A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
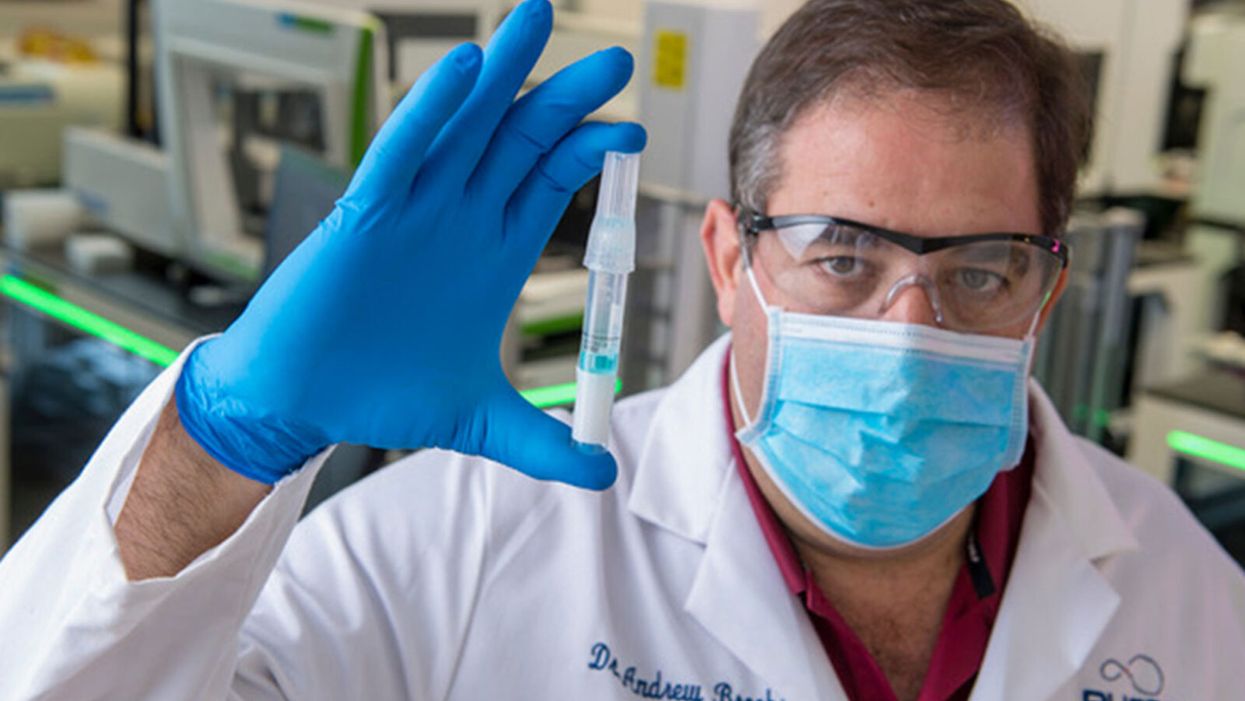
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
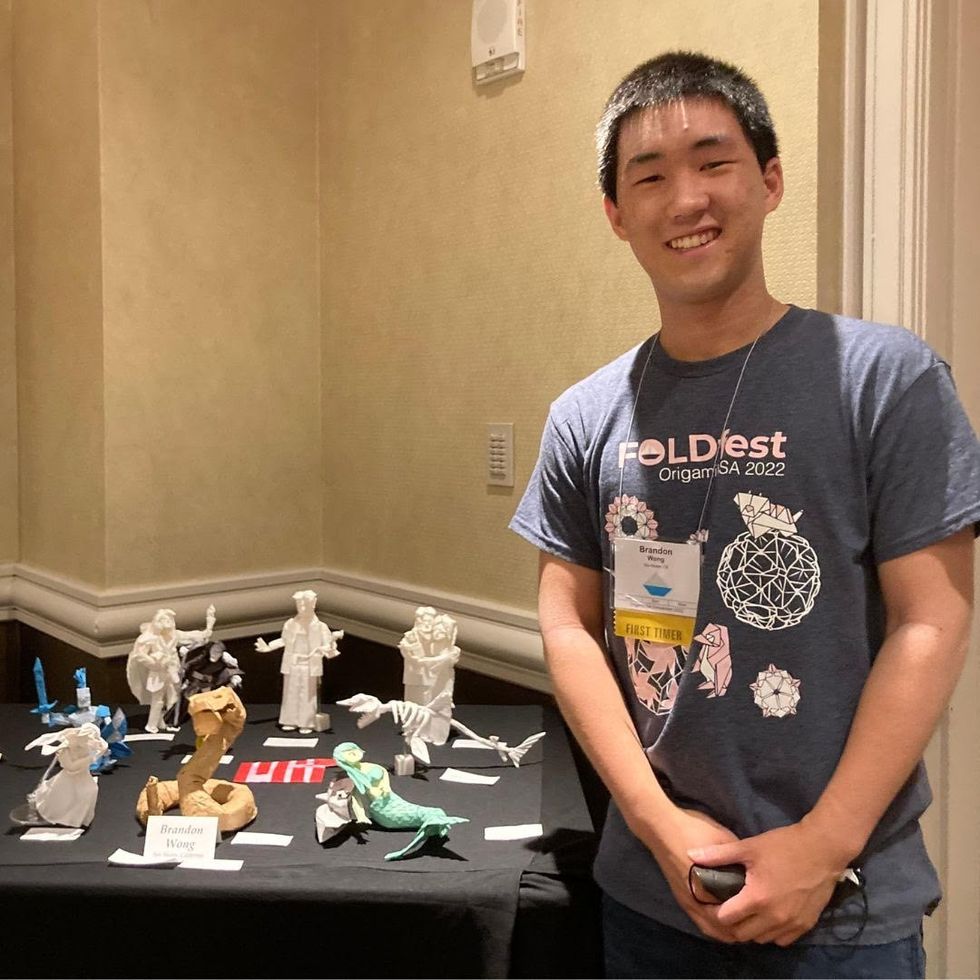
Dr. Andrew Brooks of RUCDR Infinite Biologics holds up a saliva sample.
The patient tilts back her head and winces as the long swab stick pushes six inches up her nose. The tip twirls around uncomfortably before it's withdrawn.
"Our saliva test can detect the virus in asymptomatic and pre-symptomatic cases."
A gloved and gowned healthcare worker wearing a face shield and mask tells the patient that she will learn whether she is positive for COVID-19 as soon as the lab can process her test.
This is the typical unpleasant scenario for getting a coronavirus test. But times are rapidly changing: Today, for the first time, the U.S. Food and Drug Administration cleared one company to sell saliva collection kits for individuals to use at home.
Scientists at the startup venture, RUCDR Infinite Biologics at Rutgers University in New Jersey, say that saliva testing offers an easier, more useful alternative to the standard nasal swab.
"Our saliva test can detect the virus in asymptomatic and pre-symptomatic cases," said Dr. Andrew Brooks, chief operating officer at RUCDR.
Another venture, Darwin BioSciences in Colorado, has separately developed an innovative method of testing saliva for the coronavirus that causes COVID-19.
Saliva testing can allow earlier detection to identify people who may not know they are contagious, say scientists at both companies. In addition, because patients spit into a tube or cup, saliva testing is safer for healthcare workers than taking swabs. This frees up scarce personal protective equipment (PPE) for use elsewhere. Nasal swabs themselves have been in scarce supply.
