A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
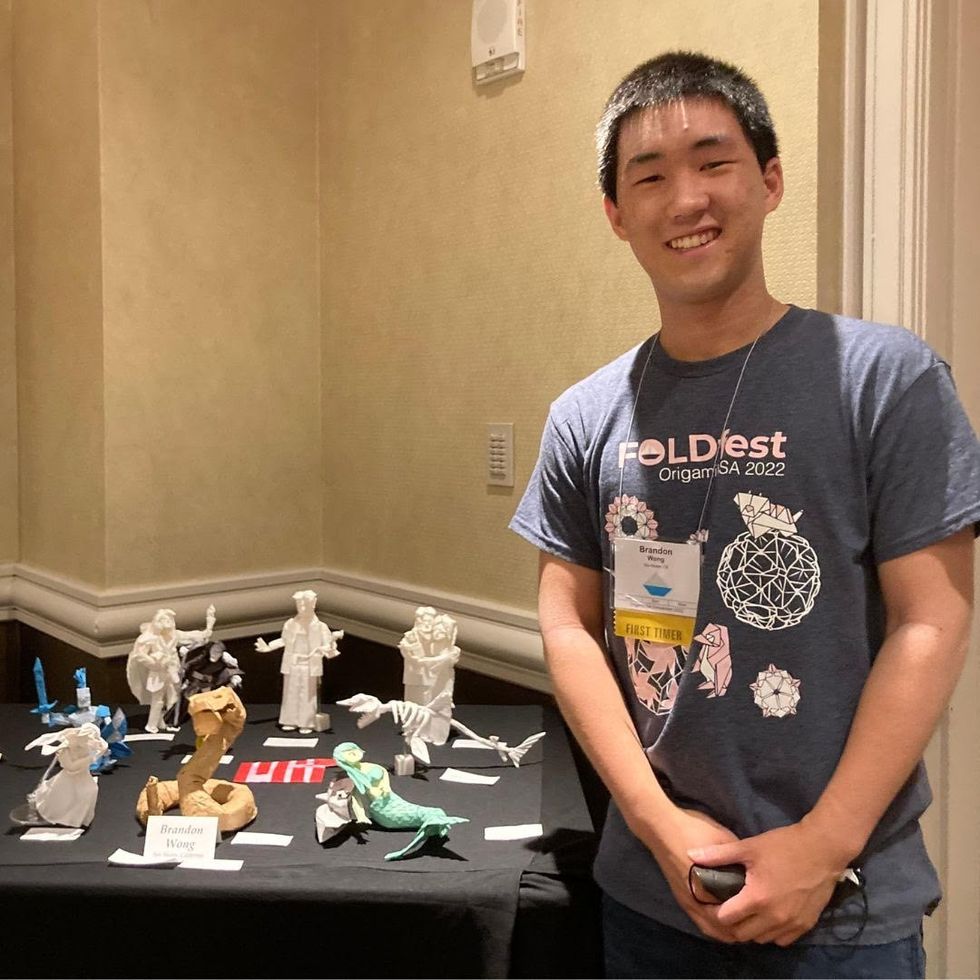
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Researchers Are Experimenting With Magic Mushrooms' Fascinating Ability to Improve Mental Health Disorders
Magic mushrooms, in conjunction with a psychotherapist's treatment, may be helpful in treating addiction, depression, anxiety, and other mental health ailments.
Mental illness is a dark undercurrent in the lives of tens of millions of Americans. According to the World Health Organization, about 450 million people worldwide have a mental health disorder, which cut across all demographics, cultures, and socioeconomic classes.
One area of research seems to herald the first major breakthrough in decades — hallucinogen-assisted psychotherapy.
The U.S. National Institute on Mental Health estimates that severely debilitating mental health disorders cost the U.S. more than $300 billion per year, and that's not even counting the human toll of broken lives, devastated families, and a health care system stretched to the limit.
However, one area of research seems to herald the first major breakthrough in decades — hallucinogen-assisted psychotherapy. Drugs like psilocybin (obtained from "magic mushrooms"), LSD, and MDMA (known as the club drug, ecstasy) are being tested in combination with talk therapy for a variety of mental illnesses. These drugs, administered by a psychotherapist in a safe and controlled environment, are showing extraordinary results that other conventional treatments would take years to accomplish.
But the therapy will likely continue to face an uphill legal battle before it achieves FDA approval. It is up against not only current drug laws (all psychedelics remain illegal on the federal level) and strict FDA regulations, but a powerful status quo that has institutionalized fear of any drug used for recreational purposes.
