Doctors worry that fungal pathogens may cause the next pandemic.
Bacterial antibiotic resistance has been a concern in the medical field for several years. Now a new, similar threat is arising: drug-resistant fungal infections. The Centers for Disease Control and Prevention considers antifungal and antimicrobial resistance to be among the world’s greatest public health challenges.
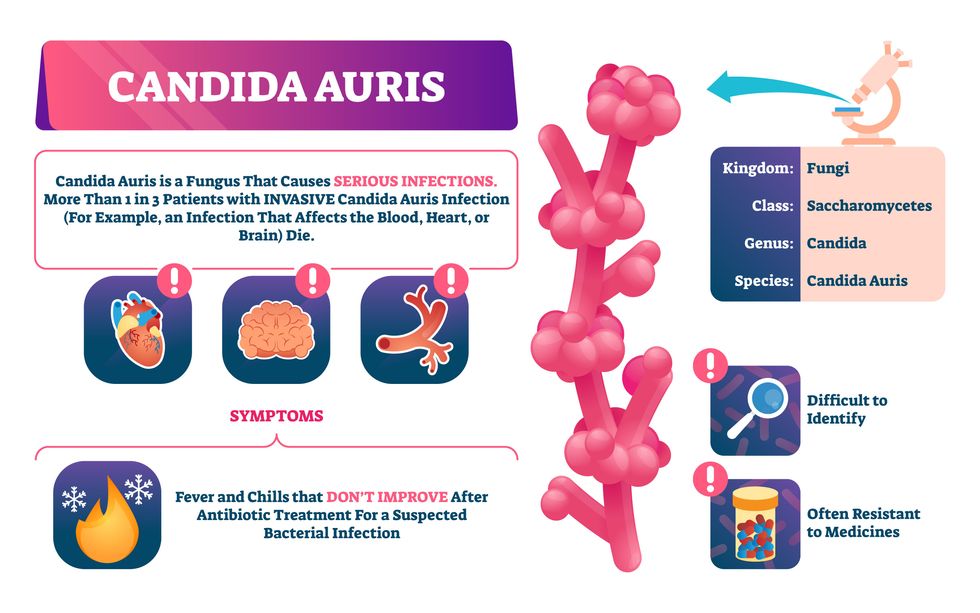
One particular type of fungal infection caused by Candida auris is escalating rapidly throughout the world. And to make matters worse, C. auris is becoming increasingly resistant to current antifungal medications, which means that if you develop a C. auris infection, the drugs your doctor prescribes may not work. “We’re effectively out of medicines,” says Thomas Walsh, founding director of the Center for Innovative Therapeutics and Diagnostics, a translational research center dedicated to solving the antimicrobial resistance problem. Walsh spoke about the challenges at a Demy-Colton Virtual Salon, one in a series of interactive discussions among life science thought leaders.
Although C. auris typically doesn’t sicken healthy people, it afflicts immunocompromised hospital patients and may cause severe infections that can lead to sepsis, a life-threatening condition in which the overwhelmed immune system begins to attack the body’s own organs. Between 30 and 60 percent of patients who contract a C. auris infection die from it, according to the CDC. People who are undergoing stem cell transplants, have catheters or have taken antifungal or antibiotic medicines are at highest risk. “We’re coming to a perfect storm of increasing resistance rates, increasing numbers of immunosuppressed patients worldwide and a bug that is adapting to higher temperatures as the climate changes,” says Prabhavathi Fernandes, chair of the National BioDefense Science Board.
Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures.
Although medical professionals aren’t concerned at this point about C. auris evolving to affect healthy people, they worry that its presence in hospitals can turn routine surgeries into life-threatening calamities. “It’s coming,” says Fernandes. “It’s just a matter of time.”
An emerging global threat
“Fungi are found in the environment,” explains Fernandes, so Candida spores can easily wind up on people’s skin. In hospitals, they can be transferred from contact with healthcare workers or contaminated surfaces. Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures. It can enter the body during medical treatments that break the skin—and cause an infection. Overall, fungal infections cost some $48 billion in the U.S. each year. And infection rates are increasing because, in an ironic twist, advanced medical therapies are enabling severely ill patients to live longer and, therefore, be exposed to this pathogen.