Saliva testing, if it becomes widespread, potentially could mean opening society sooner. The more ubiquitous testing becomes across the population, experts say, the more feasible it becomes for public health officials to trace and isolate contacts, especially of asymptomatic cases. Testing early and often will be essential to containing emerging hot spots before a vast outbreak can take root.
Darwin Biosceiences is preparing to seek an FDA Emergency Use Authorization (EUA) this month for its patented "CoVScreen" testing system, which potentially could be available to labs nationally by mid-summer.
Meanwhile, Infinite Biologics will now begin selling kits to consumers for home collection, upon order by a physician. The FDA said that the company's saliva test was as accurate as the nasal swab method used by health care professionals. An FDA summary documenting the company's data reported: "There was 100% positive and negative agreement between the results obtained from testing of saliva and those obtained from nasopharyngeal and oropharyngeal swabs."
The greatest scientific advantage, said Dr. Brooks, is that nasal and oral swabs only collect the surface area where the swab goes, which may not be the place with most viral load. In contrast, the virus occurs throughout a saliva sample, so the test is more trustworthy.
The lab at Rutgers can process 20,000 tests a day, with a 48-hour turnaround. They have 75,000 tests ready to ship now.
The Leap: Detecting Sickness Before You Feel It
"We wanted to create a device that could detect infections before symptoms appeared," explained Nicholas Meyerson, co-founder and CEO of Darwin.
