Forget Farm-to-Table: Lab-to-Table Fresh Fish Is Making Waves
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

A conventionally sourced sea bass from a fishery.
Ever wonder why you've never heard of wild-caught organic fish? It's because there's no way to certify a food that has a mysterious history. Mike Selden, a 26-year-old biochemist with an animal lover's heart and an entrepreneur's mind, decided there must be better way to consume one of our planet's primary sources of animal protein. A way that would eliminate the need to kill billions of fish per year while also producing toxin-free, cheap, delicious fish meat for your dinner table. Enter Finless Foods, a young startup with a bold vision. Selden took time out of chauffeuring fish carcasses around San Francisco (no joke!) to share his journey with LeapsMag.
What is the biggest problem with the way fish is consumed today?
There are a lot of problems ranging from metals to animal welfare to human health. Technology is solving those problems at the same time. You've got extreme over fishing, which is collapsing ocean ecosystems and removing populations of fish that are traditionally used as food sources in developing nations.
In terms of animal welfare, fish are killed in massive numbers, billions a year. Even if people don't care too much about that, we want to give them another option.
In terms of health, which I think for most people is the most convincing argument, current fish have mercury and plastic in them. And if you're getting that fish from a farm, you will also have high levels of antibiotics and growth hormones if you're getting it from outside the U.S. What we're doing is producing fish that doesn't have any of those contaminants.
What gave you the idea to start a company around lab-grown fish?
I studied biochemistry and molecular biology at UMass Amherst, traditionally an agricultural school out in the woods of Massachusetts. I have always been an environmental activist and cared about animals. I thought, animal agriculture is so incredibly inefficient, what could be done to change it?
"The worst way you can possibly make a hamburger is with a cow."
Agriculture is a system of inputs and outputs, the inputs being feed and the outputs being meat – so why are we wasting all of this input on outputs we don't care about? Why are we creating these animals that waste all this energy through sitting around, moving around, having a heartbeat, blinking? All of this uses energy and that's valuable input.
The worst way you can possibly make a hamburger is with a cow. It's an awful transfer of energy: you have to feed it many times its own weight in food that could have fed other people or other things.
In February, I got funding from Indie Bio, a startup accelerator for synthetic biology, and moved out to San Francisco with my co-founder Brian Wyrwas. We started working in our lab in March. We're the newest company in the space.
Walk me through the process of creating edible fish in the lab. Do you have to catch a real live fish first and get their cells?
We have a deal with the Aquarium of the Bay, and whenever a fish dies, they call me, I get in a zip car, drive over, and bring the fish back to the lab, where Brian cultures it up into a cell culture. We do use real, high-quality fish stock. From there, we get the cells going in a bioreactor in a suspension culture, grow them into large quantities, and then bring them out to differentiate them into the cells people want to eat—the muscle and fat tissue. Then we formulate it and bring it to people's tables.
How long does the whole process take from the phone call about the fish dying to the food on the table?
There are two different processes: One is a research process, getting the initial cells and engineering them to be what we're looking for.
The other is a production process – we have a cell line ready and need to grow it out. That timing depends on how big of a facility we have. Since we're working with cell division: If you have 1 cell, in 24 hours, you'll have two cells. Let's say you have 1 ton of cells, in 24 hours you'll have two tons of cells.
"We want to give people the wholesome food they are used to in a healthier setting."
How are you looking to scale this process?
We're trying to find a middle ground between efficiency and local distribution. Organic farming is hilariously bad for the environment and horrifyingly inefficient, but on the other hand, industrial agriculture requires lots of transport, which is also bad for the environment. We're looking to create regionally distributed facilities which don't require a lot of transit, so people can have fresh fish even extremely far inland.
What kinds of fish are you "cooking"?
Our first product will be Bluefin tuna. It's a high-quality fish with high demand and it's also a conservation issue. We also currently have a culture going with Branzino, European sea bass, that we're really happy with.
There's a concept in science called a model organism – one that is extremely well studied and understood. Like the fruit fly, for example. For fish, it's the zebra fish, which is used for genetic research, but no one eats it. It's tiny, so we started by thinking: what fish do people eat that is also close evolutionarily to the zebra fish? We came up with carp, even though it's not too widely eaten.
But our process is very species agnostic. We've done work in trout, salmon, goldfish. Any fish with a dorsal fin works with our process. We tried a wolf eel but it didn't work. Eels are pretty far evolutionarily from fish, so we dropped that one.