The first-ever case of a C. auris infection was reported in Japan in 2009, although an analysis of Candida samples dated the earliest strain to a 1996 sample from South Korea. Since then, five separate varieties – called clades, which are similar to strains among bacteria – developed independently in different geographies: South Asia, East Asia, South Africa, South America and, recently, Iran. So far, C. auris infections have been reported in 35 countries.
In the U.S., the first infection was reported in 2016, and the CDC started tracking it nationally two years later. During that time, 5,654 cases have been reported to the CDC, which only tracks U.S. data.
What’s more notable than the number of cases is their rate of increase. In 2016, new cases increased by 175 percent and, on average, they have approximately doubled every year. From 2016 through 2022, the number of infections jumped from 63 to 2,377, a roughly 37-fold increase.
“This reminds me of what we saw with epidemics from 2013 through 2020… with Ebola, Zika and the COVID-19 pandemic,” says Robin Robinson, CEO of Spriovas and founding director of the Biomedical Advanced Research and Development Authority (BARDA), which is part of the U.S. Department of Health and Human Services. These epidemics started with a hockey stick trajectory, Robinson says—a gradual growth leading to a sharp spike, just like the shape of a hockey stick.
Another challenge is that right now medics don’t have rapid diagnostic tests for fungal infections. Currently, patients are often misdiagnosed because C. auris resembles several other easily treated fungi. Or they are diagnosed long after the infection begins and is harder to treat.
The problem is that existing diagnostics tests can only identify C. auris once it reaches the bloodstream. Yet, because this pathogen infects bodily tissues first, it should be possible to catch it much earlier before it becomes life-threatening. “We have to diagnose it before it reaches the bloodstream,” Walsh says.
The most alarming fact is that some Candida infections no longer respond to standard therapeutics.
“We need to focus on rapid diagnostic tests that do not rely on a positive blood culture,” says John Sperzel, president and CEO of T2 Biosystems, a company specializing in diagnostics solutions. Blood cultures typically take two to three days for the concentration of Candida to become large enough to detect. The company’s novel test detects about 90 percent of Candida species within three to five hours—thanks to its ability to spot minute quantities of the pathogen in blood samples instead of waiting for them to incubate and proliferate.
Unlike other Candida species C. auris thrives at human body temperatures
Adobe Stock
Tackling the resistance challenge
The most alarming fact is that some Candida infections no longer respond to standard therapeutics. The number of cases that stopped responding to echinocandin, the first-line therapy for most Candida infections, tripled in 2020, according to a study by the CDC.
Now, each of the first four clades shows varying levels of resistance to all three commonly prescribed classes of antifungal medications, such as azoles, echinocandins, and polyenes. For example, 97 percent of infections from C. auris Clade I are resistant to fluconazole, 54 percent to voriconazole and 30 percent of amphotericin. Nearly half are resistant to multiple antifungal drugs. Even with Clade II fungi, which has the least resistance of all the clades, 11 to 14 percent have become resistant to fluconazole.
Anti-fungal therapies typically target specific chemical compounds present on fungi’s cell membranes, but not on human cells—otherwise the medicine would cause damage to our own tissues. Fluconazole and other azole antifungals target a compound called ergosterol, preventing the fungal cells from replicating. Over the years, however, C. auris evolved to resist it, so existing fungal medications don’t work as well anymore.
A newer class of drugs called echinocandins targets a different part of the fungal cell. “The echinocandins – like caspofungin – inhibit (a part of the fungi) involved in making glucan, which is an essential component of the fungal cell wall and is not found in human cells,” Fernandes says. New antifungal treatments are needed, she adds, but there are only a few magic bullets that will hit just the fungus and not the human cells.
Research to fight infections also has been challenged by a lack of government support. That is changing now that BARDA is requesting proposals to develop novel antifungals. “The scope includes C. auris, as well as antifungals following a radiological/nuclear emergency, says BARDA spokesperson Elleen Kane.
The remaining challenge is the number of patients available to participate in clinical trials. Large numbers are needed, but the available patients are quite sick and often die before trials can be completed. Consequently, few biopharmaceutical companies are developing new treatments for C. auris.
ClinicalTrials.gov reports only two drugs in development for invasive C. auris infections—those than can spread throughout the body rather than localize in one particular area, like throat or vaginal infections: ibrexafungerp by Scynexis, Inc., fosmanogepix, by Pfizer.
