Researchers advance drugs that treat pain without addiction
New therapies are using creative approaches that target the body’s sensory neurons, which send pain signals to the brain.
Opioids are one of the most common ways to treat pain. They can be effective but are also highly addictive, an issue that has fueled the ongoing opioid crisis. In 2020, an estimated 2.3 million Americans were dependent on prescription opioids.
Opioids bind to receptors at the end of nerve cells in the brain and body to prevent pain signals. In the process, they trigger endorphins, so the brain constantly craves more. There is a huge risk of addiction in patients using opioids for chronic long-term pain. Even patients using the drugs for acute short-term pain can become dependent on them.
Scientists have been looking for non-addictive drugs to target pain for over 30 years, but their attempts have been largely ineffective. “We desperately need alternatives for pain management,” says Stephen E. Nadeau, a professor of neurology at the University of Florida.
A “dimmer switch” for pain
Paul Blum is a professor of biological sciences at the University of Nebraska. He and his team at Neurocarrus have created a drug called N-001 for acute short-term pain. N-001 is made up of specially engineered bacterial proteins that target the body’s sensory neurons, which send pain signals to the brain. The proteins in N-001 turn down pain signals, but they’re too large to cross the blood-brain barrier, so they don’t trigger the release of endorphins. There is no chance of addiction.
When sensory neurons detect pain, they become overactive and send pain signals to the brain. “We wanted a way to tone down sensory neurons but not turn them off completely,” Blum reveals. The proteins in N-001 act “like a dimmer switch, and that's key because pain is sensation overstimulated.”
Blum spent six years developing the drug. He finally managed to identify two proteins that form what’s called a C2C complex that changes the structure of a subunit of axons, the parts of neurons that transmit electrical signals of pain. Changing the structure reduces pain signaling.
“It will be a long path to get to a successful clinical trial in humans," says Stephen E. Nadeau, professor of neurology at the University of Florida. "But it presents a very novel approach to pain reduction.”
Blum is currently focusing on pain after knee and ankle surgery. Typically, patients are treated with anesthetics for a short time after surgery. But anesthetics usually only last for 4 to 6 hours, and long-term use is toxic. For some, the pain subsides. Others continue to suffer after the anesthetics have worn off and start taking opioids.
N-001 numbs sensation. It lasts for up to 7 days, much longer than any anesthetic. “Our goal is to prolong the time before patients have to start opioids,” Blum says. “The hope is that they can switch from an anesthetic to our drug and thereby decrease the likelihood they're going to take the opioid in the first place.”
Their latest animal trial showed promising results. In mice, N-001 reduced pain-like behaviour by 90 percent compared to the control group. One dose became effective in two hours and lasted a week. A high dose had pain-relieving effects similar to an opioid.
Professor Stephen P. Cohen, director of pain operations at John Hopkins, believes the Neurocarrus approach has potential but highlights the need to go beyond animal testing. “While I think it's promising, it's an uphill battle,” he says. “They have shown some efficacy comparable to opioids, but animal studies don't translate well to people.”
Nadeau, the University of Florida neurologist, agrees. “It will be a long path to get to a successful clinical trial in humans. But it presents a very novel approach to pain reduction.”
Blum is now awaiting approval for phase I clinical trials for acute pain. He also hopes to start testing the drug's effect on chronic pain.
Learning from people who feel no pain
Like Blum, a pharmaceutical company called Vertex is focusing on treating acute pain after surgery. But they’re doing this in a different way, by targeting a sodium channel that plays a critical role in transmitting pain signals.
In 2004, Stephen Waxman, a neurology professor at Yale, led a search for genetic pain anomalies and found that biologically related people who felt no pain despite fractures, burns and even childbirth had mutations in the Nav1.7 sodium channel. Further studies in other families who experienced no pain showed similar mutations in the Nav1.8 sodium channel.
Scientists set out to modify these channels. Many unsuccessful efforts followed, but Vertex has now developed VX-548, a medicine to inhibit Nav1.8. Typically, sodium ions flow through sodium channels to generate rapid changes in voltage which create electrical pulses. When pain is detected, these pulses in the Nav1.8 channel transmit pain signals. VX-548 uses small molecules to inhibit the channel from opening. This blocks the flow of sodium ions and the pain signal. Because Nav1.8 operates only in peripheral nerves, located outside the brain, VX-548 can relieve pain without any risk of addiction.