How We Got Here
According to researchers Sean Belouin and Jack Henningfield, the use of psychedelic drugs has a long and winding history. It's believed that hallucinogenic substances have been used in healing ceremonies and religious rituals for thousands of years. Indigenous people in the U.S., Mexico, and Central and South America still use distillations from the peyote cactus and other hallucinogens in their religious ceremonies. And psilocybin mushrooms, also capable of causing hallucinations, grow throughout the world and are thought to have been used for millennia.
But psychedelic drugs didn't receive much research until 1943, when LSD's psychoactive effects were discovered by chemist Albert Hoffman. Hoffman tested the compound he had discovered years earlier on himself and found that the drug had profound mind-altering effects. He made the drug available to psychiatrists who were interested in testing it out as an adjunct to talk therapy. There were no truly effective drugs at the time for mental illnesses, and psychiatrists early on saw the possibility of psychedelics providing a kind of emotional catharsis that might represent therapeutic breakthroughs for many mental conditions.
During the 1950s and early 1960s, psychedelic drugs saw an increase in use within psychology, according to a 2018 article in Neuropharmacology. During this time, research on LSD and other hallucinogens was the subject of over 1,000 scientific papers, six international conferences, and several dozen books. LSD was widely prescribed to psychiatric patients, and by 1958, Hoffman had identified psilocybin as the hallucinogenic in "magic mushrooms," which was also administered. By 1965 some type of hallucinogenic had been given to more than 40,000 patients.
Then came a sea change. Psychedelic drugs caught the public's attention and there was widespread experimentation. The association with Hippie counterculture alarmed many and led to a legal and cultural backlash that stigmatized psychedelics for decades to come. In the mid-1960s, psychedelics were designated Schedule 1 drugs in the U.S., meaning they were seen as having "no accepted medical use and a high potential of abuse." Schedule 1 also implied that the drugs were more dangerous than cocaine, methamphetamine, Vicodin, and oxycodone, a perception that was far from proven but became an institutionalized part of drug enforcement. Medical use ceased and research dwindled down to close to zero.
For years, research into hallucinogenic-assisted therapy was basically dormant, until the 1990s when interest started to revive. In the 2000s, the first modern clinical trials of psilocybin were done by Francisco Moreno at the University of Arizona and Matthew Johnson at Johns Hopkins. Scientists in the 2010s, including Robin Carhart-Harris, started studying the use of psychedelics in the treatment of major depressive disorder (MDD).
In small trials with these patients, results showed significant and long-term improvement (for at least six months) after only two episodes of psilocybin-assisted therapy. In several studies, the guided experience of administering one of the psychedelic drugs along with psychotherapy seemed to result in marked improvement in a variety of disorders, including depression, anxiety, PTSD, and addiction.
The drugs allowed patients to experience a radical reframing of reality, helping them to become "unstuck" from the anxious and negative tape loops that played in their heads. According to Michael Pollan, an American author and professor of journalism who wrote the book, "How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression and Transcendence," psychedelics allow patients to see their lives through a kind of wide angle, where boundaries vanish and they're able to experience "consciousness without self." This perspective is usually accompanied by profound feelings of oneness with the universe.
Pollan likens the effect to a fresh blanketing of snow over the deep ruts of unproductive thinking, which characterize depression and other mental disorders. Once the new snow has fallen, the ruts disappear and a new path can be chosen. Relief from symptoms comes immediately, and in numerous studies, is sustained for months.
In spite of growing evidence for the safety and efficacy of psychedelic-assisted psychotherapy, the practice has major hurdles to cross on its quest for FDA approval.
Some of the most influential studies have focused on testing the use of psilocybin to treat end-of-life anxiety in patients diagnosed with a terminal illness. In 2016, Stephen Ross and colleagues tested a single dose of psilocybin on 29 subjects with end-of-life anxiety due to a terminal cancer diagnosis. A control group received a niacin pill. The researchers reported that of the 29 receiving psilocybin, all of the patients had "immediate, substantial, and sustained clinical benefits," even after six months.
In spite of growing evidence for the safety and efficacy of psychedelic-assisted psychotherapy, the practice has major hurdles to cross on its quest for FDA approval. The National Institutes of Health is not currently supporting any clinical trials and the research relies on private sources of funding, often with small research organizations that cannot afford the high cost of clinical trials.
Given the controversial nature of the drugs, researchers in psychedelic-assisted therapies may be cautious about publicity. Leapsmag reached out to several leaders in the field but none agreed to an interview.
Looking Ahead
Still, interest is building in the combination of psychedelic drugs and psychotherapy for treatment-resistant mental illnesses. Two months ago, Johns Hopkins University launched a new psychedelic research center with an infusion of $17 million from private investors. The center will focus on psychedelic-assisted therapies for opioid addiction, Alzheimer's disease, PTSD and major depression, to name just a few. Currently, of 51 cancer patients enrolled in a Hopkins study, more than half reported a decrease in depression and anxiety after receiving therapy with psilocybin. Two thirds even claimed that the experience was one of the most meaningful of their lives.
