Forget Farm-to-Table: Lab-to-Table Fresh Fish Is Making Waves
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

A conventionally sourced sea bass from a fishery.
Ever wonder why you've never heard of wild-caught organic fish? It's because there's no way to certify a food that has a mysterious history. Mike Selden, a 26-year-old biochemist with an animal lover's heart and an entrepreneur's mind, decided there must be better way to consume one of our planet's primary sources of animal protein. A way that would eliminate the need to kill billions of fish per year while also producing toxin-free, cheap, delicious fish meat for your dinner table. Enter Finless Foods, a young startup with a bold vision. Selden took time out of chauffeuring fish carcasses around San Francisco (no joke!) to share his journey with LeapsMag.
What is the biggest problem with the way fish is consumed today?
There are a lot of problems ranging from metals to animal welfare to human health. Technology is solving those problems at the same time. You've got extreme over fishing, which is collapsing ocean ecosystems and removing populations of fish that are traditionally used as food sources in developing nations.
In terms of animal welfare, fish are killed in massive numbers, billions a year. Even if people don't care too much about that, we want to give them another option.
In terms of health, which I think for most people is the most convincing argument, current fish have mercury and plastic in them. And if you're getting that fish from a farm, you will also have high levels of antibiotics and growth hormones if you're getting it from outside the U.S. What we're doing is producing fish that doesn't have any of those contaminants.
What gave you the idea to start a company around lab-grown fish?
I studied biochemistry and molecular biology at UMass Amherst, traditionally an agricultural school out in the woods of Massachusetts. I have always been an environmental activist and cared about animals. I thought, animal agriculture is so incredibly inefficient, what could be done to change it?
"The worst way you can possibly make a hamburger is with a cow."
Agriculture is a system of inputs and outputs, the inputs being feed and the outputs being meat – so why are we wasting all of this input on outputs we don't care about? Why are we creating these animals that waste all this energy through sitting around, moving around, having a heartbeat, blinking? All of this uses energy and that's valuable input.
The worst way you can possibly make a hamburger is with a cow. It's an awful transfer of energy: you have to feed it many times its own weight in food that could have fed other people or other things.
In February, I got funding from Indie Bio, a startup accelerator for synthetic biology, and moved out to San Francisco with my co-founder Brian Wyrwas. We started working in our lab in March. We're the newest company in the space.
Walk me through the process of creating edible fish in the lab. Do you have to catch a real live fish first and get their cells?
We have a deal with the Aquarium of the Bay, and whenever a fish dies, they call me, I get in a zip car, drive over, and bring the fish back to the lab, where Brian cultures it up into a cell culture. We do use real, high-quality fish stock. From there, we get the cells going in a bioreactor in a suspension culture, grow them into large quantities, and then bring them out to differentiate them into the cells people want to eat—the muscle and fat tissue. Then we formulate it and bring it to people's tables.
How long does the whole process take from the phone call about the fish dying to the food on the table?
There are two different processes: One is a research process, getting the initial cells and engineering them to be what we're looking for.
The other is a production process – we have a cell line ready and need to grow it out. That timing depends on how big of a facility we have. Since we're working with cell division: If you have 1 cell, in 24 hours, you'll have two cells. Let's say you have 1 ton of cells, in 24 hours you'll have two tons of cells.
"We want to give people the wholesome food they are used to in a healthier setting."
How are you looking to scale this process?
We're trying to find a middle ground between efficiency and local distribution. Organic farming is hilariously bad for the environment and horrifyingly inefficient, but on the other hand, industrial agriculture requires lots of transport, which is also bad for the environment. We're looking to create regionally distributed facilities which don't require a lot of transit, so people can have fresh fish even extremely far inland.
What kinds of fish are you "cooking"?
Our first product will be Bluefin tuna. It's a high-quality fish with high demand and it's also a conservation issue. We also currently have a culture going with Branzino, European sea bass, that we're really happy with.
There's a concept in science called a model organism – one that is extremely well studied and understood. Like the fruit fly, for example. For fish, it's the zebra fish, which is used for genetic research, but no one eats it. It's tiny, so we started by thinking: what fish do people eat that is also close evolutionarily to the zebra fish? We came up with carp, even though it's not too widely eaten.
But our process is very species agnostic. We've done work in trout, salmon, goldfish. Any fish with a dorsal fin works with our process. We tried a wolf eel but it didn't work. Eels are pretty far evolutionarily from fish, so we dropped that one.