"Frankly we need drugs for chronic pain more than acute pain," says Waxman.
The team just finished phase II clinical trials for patients following abdominoplasty surgery and bunionectomy surgery.
After abdominoplasty surgery, 76 patients were treated with a high dose of VX-548. Researchers then measured its effectiveness in reducing pain over 48 hours, using the SPID48 scale, in which higher scores are desirable. The score for Vertex’s drug was 110.5 compared to 72.7 in the placebo group, whereas the score for patients taking an opioid was 85.2. The study involving bunionectomy surgery showed positive results as well.
Waxman, who has been at the forefront of studies into Nav1.7 and Nav1.8, believes that Vertex's results are promising, though he highlights the need for further clinical trials.
“Blocking Nav1.8 is an attractive target,” he says. “[Vertex is] studying pain that is relatively simple and uniform, and that's key to having a drug trial that is informative. But the study needs to be replicated and frankly we need drugs for chronic pain more than acute pain. If this is borne out by additional studies, it's one important step in a journey.”
Vertex will be launching phase III trials later this year.
Finding just the right amount of Nerve Growth Factor
Whereas Neurocarrus and Vertex are targeting short-term pain, a company called Levicept is concentrating on relieving chronic osteoarthritis pain. Around 32.5 million Americans suffer from osteoarthritis. Patients commonly take NSAIDs, or non-steroidal anti-inflammatory drugs, but they cannot be taken long-term. Some take opioids but they aren't very effective.
Levicept’s drug, Levi-04, is designed to modify a signaling pathway associated with pain. Nerve Growth Factor (NGF) is a neurotrophin: it’s involved in nerve growth and function. NGF signals by attaching to receptors. In pain there are excess neurotrophins attaching to receptors and activating pain signals.
“What Levi-04 does is it returns the natural equilibrium of neurotrophins,” says Simon Westbrook, the CEO and founder of Levicept. It stabilizes excess neurotrophins so that the NGF pathway does not signal pain. Levi-04 isn't addictive since it works within joints and in nerves outside the brain.
Westbrook was initially involved in creating an anti-NGF molecule for Pfizer called Tanezumab. At first, Tanezumab seemed effective in clinical trials and other companies even started developing their own versions. However, a problem emerged. Tanezumab caused rapidly progressive osteoarthritis, or RPOA, in some patients because it completely removed NGF from the system. NGF is not just involved in pain signalling, it’s also involved in bone growth and maintenance.
Levicept has found a way to modify the NGF pathway without completely removing NGF. They have now finished a small-scale phase I trial mainly designed to test safety rather than efficacy. “We demonstrated that Levi-04 is safe and that it bound to its target, NGF,” says Westbrook. It has not caused RPOA.
Professor Philip Conaghan, director of the Leeds Institute of Rheumatic and Musculoskeletal Medicine, believes that Levi-04 has potential but urges the need for caution. “At this early stage of development, their molecule looks promising for osteoarthritis pain,” he says. “They will have to watch out for RPOA which is a potential problem.”
Westbrook starts phase II trials with 500 patients this summer to check for potential side effects and test the drug’s efficacy.
There is a real push to find an effective alternative to opioids. “We have a lot of work to do,” says Professor Waxman. “But I am confident that we will be able to develop new, much more effective pain therapies.”
Tech-related injuries are becoming more common as many people depend on - and often develop addictions for - smart phones and computers.
In the 1990s, a mysterious virus spread throughout the Massachusetts Institute of Technology Artificial Intelligence Lab—or that’s what the scientists who worked there thought. More of them rubbed their aching forearms and massaged their cricked necks as new computers were introduced to the AI Lab on a floor-by-floor basis. They realized their musculoskeletal issues coincided with the arrival of these new computers—some of which were mounted high up on lab benches in awkward positions—and the hours spent typing on them.