Scynexis’ ibrexafungerp appears active against C. auris and other emerging, drug-resistant pathogens. The FDA recently approved it as a therapy for vaginal yeast infections and it is undergoing Phase III clinical trials against invasive candidiasis in an attempt to keep the infection from spreading.
“Ibreafungerp is structurally different from other echinocandins,” Fernandes says, because it targets a different part of the fungus. “We’re lucky it has activity against C. auris.”
Pfizer’s fosmanogepix is in Phase II clinical trials for patients with invasive fungal infections caused by multiple Candida species. Results are showing significantly better survival rates for people taking fosmanogepix.
Although C. auris does pose a serious threat to healthcare worldwide, scientists try to stay optimistic—because they recognized the problem early enough, they might have solutions in place before the perfect storm hits. “There is a bit of hope,” says Robinson. “BARDA has finally been able to fund the development of new antifungal agents and, hopefully, this year we can get several new classes of antifungals into development.”
Many children use makeup and body products such as glitter, face paint and lip gloss. Scientists are pointing to the harmful chemicals in some of these products, and advocates are looking to outlaw them.
When Erika Schreder’s 14-year-old daughter, who is Black, had her curly hair braided at a Seattle-area salon two or three times recently, the hairdresser applied a styling gel to seal the tresses in place.
Schreder and her daughter had been trying to avoid harmful chemicals, so they were shocked to later learn that this particular gel had the highest level of formaldehyde of any product tested by the Washington State Departments of Ecology and Health. In January 2023, the agencies released a report that uncovered high levels of formaldehyde in certain hair products, creams and lotions marketed to or used by people of color. When Schreder saw the report, she mentioned it to her daughter, who told her the name of the gel smoothed on her hair.
“It was really upsetting,” said Schreder, science director at Toxic-Free Future, a Seattle-based nonprofit environmental health research and advocacy organization. “Learning that this product used on my daughter’s hair contained cancer-causing formaldehyde made me even more committed to advocating for our state to ban toxic ingredients in cosmetics and personal care products.”
In 2013, Toxic-Free Future launched Mind the Store to challenge the nation’s largest retailers in adopting comprehensive policies that eliminate toxic chemicals in their personal care products and packaging, and develop safer alternatives.
Now, more efforts are underway to expose and mitigate the harm in cosmetics, hair care and other products that children apply on their faces, heads, nails and other body parts. Advocates hope to raise awareness among parents while prompting manufacturers and salon professionals to adopt safer alternatives.
A recent study by researchers at Columbia University Mailman School of Public Health and Earthjustice, a San Francisco-based nonprofit public interest environmental law organization, revealed that most children in the United States use makeup and body products that may contain carcinogens and other toxic chemicals. In January, the results were published in the International Journal of Environmental Research and Public Health. Based on more than 200 surveys, 70 percent of parents in the study reported that their children 12 or younger have used makeup and body products marketed to youth — for instance, glitter, face paint and lip gloss.
Childhood exposure to harmful makeup and body product ingredients can also be considered an environmental justice issue, as communities of color may be more likely to use these products.
“We are concerned about exposure to chemicals that may be found in cosmetics and body products, including those that are marketed toward children,” said the study’s senior author, Julie Herbstman, a professor and director of the Columbia Center for Children's Environmental Health. The goal of the survey was to try to understand how much kids are using cosmetic and body products and when, how and why they are using them.
“There is widespread use of children’s cosmetic and body products, and kids are using them principally to play,” Herbstman said. “That’s really quite different than how adults use cosmetic and body products.” Even with products that are specifically designed for children, “there’s no regulation that ensures that these products are safe for kids.” Also, she said, some children are using adult products — and they may do so in inadvisable ways, such as ingesting lipstick or applying it to other areas of the face.
Earlier research demonstrated that beauty and personal care products manufactured for children and adults frequently contain toxic chemicals, such as lead, asbestos, PFAS, phthalates and formaldehyde. Heavy metals and other toxic chemicals in children’s makeup and body products are particularly harmful to infants and youth, who are growing rapidly and whose bodies are less efficient at metabolizing these chemicals. Whether these chemicals are added intentionally or are present as contaminants, they have been associated with cancer, neurodevelopmental harm, and other serious and irreversible health effects, the Columbia University and Earthjustice researchers noted.
“Even when concentrations of individual chemicals are low in products, the potential for interactive effects from multiple toxicants is important to take into consideration,” the authors wrote in the journal article. “Allergic reactions, such as contact dermatitis, are some of the most frequently cited negative health outcomes associated with the use of cosmetics.”