It is not unheard of for Schedule 1 drugs to make their way into medical use if they're shown to provide a bonafide improvement in a medical condition through well-designed clinical trials. MDMA, for example, has been designated a Breakthrough Therapy by the FDA as part of an Investigational New Drug Application. The FDA has agreed to a special protocol assessment that could speed up phase three clinical trials. The next step is for the data to be submitted to the FDA for an in-depth regulatory review. If the FDA agrees, MDMA-assisted therapy could be legalized.
Will the positive buzz around psychedelics persuade the NIH to provide the millions of dollars needed to push the field forward?
Robin Carhart-Harris believes the first drug that will receive FDA clearance is psilocybin, which he speculates could become legal in the next five to ten years. However, the field of psychedelic-assisted therapy needs more and larger clinical trials, preferably with the support of the NIH.
As Rucker and colleagues noted, the scientific literature bends toward the theme that the drugs are not necessarily therapeutic in and of themselves. It's the use of hallucinogens within a "psychologically supportive context" with a trained expert that's helpful. It's currently unknown how many users of recreational drugs are self-medicating for depression, anxiety, or other mental illnesses. But without the guidance of a knowledgeable psychotherapist, those who are self-medicating may not be helping themselves at all.
Will the positive buzz around psychedelics persuade the NIH to provide the millions of dollars needed to push the field forward? Given the changing climate in public opinion around these drugs and the need for breakthroughs in mental health therapies, it's possible that in the foreseeable future, this bold new therapy will become part of the mental health arsenal.
How 30 Years of Heart Surgeries Taught My Dad How to Live
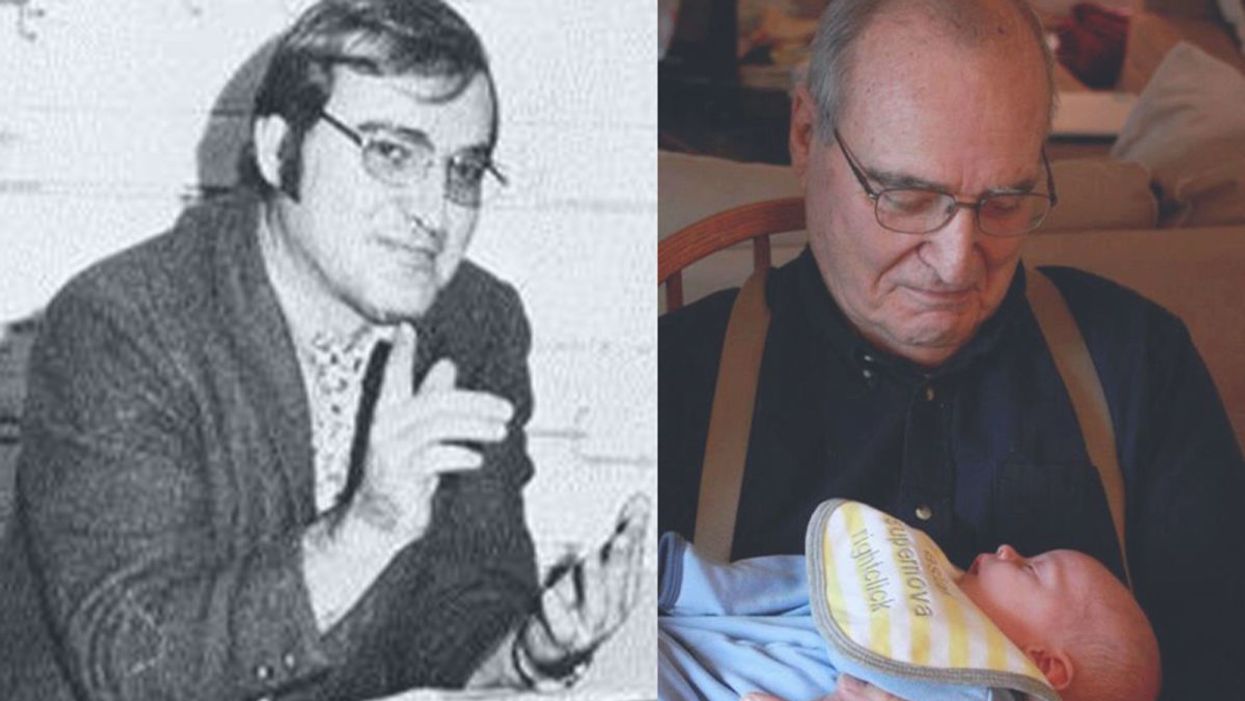
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.