Today, these injuries have become more common in a society awash with smart devices, sleek computers, and other gadgets. And we don’t just get hurt from typing on desktop computers; we’re massaging our sore wrists from hours of texting and Facetiming on phones, especially as they get bigger in size.
In 2007, the first iPhone measured 3.5-inches diagonally, a measurement known as the display size. That’s been nearly doubled by the newest iPhone 13 Pro, which has a 6.7-inch display. Other phones, too, like the Google Pixel 6 and the Samsung Galaxy S22, have bigger screens than their predecessors. Physical therapists and orthopedic surgeons have had to come up with names for a variety of new conditions: selfie elbow, tech neck, texting thumb. Orthopedic surgeon Sonya Sloan says she sees selfie elbow in younger kids and in women more often than men. She hears complaints related to technology once or twice a day.
The addictive quality of smartphones and social media means that people spend more time on their devices, which exacerbates injuries. According to Statista, 68 percent of those surveyed spent over three hours a day on their phone, and almost half spent five to six hours a day. Another report showed that people dedicate a third of their day to checking their phones, while the Media Effects Research Laboratory at Pennsylvania State University has found that bigger screens, ideal for entertainment purposes, immerse their users more than smaller screens. Oversized screens also provide easier navigation and more space for those with bigger hands or trouble seeing.
But others with conditions like arthritis can benefit from smaller phones. In March of 2016, Apple released the iPhone SE with a display size of 4.7 inches—an inch smaller than the iPhone 7, released that September. Apple has since come out with two more versions of the diminutive iPhone SE, one in 2020 and another in 2022.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable?
Kavin Senapathy, a freelance science journalist, has the Google Pixel 6. She was drawn to the phone because Google marketed the Pixel 6’s camera as better at capturing different skin tones. But this phone boasts one of the largest display sizes on the market: 6.4 inches.
Senapathy was diagnosed with carpal and cubital tunnel syndromes in 2017 and fibromyalgia in 2019. She has had to create a curated ergonomic workplace setup, otherwise her wrists and hands get weak and tingly, and she’s had to adjust how she holds her phone to prevent pain flares.
Recently, Senapathy underwent an electromyography, or an EMG, in which doctors insert electrodes into muscles to measure their electrical activity. The electrical response of the muscles tells doctors whether the nerve cells and muscles are successfully communicating. Depending on her results, steroid shots and even surgery might be required. Senapathy wants to stick with her Pixel 6, but the pain she’s experiencing may push her to buy a smaller phone. Unfortunately, options for these modestly sized phones are more limited.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers like Senapathy to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable for creating addictive devices that lead to musculoskeletal injury?

Kavin Senapathy, a freelance journalist, bought the Google Pixel 6 because of its high-quality camera, but she’s had to adjust how she holds the oversized phone to prevent pain flares.
Kavin Senapathy
A one-size-fits-all mentality for smartphones will continue to lead to injuries because every user has different wants and needs. S. Shyam Sundar, the founder of Penn State’s lab on media effects and a communications professor, says the needs for mobility and portability conflict with the desire for greater visibility. “The best thing a company can do is offer different sizes,” he says.
Joanna Bryson, an AI ethics expert and professor at The Hertie School of Governance in Berlin, Germany, echoed these sentiments. “A lot of the lack of choice we see comes from the fact that the markets have consolidated so much,” she says. “We want to make sure there’s sufficient diversity [of products].”
Consumers can still maintain some control despite the ubiquity of tech. Sloan, the orthopedic surgeon, has to pester her son to change his body positioning when using his tablet. Our heads get heavier as they bend forward: at rest, they weigh 12 pounds, but bent 60 degrees, they weigh 60. “I have to tell him, ‘Raise your head, son!’” she says. It’s important, Sloan explains, to consider that growth and development will affect ligaments and bones in the neck, potentially making kids even more vulnerable to injuries from misusing gadgets. She recommends that parents limit their kids’ tech time to alleviate strain. She also suggested that tech companies implement a timer to remind us to change our body positioning.