From left to right, Ron Shigeta (IndieBio), Brian Wyrwas (Finless Foods), Amy Fleming (The Guardian), and Jihyun Kim (Finless Foods) tasting the first ever clean carp croquettes.
(Courtesy Mike Selden)
Why fish as opposed to, say, a cow?
Scientifically, there are a lot of advantages. Fish have a simpler structure than land animals. A fillet from a cow has complex marbling going on between the fat and muscle. When it's fish, like sashimi, it's in layers of muscle and fat. So it's simpler to build, plus fish are cold-blooded, so because they breathe underwater, our equipment needs less complexity. We don't need a CO2 line and we don't need to culture our cells at 37 degrees Celsius. We culture them at room temperature.
It's also easier to get to market since there's much higher value. Chicken in the last year was $3.84 per pound in America, whereas Bluefin tuna is between $100 and $1200 a pound. Because this is about dropping cost, we can get to market faster and give investors a better value proposition.
What's also cool is that something like Bluefin tuna is something many people haven't had the opportunity to eat. We can get these down in cost until there is price parity with any cheap conventional fish. We want to give people a choice between buying something like albacore tuna in a can –with mercury and plastic– or high-quality tuna without any contaminants for the same price.
Do you shape them like fish fillets to help the consumer overcome whatever discomfort they might feel about eating a bunch of lab-grown cells?
Yeah, people want to continue eating food they are eating, and that's fine. We want to give people a better option. We don't want to give them something weird and out there. We want to give them the wholesome food they are used to in a healthier setting that also solves some environmental issues.
How about the taste? Have you done any blind side-by-side tests with the real thing and your version?
Not blind taste tests. But we have been tasting it, and it is firmly fish. I even tried leaving it outside of the fridge – and man, that tasted like spoiled fish.
We want it to have the exact same properties as real fish. We don't want people to have to learn how to cook with it. We want them to just bring it into their homes and eat it exactly like they were doing before, but better.
What you're growing isn't the whole fish, right? It is not an actual organism?
Right, we're only growing muscle cells. It doesn't know where it is. There is no brain, nervous system, or pain receptors.
Are you the only people in this lab-grown food space working on fish?
We're the only ones doing fish so far. Other companies are doing chicken, duck, egg white, milk, gelatin, leather, and beef.
Are people generally weirded out by sci-fi lab food, or intrigued?
It's been very positive. When people sit down and talk to us, they realize it's not some crazed money grab or some weird Ted talk, it's real activists using real science trying to solve real problems. Sure, there will be some pushback from people who don't understand it, and that's fine.
When can I expect to see Finless Food at my local Whole Foods?
We plan on being in restaurants in two years, and grocery stores in four years.
What about people who aren't big fans of fish in the first place? Like those who don't eat sushi, because consuming something raw with an unknown history isn't very appetizing.
There are too many examples of food poisoning because fish are in a less clean environment than they should be, swimming around in their own fecal matter, and being doused in antibiotics so their diseases don't transmit. It's a bit of a mess. That's why as an industry, we're calling this clean meat. Fish is a healthy thing, or at least it should be, with Omega 3 and 6, and DHA. This is a way for people to continue getting those nutrients without any of the questions of where it came from. For people who are skeptical of fish, we invite you to dive in.

Brian Wyrwas, Co-Founder & CSO, and Mike Selden, Co-Founder & CEO
(Courtesy Mike Selden)
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.
Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
Last month, a paper published in Cell by Harvard biologist David Sinclair explored root cause of aging, as well as examining whether this process can be controlled. We talked with Dr. Sinclair about this new research.
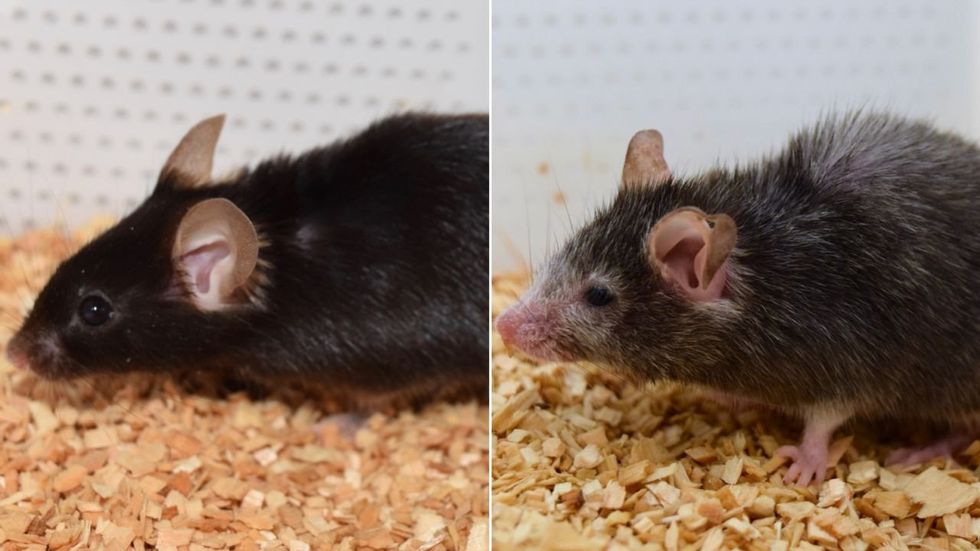
What causes aging? In a paper published last month, Dr. David Sinclair, Professor in the Department of Genetics at Harvard Medical School, reports that he and his co-authors have found the answer. Harnessing this knowledge, Dr. Sinclair was able to reverse this process, making mice younger, according to the study published in the journal Cell.
I talked with Dr. Sinclair about his new study for the latest episode of Making Sense of Science. Turning back the clock on mouse age through what’s called epigenetic reprogramming – and understanding why animals get older in the first place – are key steps toward finding therapies for healthier aging in humans. We also talked about questions that have been raised about the research.
Show links:
Dr. Sinclair's paper, published last month in Cell.
Recent pre-print paper - not yet peer reviewed - showing that mice treated with Yamanaka factors lived longer than the control group.
Dr. Sinclair's podcast.
Previous research on aging and DNA mutations.
Dr. Sinclair's book, Lifespan.

Harvard Medical School