Children’s small body side, rapid growth rate and immature immune systems are biologically more prone to the effects of toxicants than adults.
Adobe Stock
In addition to children’s rapid growth rate, the study also reported that their small body size, developing tissues and organs, and immature immune systems are biologically more prone to the effects of toxicants than adults. Meanwhile, the study noted, “childhood exposure to harmful makeup and body product ingredients can also be considered an environmental justice issue, as communities of color may be more likely to use these products.”
Although adults are the typical users of cosmetics, similar items are heavily marketed to youth with attention-grabbing features such as bright colors, animals and cartoon characters, according to the study. Beyond conventional makeup such as eyeshadow and lipstick, children may apply face paint, body glitter, nail polish, hair gel and fragrances. They also may frequent social media platforms on which these products are increasingly being promoted.
Products for both children and adults are currently regulated by the U.S. Food and Drug Administration under the Federal Food, Drug, and Cosmetic Act of 1938. Also, the Fair Packaging and Labeling Act of 1967 directs the Federal Trade Commission and the FDA “to issue regulations requiring that all ‘consumer commodities’ be labeled to disclose net contents, identity of commodity, and name and place of business of the product's manufacturer, packer, or distributor.” As the Columbia University and Earthjustice authors pointed out, though, “current safety regulations have been widely criticized as inadequate.”
The Personal Care Products Council in Washington, D.C., “fundamentally disagrees with the premise that companies put toxic chemicals in products produced for children,” industry spokeswoman Lisa Powers said in an email. Founded in 1894, the national trade association represents 600 member companies that manufacture, distribute and supply most personal care products marketed in the United States.
No category of consumer products is subject to less government oversight than cosmetics and other personal care products. -- Environmental Working Group.
“Science and safety are the cornerstones of our industry,” Powers stated. For more than a decade, she wrote, “the [Council] and our member companies worked diligently with a bipartisan group of congressional leaders and a diverse group of stakeholders to enhance the effectiveness of the FDA regulatory authority and to provide the safety reassurances that consumers expect and deserve.”
Powers added that the “industry employs and consults thousands of scientific and medical experts” who study the impacts of cosmetics and personal care products and the ingredients used in them. The Council also maintains a comprehensive database where consumers can look up science and safety information on the thousands of ingredients in sunscreens, toothpaste, shampoo, moisturizer, makeup, fragrances and other products.
However, the Environmental Working Group, which empowers consumers with breakthrough research to make informed choices about healthy living, believes the regulations are still not robust enough. “No category of consumer products is subject to less government oversight than cosmetics and other personal care products,” states the organization’s website. “Although many of the chemicals and contaminants in cosmetics and personal care products likely pose little risk, exposure to some has been linked to serious health problems, including cancer.”
The group, which operates the Skin Deep Database noted that “since 2009, 595 cosmetics manufacturers have reported using 88 chemicals, in more than 73,000 products, that have been linked to cancer, birth defects or reproductive harm.”
But change, for both adults and kids, is on the horizon. The Modernization of Cosmetics Regulation Act of 2022 significantly expanded the FDA’s authority to regulate cosmetics. In May 2023, Washington state adopted a law regulating cosmetics and personal care products. The Toxic-Free Cosmetics Act (HB 1047) bans chemicals in beauty and personal care products, such as PFAS, lead, mercury, phthalates and formaldehyde-releasing agents. These bans take effect in 2025, except for formaldehyde releasers, which have a phased-in approach starting in 2026.
Industry and advocates view this as a positive development. Powers, the spokesperson, praised “the long-awaited” Modernization Cosmetics Regulation Act of 2022, which she said, “advances product safety and innovation.” Jen Lee, chief impact officer at Beautycoutner, a company that sells personal care products, also welcomes the change. “We were proud to support the Washington Toxic-Free Cosmetics Act (HB 1047) by mobilizing our community of Brand Advocates who reside in Washington State,” Lee said. “Together, they made their voices heard by sending over 1,000 emails to their state legislators urging them to support and pass the bill.”
Laurie Valeriano, executive director of Toxic-Free Future, praised the upcoming Washington state law as “a huge win for public health and the environment that will have impacts that ripple across the nation.” She added that “companies won’t make special products for Washington state.” Instead, “they will reformulate and make products safer for everyone” — adults and children.