In 2017, Nan-Wei Gong, a former contractor for Google, founded Figur8, which uses wearable trackers to measure muscle function and joint movement. It’s like physical therapy with biofeedback. “Each unique injury has a different biomarker,” says Gong. “With Figur8, you are comparing yourself to yourself.” This allows an individual to self-monitor for wear and tear and strengthen an injury in a way that’s efficient and designed for their body. Gong noticed that the work-from-home model during the COVID-19 pandemic created a new set of ergonomic problems that resulted in injuries. Figur8 provides real-time data for these injuries because “behavioral change requires feedback.”
Gong worked on a project called Jacquard while at Google. Textile experts weave conductive thread into their fabric, and the result is a patch of the fabric—like the cuff of a Levi’s jacket—that responds to commands on your smartphone. One swipe can call your partner or check the weather. It was designed with cyclists in mind who can’t easily check their phones, and it’s part of a growing movement in the tech industry to deliver creative, hands-free design. Gong thinks that engineers at large corporations like Google have accessibility in mind; it’s part of what drives their decisions for new products.
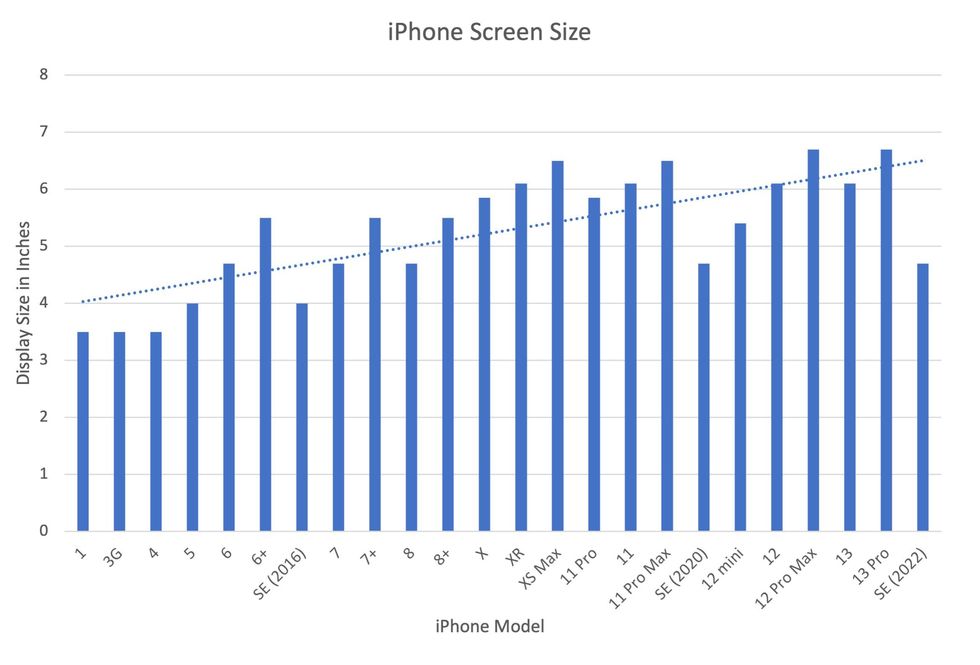
Display sizes of iPhones have become larger over time.
Sourced from Screenrant https://screenrant.com/iphone-apple-release-chronological-order-smartphone/ and Apple Tech Specs: https://www.apple.com/iphone-se/specs/
Back in Germany, Joanna Bryson reminds us that products like smartphones should adhere to best practices. These rules may be especially important for phones and other products with AI that are addictive. Disclosure, accountability, and regulation are important for AI, she says. “The correct balance will keep changing. But we have responsibilities and obligations to each other.” She was on an AI Ethics Council at Google, but the committee was disbanded after only one week due to issues with one of their members.
Bryson was upset about the Council’s dissolution but has faith that other regulatory bodies will prevail. OECD.AI, and international nonprofit, has drafted policies to regulate AI, which countries can sign and implement. “As of July 2021, 46 governments have adhered to the AI principles,” their website reads.
Sundar, the media effects professor, also directs Penn State’s Center for Socially Responsible AI. He says that inclusivity is a crucial aspect of social responsibility and how devices using AI are designed. “We have to go beyond first designing technologies and then making them accessible,” he says. “Instead, we should be considering the issues potentially faced by all different kinds of users before even designing them.”
