A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
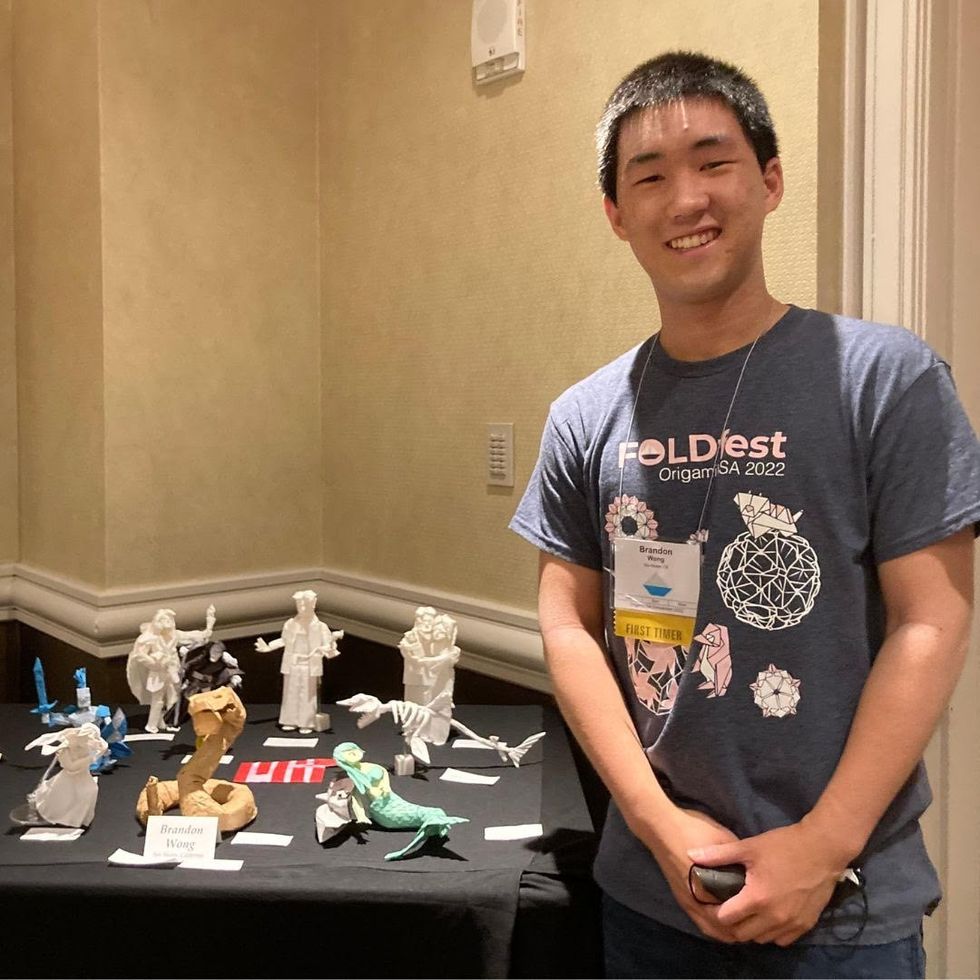
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Jessica Lovett, who suffers from long Covid, feels a renewed sense of energy and hope since getting vaccinated.
One of the biggest challenges of the COVID-19 pandemic is the way in which it has forced us to question our hopes. In normal times, hope is a tonic we take in small doses to keep us moving forward through the slog of daily life. The pandemic, however, has made it a much scarcer commodity, spurring us not only to seek it more desperately but to scrutinize it more closely.
Every bit of reassurance seems to come with caveats: Masks can shield us from the coronavirus, but they may need to be doubled in some situations to provide adequate protection. Vaccines work, but they may not be as effective against some viral variants—and they can cause extremely rare but serious side effects. Every few weeks, another potential miracle cure makes headlines (Hydroxychloroquine! Convalescent plasma!), only to prove disappointing on closer inspection. It's hard to know which alleged breakthroughs are worth pinning our hopes on, and which are the products of wishful thinking or hucksterism.