You shouldn’t have to be a toxicologist to shop for shampoo. -- Washington State Rep. Sharlett Mena
The new legislation will require Washington state agencies to assess the hazards of chemicals used in products that can impact vulnerable populations, while providing support for small businesses and independent cosmetologists to transition to safer products.

The Toxic-Free Future team lauds the Cosmetics Act, signed in May 2023.
Courtesy Toxic-Free Future
“When we go to a store, we assume the products on the shelf are safe, but this isn’t always true,” said Washington State Rep. Sharlett Mena, a Democrat serving in the 29th Legislative District (Tacoma), who sponsored the law. “I introduced this bill (HB 1047) because currently, the burden is on the consumer to navigate labels and find safe alternatives. You shouldn’t have to be a toxicologist to shop for shampoo.”
The new law aims to protect people of all ages, but especially youth. “Children are more susceptible to the impacts of toxic chemicals because their bodies are still developing,” Mena said. “Lead, for example, is significantly more hazardous to children than adults. Also, since children, unlike adults, tend to put things in their mouths all the time, they are more exposed to harmful chemicals in personal care and other products.”
Cosmetologists and hair professionals are taking notice. “Safety should be the practitioner’s number one concern” in using products on small children, said Anwar Saleem, a hair stylist, instructor and former salon owner in Washington, D.C., who is chairman of the D.C. Board of Barbering and Cosmetology and president of the National Interstate Council of State Boards of Cosmetology. “There are so many products on the market that it can be confusing.”
Hair products designed and labeled for children's use often have milder formulations, but “every child is unique, and what works for one may not work for another,” Saleem said. He recommends doing a patch test, in which the stylist or cosmetologist dabs the product on a small, inconspicuous area of the scalp or skin and waits anywhere from an hour to a day to check for irritation before continuing to serve the client. “Performing a patch test, observing children's reactions to a product and adequately adjusting are essential.”
Saleem seeks products that are free from harsh chemicals such as sulfates, phthalates and parabens, noting that these ingredients can be irritating and drying to the hair and scalp. If a child has sensitive skin or allergies, Saleem opts for hypoallergenic products.
We also need to ensure that less toxic alternatives are available and accessible to all consumers. It’s often under-resourced, low-income populations who suffer the burden of environmental exposures and do not have access or cannot afford these safer alternatives. -- Lesliam Quirós-Alcalá.
Lesliam Quirós-Alcalá, an assistant professor in the department of environmental health and engineering at the Johns Hopkins Bloomberg School of Public Health, said current regulatory loopholes on product labeling still allow manufacturers to advertise their cosmetics and personal care products as “gentle” and “natural.” However, she said, those terms may be misleading as they don’t necessarily mean the contents are less toxic or harmful to consumers.
“We also need to ensure that less toxic alternatives are available and accessible to all consumers,” Quirós-Alcalá said, “as often alternatives considered to be less toxic come with a hefty price tag.” As a result, “it’s often under-resourced, low-income populations who suffer the burden of environmental exposures and do not have access or cannot afford these safer alternatives.”
To advocate for safer alternatives, Quirós-Alcalá suggests that parents turn to consumer groups involved in publicizing the harms of personal care products. The Campaign for Safe Cosmetics is a program of Breast Cancer Prevention Partners, a national science-based advocacy organization aiming to prevent the disease by eliminating related environmental exposures. Other resources that inform users about unsafe ingredients include the mobile apps Clearya and Think Dirty.
“Children are not little adults, so it’s important to increase parent and consumer awareness to minimize their exposures to toxic chemicals in everyday products,” Quirós-Alcalá said. “Becoming smarter, more knowledgeable consumers is the first step to protecting your family from potentially harmful and toxic ingredients in consumer products.”
Often called the window to the soul, the eyes are more sacred than other body parts, at least for some.
Awash in a fluid finely calibrated to keep it alive, a human eye rests inside a transparent cubic device. This ECaBox, or Eyes in a Care Box, is a one-of-a-kind system built by scientists at Barcelona’s Centre for Genomic Regulation (CRG). Their goal is to preserve human eyes for transplantation and related research.