They received retinal implants to restore their vision. Then the company turned its back on them.
A company called Second Sight made an implant that partially restored vision to people who'd been blind for decades. But when Second Sight pivoted, it stopped servicing its product, leaving many in the dark.
The first thing Jeroen Perk saw after he partially regained his sight nearly a decade ago was the outline of his guide dog Pedro.
“There was a white floor, and the dog was black,” recalls Perk, a 43-year-old investigator for the Dutch customs service. “I was crying. It was a very nice moment.”
Perk was diagnosed with retinitis pigmentosa as a child and had been blind since early adulthood. He has been able to use the implant placed into his retina in 2013 to help identify street crossings, and even ski and pursue archery. A video posted by the company that designed and manufactured the device indicates he’s a good shot.
Less black-and-white has been the journey Perk and others have been on after they were implanted with the Argus II, a second-generation device created by a Los Angeles-based company called Second Sight Medical Devices.
The Argus II uses the implant and a video camera embedded in a special pair of glasses to provide limited vision to those with retinitis pigmentosa, a genetic disease that causes cells in the retina to deteriorate. The camera feeds information to the implant, which sends electrical impulses into the retina to recapitulate what the camera sees. The impulses appear in the Argus II as a 60-pixel grid of blacks, grays and whites in the user’s eye that can render rough outlines of objects and their motion.
Smartphone and computer manufacturers typically stop issuing software upgrades to their devices after two or three years, eventually rendering them bricks. But is the smartphone approach acceptable for a device that helps restore the most crucial sense a human being possesses?
Ross Doerr, a retired disability rights attorney in Maine who received an Argus II in 2019, describes the field of vision as the equivalent of an index card held at arm’s length. Perk often brings objects close to his face to decipher them. Moreover, users must swivel their heads to take in visual data; moving their eyeballs does not work.
Despite its limitations, the Argus II beats the alternative. Perk no longer relies on his guide dog. Doerr was uplifted when he was able to see the outlines of Christmas trees at a holiday show.
“The fairy godmother department sort of reaches out and taps you on the shoulder once in a while,” Doerr says of his implant, which came about purely by chance. A surgeon treating his cataracts was partnered with the son of another surgeon who was implanting the devices, and he was referred.
Doerr had no reason to believe the shower of fairy dust wouldn’t continue. Second Sight held out promises that the Argus II recipients’ vision would gradually improve through upgrades to much higher pixel densities. The ability to recognize individual faces was even touted as a possibility. In the winter of 2020, Doerr was preparing to travel across the U.S. to Second Sight’s headquarters to receive an upgrade. But then COVID-19 descended, and the trip was canceled.
The pandemic also hit Second Sight’s bottom line. Doerr found out about its tribulations only from one of the company’s vision therapists, who told him the entire department was being laid off. Second Sight cut nearly 80% of its workforce in March 2020 and announced it would wind down operations.

Ross Doerr has mostly stopped using his Argus II, the result of combination of fear of losing its assistance from wear and tear and disdain for the company that brought it to market.
Jan Doerr
Second Sight’s implosion left some 350 Argus recipients in the metaphorical dark about what to do if their implants failed. Skeleton staff seem to have rarely responded to queries from their customers, at least based on the experiences of Perk and Doerr. And some recipients have unfortunately returned to the actual dark as well, as reports have surfaced of Argus II failures due to aging or worn-down parts.
Product support for complex products is remarkably uneven. Although the iconic Ford Mustang ceased production in the late 1960s, its parts market is so robust that it’s theoretically possible to assemble a new vehicle from recently crafted components. Conversely, smartphone and computer manufacturers typically stop issuing software upgrades to their devices after two or three years, eventually rendering them bricks. Consumers have accepted both extremes.
But is the smartphone approach acceptable for a device that helps restore the most crucial sense a human being possesses?
Margaret McLean, a senior fellow at the Markkula Center for Applied Ethics at Santa Clara University in California, notes companies like Second Sight have a greater obligation for product support than other consumer product ventures.
“In this particular case, you have a great deal of risk that is involved in using this device, the implant, and the after care of this device,” she says. “You cannot, like with your car, decide that ‘I don’t like my Mustang anymore,’ and go out and buy a Corvette.”