For more than 300 years, he said, "the thermometer was the gold standard for detecting disease because we thought the first sign of illness was a fever. This COVID-19 pandemic has proven that not all pathogens cause a fever. You can be highly contagious without knowing it."
"The question is whether we can scale up fast enough to meet the need. I believe saliva testing can help."
Therefore, Meyerson and co-founder Sara Sawyer from the University of Colorado began to identify RNA biomarkers that can sense when a pathogen first enters a molecule and "sets off alarms." They focused on the nucleic acids concentrated in saliva as the best and easiest place to collect samples for testing.
"The isothermal reaction in saliva takes place at body or room temperature," he said, "so there's no need for complicated testing machinery. The chemical reaction can be read out on a paper strip, like a pregnancy test -- two stripes if you're sick, and one stripe if you're okay."
Before the pandemic, limited but successful human trials were already underway at CU in Boulder and at the CU Anschutz Medical Campus east of Denver. "This was our proof of concept," he said.
Darwin was founded in March and has secured enough venture capital to concentrate protype development on detecting the virus causing COVID-19. So far, said Meyerson, "Everything works."
A small double-blind test of 30 samples at CU produced 100 percent accuracy. "I'm not sure if that will hold true as we go into clinical trials," he said, "but I'm confident we will satisfy all the requirements for at least 95 percent clinical validation."
The specific "CoVStick" test strips will roll out soon, he said: "We hope before the second wave of the pandemic hits."
The broader saliva test-strip product from Darwin, "SickStick," is still one to two years away from deployment by the military and introduction into the consumer drugstore market for home use, said Meyerson. It will affordably and quickly detect a range of viral and bacterial infections.

An illustration of the "CoVStick."
(Darwin Biosciences)
A Potential Game Changer
Society needs widespread testing daily, said George Church, founding core faculty of the Wyss Institute for Biologically Inspired Engineering at Harvard University. Speaking at an online SynBioBeta webinar in April, he urged developing stockpiles of testing kits for home use.
As for any potential of false positives, Church said a much bigger risk is not having enough tests.
"Saliva testing is going to speed up the timeline for opening society a lot," said Meyerson. "People need to self-collect samples at home. A lot more people are going to be willing to spit into a tube than to push a swab six inches up their own nose."
Brooks, of Rutgers, addressed the big picture. "It's critical that we open society as soon as possible to minimize the economic impact of the pandemic. Testing is the surest and safest path. The question is whether we can scale up fast enough to meet the need. I believe saliva testing can help."
A vaccine from Moderna could be available as early as January, Fauci recently said.
Earlier this year, biotech company Moderna broke world records for speed in vaccine development. Their researchers translated the genetic code of the coronavirus into a vaccine candidate in just 42 days.
We're about to expand our safety data in Phase II.
Phase I of the clinical trial started in Seattle on March 16th, with the already-iconic image of volunteer Jennifer Haller calmly receiving the very first dose.
Instead of traditional methods, this vaccine uses a new -- and so far unproven -- technology based on synthetic biology: It hijacks the software of life – messenger RNA – to deliver a copy of the virus's genetic sequence into cells, which, in theory, triggers the body to produce antibodies to fight off a coronavirus infection.
U.S. National Institute of Allergy and Infectious Diseases Director Anthony Fauci called the vaccine's preclinical data "impressive" and told National Geographic this week that a vaccine could be ready for general use as early as January.
The Phase I trial has dosed 45 healthy adults. Phase II trials are about to start, enrolling around 600 adults. Pivotal efficacy trials would follow soon thereafter, bankrolled in collaboration with the government office BARDA (Biomedical Advanced Research and Development Authority).
Today, the chief medical officer of Moderna, Tal Zaks, answered burning questions from the public in a webinar hosted by STAT. Here's an edited and condensed summary of his answers.
1) When will a vaccine become available?
We expect to have data in early summer about the antibody levels from our mRNA vaccine. At the same time, we can measure the antibody levels of people who have had the disease, and we should be able to measure the ability of those antibodies to prevent disease.
We will not yet know if the mRNA vaccine works to prevent disease, but we could soon talk about a potential for benefit. We don't yet know about risk. We're about to expand our safety data in Phase II.
In the summer, there is an expectation that we will be launching pivotal trials, in collaboration with government agencies that are helping fund the research. The trials would be launched with the vaccine vs. a placebo with the goal of establishing: How many cases can we show we prevented with the vaccine?