In recent years, scientists have learned to transplant delicate organs such as the liver, lungs or pancreas, but eyes are another story. Even when preserved at the average transplant temperature of 4 Centigrade, they last for 48 hours max. That's one explanation for why transplanting the whole eye isn’t possible—only the cornea, the dome-shaped, outer layer of the eye, can withstand the procedure. The retina, the layer at the back of the eyeball that turns light into electrical signals, which the brain converts into images, is extremely difficult to transplant because it's packed with nerve tissue and blood vessels.
These challenges also make it tough to research transplantation. “This greatly limits their use for experiments, particularly when it comes to the effectiveness of new drugs and treatments,” said Maria Pia Cosma, a biologist at Barcelona’s Centre for Genomic Regulation (CRG), whose team is working on the ECaBox.
Eye transplants are desperately needed, but they're nowhere in sight. About 12.7 million people worldwide need a corneal transplant, which means that only one in 70 people who require them, get them. The gaps are international. Eye banks in the United Kingdom are around 20 percent below the level needed to supply hospitals, while Indian eye banks, which need at least 250,000 corneas per year, collect only around 45 to 50 thousand donor corneas (and of those 60 to 70 percent are successfully transplanted).
As for retinas, it's impossible currently to put one into the eye of another person. Artificial devices can be implanted to restore the sight of patients suffering from severe retinal diseases, but the number of people around the world with such “bionic eyes” is less than 600, while in America alone 11 million people have some type of retinal disease leading to severe vision loss. Add to this an increasingly aging population, commonly facing various vision impairments, and you have a recipe for heavy burdens on individuals, the economy and society. In the U.S. alone, the total annual economic impact of vision problems was $51.4 billion in 2017.
Even if you try growing tissues in the petri dish route into organoids mimicking the function of the human eye, you will not get the physiological complexity of the structure and metabolism of the real thing, according to Cosma. She is a member of a scientific consortium that includes researchers from major institutions from Spain, the U.K., Portugal, Italy and Israel. The consortium has received about $3.8 million from the European Union to pursue innovative eye research. Her team’s goal is to give hope to at least 2.2 billion people across the world afflicted with a vision impairment and 33 million who go through life with avoidable blindness.
Their method? Resuscitating cadaveric eyes for at least a month.
If we succeed, it will be the first intact human model of the eye capable of exploring and analyzing regenerative processes ex vivo. -- Maria Pia Cosma.
“We proposed to resuscitate eyes, that is to restore the global physiology and function of human explanted tissues,” Cosma said, referring to living tissues extracted from the eye and placed in a medium for culture. Their ECaBox is an ex vivo biological system, in which eyes taken from dead donors are placed in an artificial environment, designed to preserve the eye’s temperature and pH levels, deter blood clots, and remove the metabolic waste and toxins that would otherwise spell their demise.

Scientists work on resuscitating eyes in the lab of Maria Pia Cosma.
Courtesy of Maria Pia Cosma.
“One of the great challenges is the passage of the blood in the capillary branches of the eye, what we call long-term perfusion,” Cosma said. Capillaries are an intricate network of very thin blood vessels that transport blood, nutrients and oxygen to cells in the body’s organs and systems. To maintain the garland-shaped structure of this network, sufficient amounts of oxygen and nutrients must be provided through the eye circulation and microcirculation. “Our ambition is to combine perfusion of the vessels with artificial blood," along with using a synthetic form of vitreous, or the gel-like fluid that lets in light and supports the the eye's round shape, Cosma said.
The scientists use this novel setup with the eye submersed in its medium to keep the organ viable, so they can test retinal function. “If we succeed, we will ensure full functionality of a human organ ex vivo. It will be the first intact human model of the eye capable of exploring and analyzing regenerative processes ex vivo,” Cosma added.
A rapidly developing field of regenerative medicine aims to stimulate the body's natural healing processes and restore or replace damaged tissues and organs. But for people with retinal diseases, regenerative medicine progress has been painfully slow. “Experiments on rodents show progress, but the risks for humans are unacceptable,” Cosma said.
The ECaBox could boost progress with regenerative medicine for people with retinal diseases, which has been painfully slow because human experiments involving their eyes are too risky. “We will test emerging treatments while reducing animal research, and greatly accelerate the discovery and preclinical research phase of new possible treatments for vision loss at significantly reduced costs,” Cosma explained. Much less time and money would be wasted during the drug discovery process. Their work may even make it possible to transplant the entire eyeball for those who need it.