And, whether the Argus II implant works or not, its physical presence can impact critical medical decisions. Doerr’s doctor wanted him to undergo an MRI to assist in diagnosing attacks of vertigo. But the physician was concerned his implant might interfere. With the latest available manufacturer advisories on his implant nearly a decade old, the procedure was held up. Doerr spent months importuning Second Sight through phone calls, emails and Facebook postings to learn if his implant was contraindicated with MRIs, which he never received. Although the cause of his vertigo was found without an MRI, Doerr was hardly assured.
“Put that into context for a minute. I get into a serious car accident. I end up in the emergency room, and I have a tag saying I have an implanted medical device,” he says. “You can’t do an MRI until you get the proper information from the company. Who’s going to answer the phone?”
Second Sight’s management did answer the call to revamp its business. It netted nearly $78 million through a private stock placement and an initial public offering last year. At the end of 2021, Second Sight had nearly $70 million in cash on hand, according to a recent filing with the Securities and Exchange Commission.
And while the Argus II is still touted at length on Second Sight’s home page, it appears little of its corporate coffers are earmarked toward its support. These days, the company is focused on obtaining federal approvals for Orion, a new implant that would go directly into the recipient’s brain and could be used to remedy blindness from a variety of causes. It obtained a $6.4 million grant from the National Institutes of Health in May 2021 to help develop Orion.
Presented with a list of written questions by email, Second Sight’s spokesperson, Dave Gentry of the investor relations firm Red Chip Companies, copied a subordinate with an abrupt message to “please handle.” That was the only response from a company representative. A call to Second Sight acting chief executive officer Scott Dunbar went unreturned.
Whether or not the Orion succeeds remains to be seen. The company’s SEC filings suggest a viable and FDA-approved device is years away, and that operational losses are expected for the “foreseeable future.” Second Sight reported zero revenue in 2020 or 2021.
Moreover, the experiences of the Argus II recipients could color the reception of future Second Sight products. Doerr notes that his insurer paid nearly $500,000 to implant his device and for training on how to use it.
“What’s the insurance industry going to say the next time this crops up?” Doerr asks, noting that the company’s reputation is “completely shot” with the recipients of its implants.
Perk, who made speeches to praise the Argus II and is still featured in a video on the Second Sight website, says he also no longer supports the company.

Jeroen Perk, an investigator for the Dutch customs service, cried for joy after partially regaining his sight, but he no longer trusts Second Sight, the company that provided his implant.
Nanda Perk
Nevertheless, Perk remains highly reliant on the technology. When he dropped an external component of his device in late 2020 and it broke, Perk briefly debated whether to remain blind or find a way to get his Argus II working again. Three months later, he was able to revive it by crowdsourcing parts, primarily from surgeons with spare components or other Argus II recipients who no longer use their devices. Perk now has several spare parts in reserve in case of future breakdowns.
Despite the frantic efforts to retain what little sight he has, Perk has no regrets about having the device implanted. And while he no longer trusts Second Sight, he is looking forward to possibly obtaining more advanced implants from companies in the Netherlands and Australia working on their own products.
Doerr suggests that biotech firms whose implants are distributed globally be bound to some sort of international treaty requiring them to service their products in perpetuity. Such treaties are still applied to the salvage rights for ships that sunk centuries ago, he notes.
“I think that in a global tech economy, that would be a good thing,” says McLean, the fellow at Santa Clara, “but I am not optimistic about it in the near term. Business incentives push toward return on share to stockholders, not to patients and other stakeholders. We likely need to rely on some combination of corporately responsibility…and [international] government regulation. It’s tough—the Paris Climate Accord implementation at a slow walk comes to mind.”
Unlike Perk, Doerr has mostly stopped using his Argus II, the result of combination of fear of losing its assistance from wear and tear and disdain for the company that brought it to market. At 70, Doerr says he does not have the time or energy to hold the company more accountable. And with Second Sight having gone through a considerable corporate reorganization, Doerr believes a lawsuit to compel it to better serve its Argus recipients would be nothing but an extremely costly longshot.
“It’s corporate America at its best,” he observes.