This is determined by two factors: How big is the trial? And what's the attack rate in the population we vaccinate? The challenge will be to vaccinate in the areas where the risk of infection is still high in the coming months, and we're able to vaccinate and demonstrate fewer infections compared to a placebo. If the disease is happening faster in a given area, you will be able to see an outcome faster. Potentially by the end of the year, we will have the data to say if the vaccine works.
Will that be enough for regulatory approval? The main question is: When will we cross the threshold for the anticipated benefit of a presumed vaccine to be worth the risk?
There is a distinction between approval for those who need it most, like the elderly. Their unmet need and risk/benefit is not the same as it is for younger adults.
My private opinion: I don't think it's a one-size-fits-all. It will be a more measured stance.
2) Can you speed up the testing process with challenge studies, where volunteers willingly get infected?
It's a great question and I applaud the people who ask it and I applaud those signing up to do it. I'm not sure I am a huge fan, for both practical and ethical reasons. The devil is in the details. A challenge study has to show us a vaccine can prevent not just infection but prevent disease. Otherwise, how do I know the dose in the challenge study is the right dose? If you take 100 young people, 90 of them will get mild or no disease. Ten may end up in hospital and one in the ICU.
Also, the timeline. Can it let you skip Phase II of large efficacy trial? The reality for us is that we are about to start Phase II anyway. It would be months before a challenge trial could be designed. And ethically: everybody agrees there is a risk that is not zero of having very serious disease. To justify the risk, we have to be sure the benefit is worth it - that it actually shrunk the timeline. To just give us another data point, I find it hard to accept.
This technology allows us to scale up manufacturing and production.
3) What was seen preclinically in the animal models with Moderna's mRNA vaccines?
We have taken vaccines using our technology against eight different viruses, including two flu strains. In every case, in the preclinical model, we showed we could prevent disease, and when we got to antibody levels, we got the data we wanted to see. In doses of 25-100 micrograms, that usually ends up being a sweet spot where we see an effect. It's a good place as to the expectation of what we will see in Phase I trials.
4) Why is Moderna pursuing an mRNA virus instead of a traditional inactivated virus or recombinant one? This is an untried technology.
First, speed matters in a pandemic. If you have tech that can move much quicker, that makes a difference. The reason we have broken world records is that we have invested time and effort to be ready. We're starting from a platform where it's all based on synthetic biology.
Second, it's fundamental biology - we do not need to make an elaborate vaccine or stick a new virus in an old virus, or try to make a neutralizing but not binding virus. Our technology is basically mimicking the virus. All life works on making proteins through RNA. We have a biological advantage by teaching the immune system to do the right thing.
Third, this technology allows us to scale up manufacturing and production. We as a company have always seen this ahead of us. We invested in our own manufacturing facility two years ago. We have already envisioned scale up on two dimensions. Lot size and vaccines. Vaccines is the easier piece of it. If everybody gets 100 micrograms, it's not a heck of a lot. Prior to COVID, our lead program was a CMV (Cytomegalovirus) vaccine. We had envisioned launching Phase III next year. We had been already well on the path to scale up when COVID-19 caught us by surprise. This would be millions and millions of doses, but the train tracks have been laid.
5) People tend to think of vaccines as an on-off switch -- you get a vaccine and you're protected. But efficacy can be low or high (like the flu vs. measles vaccines). How good is good enough here for protection, and could we need several doses?
Probably around 50-60 percent efficacy is good enough for preventing a significant amount of disease and decreasing the R0. We will aim higher, but it's hard to estimate what degree of efficacy to prepare for until we do the trial. (For comparison, the average flu vaccine efficacy is around 50 percent.)
We anticipate a prime boost. If our immune system has never seen a virus, you can show you're getting to a certain antibody level and then remind the immune system (with another dose). A prime boost is optimal.
My only two competitors are the virus and the clock.
6) How would mutations affect a vaccine?
Coronaviruses tend to mutate the least compared to other viruses but it's entirely possible that it mutates. The report this week about those projected mutations on the spike protein have not been predicted to alter the critical antibodies.
As we scale up manufacturing, the ability to plug in a new genetic sequence and get a new vaccine out there will be very rapid.
For flu vaccine, we don't prove efficacy every year. If we get to the same place with an mRNA vaccine, we will just change the sequence and come out with a new vaccine. The path to approval would be much faster if we leverage the totality of efficacy data like we do for flu.
7) Will there be more than one vaccine and how will they be made available?
I hope so, I don't know. The path to making these available will go through a public-private partnership. It's not your typical commercial way of deploying a vaccine. But my only two competitors are the virus and the clock. We need everybody to be successful.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.