that overall sensitivity of the strategy could be considered cumulatively rather than based on one-time testing….In the case of a manufacturer with an at-home test that can only detect people with COVID-19 when they have a high viral load, we encourage them to talk with us so we can better understand their test, how they propose to use it, and the validation data they have collected to support that use."
However, the FDA's actions so far conflict with its stated openness. e25 ended up adding a step to the protocol in order to better meet FDA standards for sensitivity, but that extra step—sending samples to a laboratory for results—will undercut the test's ability to work as an at-home screening tool.
"We believe this should be an at-home test, but [if FDA approval comes through] the first rollout is to do this in laboratories, hospitals, and clinics," Ferré says.
According to the FDA, no test developers have approached them with a request for an emergency use authorization that proposes an alternate testing paradigm, such as serial testing, to mitigate test sensitivity below 80 percent.
From a scientific perspective, antigen tests like e25Bio's are not the only horse in the race for a simple rapid test with potential for at-home use. CRISPR technology has long been touted as fertile ground for diagnostics, and in an eerily prescient interview with LeapsMag in November, CRISPR pioneer Feng Zhang spoke of its potential application as an at-home diagnostic for an infectious disease specifically.
"I think in the long run it will be great to see this for, say, at-home disease testing, for influenza and other sorts of important public health [concerns]," he said in the fall. "To be able to get a readout at home, people can potentially quarantine themselves rather than traveling to a hospital and then carrying the risk of spreading that disease to other people as they get to the clinic."
Zhang's company Sherlock Biosciences is now working on scaled-up manufacturing of a test to detect SARS CoV-2. Mammoth Biosciences, which secured funding from the National Institutes of Health's Rapid Acceleration of Diagnostics program, is also working on a CRISPR diagnostic for SARS CoV-2. Both would check the box for rapid testing, but so far not for at-home testing, as they would also require laboratory infrastructure to provide results.
If any at-home tests can clear the regulatory hurdles, they would also need to be manufactured on a large scale and be cheap enough to entice people to actually use them. In the world of at-home diagnostics, pregnancy tests have become the sole mainstream victor because they're simple to use, small to carry, easy to interpret, and costs about seven or eight dollars at any ubiquitous store, like Target or Walmart. By comparison, the at-home COVID collection tests that don't even offer diagnostics—you send away your sample to an external lab—all cost over $100 to take just one time.
For the time being, the only available diagnostics for COVID require a lab or an expensive dedicated machine to process. This disconnect could prolong the world's worst health crisis in a century.
"Daily rapid tests have enormous potential to sever transmission chains and create herd effects similar to herd immunity," Mina says. "We all recognize that vaccines and infections can result in herd immunity when something around half of people are no longer susceptible.
"The same thing exists with these tests. These are the intervention to stop the virus. If half of people choose to use these tests every other day, then we can stop transmission faster than a vaccine can. The technology exists, the theory and mathematics back it up, the epidemiology is sound. There is no reason we are not approaching this as strongly as we would be approaching vaccines."
--Additional reporting by Julia Sklar
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Coronavirus Risk Calculators: What You Need to Know
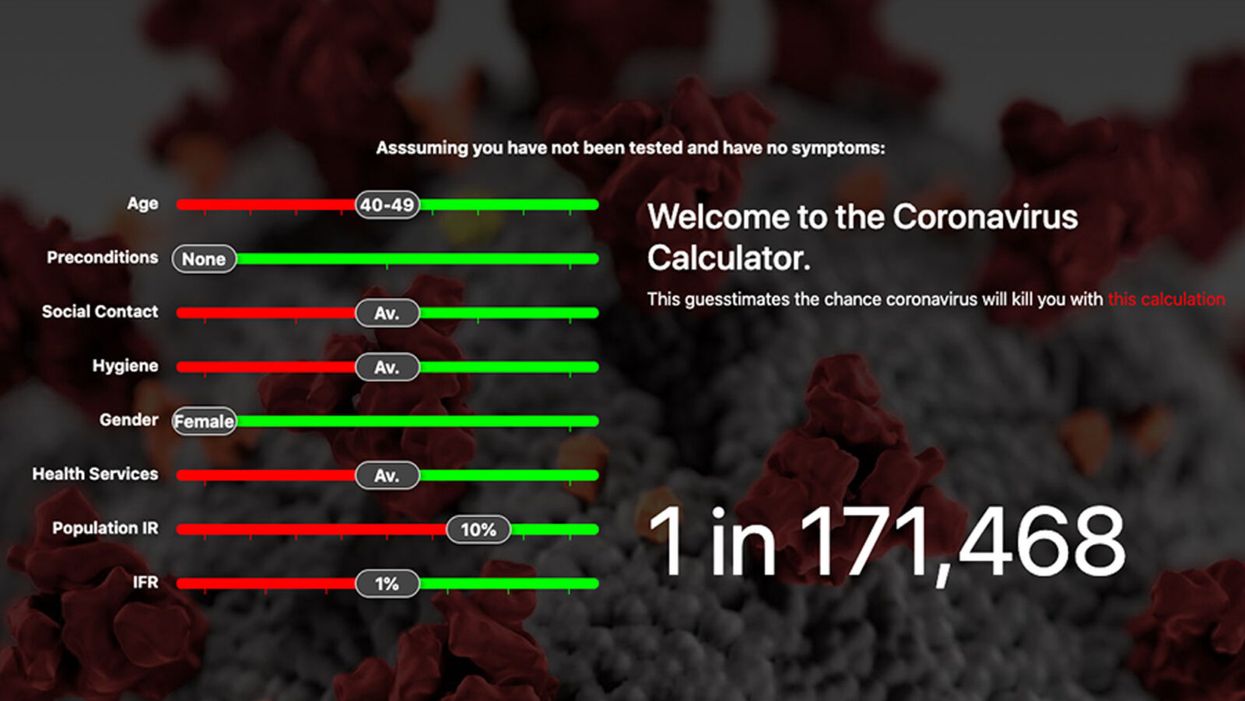
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.