In January 2021, a study published in the journal Gut offered evidence that bacteria in the intestines might influence a whole spectrum of symptoms in long-haul patients.
Lately, two possible sources of hope have emerged concerning so-called "long COVID"—the debilitating syndrome, estimated to affect up to one-third of patients, in which physical, neurological, and cognitive symptoms persist for months. The first encouraging item has gotten plenty of media attention: reports that some long-haulers feel better after being vaccinated. The second item, while less widely covered, has caused a stir among scientists: a study suggesting that rebalancing the gut microbiome—the community of microorganisms in our intestines—could decrease both the severity and duration of the illness.
How optimistic should we allow ourselves to be about either of these developments? Experts warn that it's too soon to tell. Yet research into how vaccines and gut bacteria affect long-haulers—and how both factors might work together—could eventually help solve key pieces of the pandemic puzzle.
Investigating the Role of the Gut Microbiome
The idea that there may be a link between COVID-19 and gut health comes as no surprise to Jessica Lovett. Her case began in June 2020 with gastrointestinal distress—a symptom that was just beginning to be recognized as commonplace in what had initially been considered a respiratory illness. "I had diarrhea three to five times a day for two months," Lovett recalls. "I lost a lot of weight." By July, she was also suffering shortness of breath, chest pain, racing heartbeat, severe fatigue, brain fog, migraines, memory lapses, and more. As with many other COVID long-haulers, these troubles waxed and waned in an endless parade.
Lovett was the marketing manager for a music school in Austin, Texas, and the mother of a two-year-old boy. Just before she got sick, she ran a 5K race for her 40th birthday. Afterward, she had to give up her job, stop driving, and delegate childcare to her husband (who fell ill shortly before she did but recovered in 12 days). Tests showed no visible damage to her lungs, heart, or other organs. But she felt intuitively that taming her GI troubles would be key to getting well. On the advice of fellow patients in a long-COVID Facebook group—and, later, with the guidance of a doctor—she tried avoiding foods thought to trigger histamine reactions or inflammation. That seemed to help some, as did nutritional supplements, antihistamines, and angina medications. Still, she relapsed frequently, and was often bedridden.
In January 2021, a study published in the journal Gut offered evidence that bacteria in the intestines might influence a whole spectrum of symptoms in patients like Lovett. Researchers at the Chinese University of Hong Kong examined blood and stool samples and medical records from 100 hospital patients with lab-confirmed COVID-19 infections, and from 78 people without the disease who were taking part in a microbiome study before the pandemic.
The team, led by professor Siew Chien Ng, found that the makeup of the gut microbiome differed sharply between the two groups. Patients with COVID had higher levels of three bacterial species than those without the infection, but lower levels of several species known to enhance immune system response. Reductions in two of those species—Faecalibacterium prausnitzii and Bifidobacterium bifidum—were associated with more severe symptoms. And the numbers of such helpful bacteria remained low in stool samples collected up to 30 days after infected patients had seemingly cleared the coronavirus from their bodies.
Analysis of blood samples, moreover, showed that these bacterial imbalances correlated with higher levels of inflammatory cytokines (immune system chemicals that are elevated in many patients with severe COVID-19) and markers of tissue damage, such as C-reactive protein.
These findings led the researchers to suggest that rebalancing the microbiome might lessen not only the intensity of COVID symptoms, but also their persistence. "Bolstering of beneficial gut species depleted in COVID-19," they wrote, "could serve as a novel avenue to mitigate severe disease, underscoring the importance of managing patients' gut biota during and after COVID-19."
Soon afterward, Ng revealed that she was working on a solution. Her team, she told Medscape, had developed "a microbiome immunity product that is targeted to what is missing in COVID-19 patients." Early research showed that hospitalized patients who received the treatment developed more antibodies, had fewer symptoms, and were discharged sooner. "So it is quite a bright and promising future," she enthused, "in alleviating some of these detrimental effects of the virus."