“It is a very exciting project,” said Sanjay Sharma, a professor of ophthalmology and epidemiology at Queen's University, in Kingston, Canada. “The ability to explore and monitor regenerative interventions will increasingly be of importance as we develop therapies that can regenerate ocular tissues, including the retina.”
Seemingly, there's no sacred religious text or a holy book prohibiting the practice of eye donation.
But is the world ready for eye transplants? “People are a bit weird or very emotional about donating their eyes as compared to other organs,” Cosma said. And much can be said about the problem of eye donor shortage. Concerns include disfigurement and healthcare professionals’ fear that the conversation about eye donation will upset the departed person’s relatives because of cultural or religious considerations. As just one example, Sharma noted the paucity of eye donations in his home country, Canada.
Yet, experts like Sharma stress the importance of these donations for both the recipients and their family members. “It allows them some psychological benefit in a very difficult time,” he said. So why are global eye banks suffering? Is it because the eyes are the windows to the soul?
Seemingly, there's no sacred religious text or a holy book prohibiting the practice of eye donation. In fact, most major religions of the world permit and support organ transplantation and donation, and by extension eye donation, because they unequivocally see it as an “act of neighborly love and charity.” In Hinduism, the concept of eye donation aligns with the Hindu principle of daan or selfless giving, where individuals donate their organs or body after death to benefit others and contribute to society. In Islam, eye donation is a form of sadaqah jariyah, a perpetual charity, as it can continue to benefit others even after the donor's death.
Meanwhile, Buddhist masters teach that donating an organ gives another person the chance to live longer and practice dharma, the universal law and order, more meaningfully; they also dismiss misunderstandings of the type “if you donate an eye, you’ll be born without an eye in the next birth.” And Christian teachings emphasize the values of love, compassion, and selflessness, all compatible with organ donation, eye donation notwithstanding; besides, those that will have a house in heaven, will get a whole new body without imperfections and limitations.
The explanation for people’s resistance may lie in what Deepak Sarma, a professor of Indian religions and philosophy at Case Western Reserve University in Cleveland, calls “street interpretation” of religious or spiritual dogmas. Consider the mechanism of karma, which is about the causal relation between previous and current actions. “Maybe some Hindus believe there is karma in the eyes and, if the eye gets transplanted into another person, they will have to have that karmic card from now on,” Sarma said. “Even if there is peculiar karma due to an untimely death–which might be interpreted by some as bad karma–then you have the karma of the recipient, which is tremendously good karma, because they have access to these body parts, a tremendous gift,” Sarma said. The overall accumulation is that of good karma: “It’s a beautiful kind of balance,” Sarma said.
For the Jews, Christians, and Muslims who believe in the physical resurrection of the body that will be made new in an afterlife, the already existing body is sacred since it will be the basis of a new refashioned body in an afterlife.---Omar Sultan Haque.
With that said, Sarma believes it is a fallacy to personify or anthropomorphize the eye, which doesn’t have a soul, and stresses that the karma attaches itself to the soul and not the body parts. But for scholars like Omar Sultan Haque—a psychiatrist and social scientist at Harvard Medical School, investigating questions across global health, anthropology, social psychology, and bioethics—the hierarchy of sacredness of body parts is entrenched in human psychology. You cannot equate the pinky toe with the face, he explained.
“The eyes are the window to the soul,” Haque said. “People have a hierarchy of body parts that are considered more sacred or essential to the self or soul, such as the eyes, face, and brain.” In his view, the techno-utopian transhumanist communities (especially those in Silicon Valley) have reduced the totality of a person to a mere material object, a “wet robot” that knows no sacredness or hierarchy of human body parts. “But for the Jews, Christians, and Muslims who believe in the physical resurrection of the body that will be made new in an afterlife, the [already existing] body is sacred since it will be the basis of a new refashioned body in an afterlife,” Haque said. “You cannot treat the body like any old material artifact, or old chair or ragged cloth, just because materialistic, secular ideologies want so,” he continued.
For Cosma and her peers, however, the very definition of what is alive or not is a bit semantic. “As soon as we die, the electrophysiological activity in the eye stops,” she said. “The goal of the project is to restore this activity as soon as possible before the highly complex tissue of the eye starts degrading.” Cosma’s group doesn’t yet know when they will be able to keep the eyes alive and well in the ECaBox, but the consensus is that the sooner the better. Hopefully, the taboos and fears around the eye donations will dissipate around the same time.