The Chicken-and-Egg Problem
Ng's study isn't the only one to suggest a connection between the gut and long COVID. Researchers led by gastroenterologist Saurabh Mehandru at New York's Mount Sinai Hospital recently determined that SARS-CoV-2, the virus that causes COVID-19, can linger in the intestines for months after a patient tests negative. Some studies have also found that gastrointestinal symptoms in the acute phase of the illness correlate with poorer outcomes—though that's far from settled. (In another study, Mehandru's team found lower mortality among patients presenting with GI symptoms.) But the Hong Kong group's paper was the first to posit that resident microbes may play a decisive role in the disease.
That view reflects growing evidence that these bugs can influence a range of ailments, from diabetes to schizophrenia. Over the past decade, the gut microbiome has emerged as a central regulator of the immune system. Some intestinal bacteria emit chemicals that signal immune cells to reduce production of inflammatory proteins, or help those cells effectively target invading pathogens. They also help maintain the integrity of the intestinal lining—preventing the syndrome known as "leaky gut," in which harmful microbes or toxins penetrate to the underlying tissue, potentially wreaking havoc throughout the body and brain.
Nonetheless, many experts have responded to Ng's findings with distinct caution. One problem, they point out, is the chicken-and-egg question: Do reduced levels of beneficial gut bacteria trigger the inflammation seen in COVID-19, or does inflammation triggered by COVID-19 kill off beneficial gut bacteria? "It's an issue of causality versus just association," explains Somsouk Ma, a professor of gastroenterology at the University of California, San Francisco. "I tend to think that the shift in microbes is more likely a consequence of the infection. But, of course, that's just speculation."
A related issue is whether a pill that replenishes "good" bacteria can really combat the effects of COVID-19—whether acute or chronic. Although scientists are studying fecal transplants and other probiotic therapies for many disorders, none has yet been approved by the U.S Food and Drug Administration. "The only situation where bacterial transplantation is known to work is in a form of colitis called Clostridium difficile," notes Mehandru. "I think it's a bit premature to lay too much emphasis on this in the context of COVID."
Placebo-controlled clinical trials will be needed to determine the efficacy of Ng's approach. (Consumer warning: The bacteria she's employing are not found in commercially available probiotics.) Whatever the results, such research—along with studies that track patients' gut microbiomes before, during, and after COVID-19 infection—could help scientists understand why some people have such trouble kicking the disease.
An Unexpected Benefit of Vaccines
The question of what causes long COVID is also central to understanding the effects of vaccines on the condition. In March, as inoculation campaigns took off across the nation, many long-haulers were delighted to see their symptoms disappear within days of getting the shot. "I woke up and it was like, 'Oh what a beautiful morning,'" one patient told The New York Times.
Yet the effects have been far from uniform. Although scientific surveys have not yet been conducted, an April poll by a Facebook group called Survivor Corps found numbers close to experts' estimates: 39 percent said they experienced partial to full recovery post-vaccination; 46 percent saw no difference; and 14 percent felt worse.
How could vaccines—which are designed to prevent COVID-19, not cure it—help some chronic patients get well? In a blog post, Yale immunologist Akiko Iwasaki suggested that the answer depends on what is driving a particular patient's symptoms. Iwasaki identified three possible mechanisms behind long COVID: 1) a persistent viral reservoir; 2) a "viral ghost," composed of fragments of the virus (RNA or proteins) that linger after the infection has been cleared but can still stimulate inflammation; and 3) an autoimmune response triggered by the infection, inducing a patient's immune cells to attack her own tissues.
These mechanisms "are not mutually exclusive," Iwasaki wrote, "and all three might benefit from the vaccines." If a patient has a viral reservoir, vaccine-induced immune cells and antibodies might be able to eliminate it. If the patient has a viral ghost, those vaccine-primed immune responses might knock it out as well. And if the patient is suffering from a COVID-triggered autoimmune syndrome, the vaccine might act as a decoy, shifting the immune system's attention to antigens contained in the shot (and perhaps reprogramming autoimmune cells in the process). The varying role of these underlying factors, and possibly others—such as the gut microbiome—might also help explain why vaccines don't benefit all long-haulers equally. Iwasaki and her team recently launched a clinical study to investigate this theory.
Pato Hebert, a professor of art and public policy at NYU, contracted COVID-19 in March 2020 while on sabbatical in Los Angeles. Hebert, then 50, started out with mild flu-like symptoms, but he was slammed with fatigue, headaches, and confusion a week after testing positive. In April, he landed in urgent care with severe shortness of breath. His brain fog worsened that summer, and a gentle swim brought on a dizzy spell so overwhelming that he feared it was a stroke. (Thankfully, tests showed it wasn't.) In September, he developed severe GI issues, which came and went over the following months. He found some relief through medications, dietary adjustments, acupuncture, herbal remedies, and careful conservation of his physical and mental energy—but a year after his diagnosis, he was still sick.
Hebert received his first dose of the Moderna vaccine on March 1, 2021; it made no difference in his symptoms. After his second dose, on the 29th, he suffered terrible headaches—"like early COVID days," he told me. A week later, his condition had improved slightly compared to pre-vaccination. "With a few exceptions, my fatigue and brain fog have been less challenging," he reported. "I'm cautiously optimistic." But in late April, he suffered another flareup of respiratory and GI issues.
For Jessica Lovett, the vaccine's effects were more dramatic. After her first dose of the Pfizer-BioNTech formula, on February 26, her cognitive symptoms improved enough that she was able to drive again; within a week, she was pushing her son uphill in a stroller, lifting light weights, and running for short distances. After the second dose, she says, "I had incredible energy. It was insane, like I drank three cups of coffee."
Lovett (who now runs a Facebook support group for Austin locals, ATX Covid Long Haulers) stresses that the vaccine hasn't cured her. She winds up back in bed whenever she pushes herself too hard. She still needs to take antihistamines and shun certain foodstuffs; any slip-up brings another relapse. Yet she's able to live more fully than at any time since she fell ill—and she has begun to feel a renewed sense of hope.
Recently, in fact, she and her husband decided to expand their family. "I guess that tells you something," she says with a laugh. "The doctors have given us the okay, and we're going to try."
A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
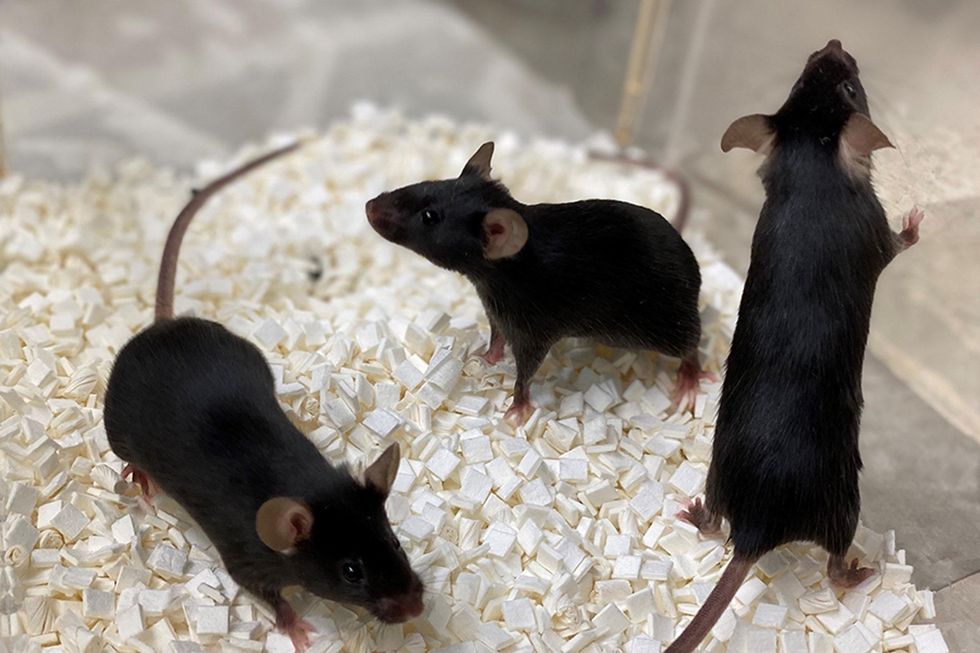
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