From left to right, Ron Shigeta (IndieBio), Brian Wyrwas (Finless Foods), Amy Fleming (The Guardian), and Jihyun Kim (Finless Foods) tasting the first ever clean carp croquettes.
(Courtesy Mike Selden)
Why fish as opposed to, say, a cow?
Scientifically, there are a lot of advantages. Fish have a simpler structure than land animals. A fillet from a cow has complex marbling going on between the fat and muscle. When it's fish, like sashimi, it's in layers of muscle and fat. So it's simpler to build, plus fish are cold-blooded, so because they breathe underwater, our equipment needs less complexity. We don't need a CO2 line and we don't need to culture our cells at 37 degrees Celsius. We culture them at room temperature.
It's also easier to get to market since there's much higher value. Chicken in the last year was $3.84 per pound in America, whereas Bluefin tuna is between $100 and $1200 a pound. Because this is about dropping cost, we can get to market faster and give investors a better value proposition.
What's also cool is that something like Bluefin tuna is something many people haven't had the opportunity to eat. We can get these down in cost until there is price parity with any cheap conventional fish. We want to give people a choice between buying something like albacore tuna in a can –with mercury and plastic– or high-quality tuna without any contaminants for the same price.
Do you shape them like fish fillets to help the consumer overcome whatever discomfort they might feel about eating a bunch of lab-grown cells?
Yeah, people want to continue eating food they are eating, and that's fine. We want to give people a better option. We don't want to give them something weird and out there. We want to give them the wholesome food they are used to in a healthier setting that also solves some environmental issues.
How about the taste? Have you done any blind side-by-side tests with the real thing and your version?
Not blind taste tests. But we have been tasting it, and it is firmly fish. I even tried leaving it outside of the fridge – and man, that tasted like spoiled fish.
We want it to have the exact same properties as real fish. We don't want people to have to learn how to cook with it. We want them to just bring it into their homes and eat it exactly like they were doing before, but better.
What you're growing isn't the whole fish, right? It is not an actual organism?
Right, we're only growing muscle cells. It doesn't know where it is. There is no brain, nervous system, or pain receptors.
Are you the only people in this lab-grown food space working on fish?
We're the only ones doing fish so far. Other companies are doing chicken, duck, egg white, milk, gelatin, leather, and beef.
Are people generally weirded out by sci-fi lab food, or intrigued?
It's been very positive. When people sit down and talk to us, they realize it's not some crazed money grab or some weird Ted talk, it's real activists using real science trying to solve real problems. Sure, there will be some pushback from people who don't understand it, and that's fine.
When can I expect to see Finless Food at my local Whole Foods?
We plan on being in restaurants in two years, and grocery stores in four years.
What about people who aren't big fans of fish in the first place? Like those who don't eat sushi, because consuming something raw with an unknown history isn't very appetizing.
There are too many examples of food poisoning because fish are in a less clean environment than they should be, swimming around in their own fecal matter, and being doused in antibiotics so their diseases don't transmit. It's a bit of a mess. That's why as an industry, we're calling this clean meat. Fish is a healthy thing, or at least it should be, with Omega 3 and 6, and DHA. This is a way for people to continue getting those nutrients without any of the questions of where it came from. For people who are skeptical of fish, we invite you to dive in.

Brian Wyrwas, Co-Founder & CSO, and Mike Selden, Co-Founder & CEO
(Courtesy Mike Selden)
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Working to Decipher the Puzzle of ‘Broken Heart Syndrome’
Elaine Kamil had just returned home after a few days of business meetings in 2013 when she started having chest pains. At first Kamil, then 66, wasn't worried—she had had some chest pain before and recently went to a cardiologist to do a stress test, which was normal.
"I can't be having a heart attack because I just got checked," she thought, attributing the discomfort to stress and high demands of her job. A pediatric nephrologist at Cedars-Sinai Hospital in Los Angeles, she takes care of critically ill children who are on dialysis or are kidney transplant patients. Supporting families through difficult times and answering calls at odd hours is part of her daily routine, and often leaves her exhausted.
She figured the pain would go away. But instead, it intensified that night. Kamil's husband drove her to the Cedars-Sinai hospital, where she was admitted to the coronary care unit. It turned out she wasn't having a heart attack after all. Instead, she was diagnosed with a much less common but nonetheless dangerous heart condition called takotsubo syndrome, or broken heart syndrome.
A heart attack happens when blood flow to the heart is obstructed—such as when an artery is blocked—causing heart muscle tissue to die. In takotsubo syndrome, the blood flow isn't blocked, but the heart doesn't pump it properly. The heart changes its shape and starts to resemble a Japanese fishing device called tako-tsubo, a clay pot with a wider body and narrower mouth, used to catch octopus.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks," explains Noel Bairey Merz, the cardiologist at Cedar Sinai who Kamil went to see after she was discharged.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks."
But even though the heart isn't permanently damaged, mortality rates due to takotsubo syndrome are comparable to those of a heart attack, Merz notes—about 4-5 percent of patients die from the attack, and 20 percent within the next five years. "It's as bad as a heart attack," Merz says—only it's much less known, even to doctors. The condition affects only about 1 percent of people, and there are around 15,000 new cases annually. It's diagnosed using a cardiac ventriculogram, an imaging test that allows doctors to see how the heart pumps blood.
Scientists don't fully understand what causes Takotsubo syndrome, but it usually occurs after extreme emotional or physical stress. Doctors think it's triggered by a so-called catecholamine storm, a phenomenon in which the body releases too much catecholamines—hormones involved in the fight-or-flight response. Evolutionarily, when early humans lived in savannas or forests and had to either fight off predators or flee from them, these hormones gave our ancestors the needed strength and stamina to take either action. Released by nerve endings and by the adrenal glands that sit on top of the kidneys, these hormones still flood our bodies in moments of stress, but an overabundance of them could sometimes be damaging.

Elaine Kamil
A study by scientists at Harvard Medical School linked increased risk of takotsubo to higher activity in the amygdala, a brain region responsible for emotions that's involved in responses to stress. The scientists believe that chronic stress makes people more susceptible to the syndrome. Notably, one small study suggested that the number of Takotsubo cases increased during the COVID-19 pandemic.
There are no specific drugs to treat takotsubo, so doctors rely on supportive therapies, which include medications typically used for high blood pressure and heart failure. In most cases, the heart returns to its normal shape within a few weeks. "It's a spontaneous recovery—the catecholamine storm is resolved, the injury trigger is removed and the heart heals itself because our bodies have an amazing healing capacity," Merz says. It also helps that tissues remain intact. 'The heart cells don't die, they just aren't functioning properly for some time."
That's the good news. The bad news is that takotsubo is likely to strike again—in 5-20 percent of patients the condition comes back, sometimes more severe than before.
That's exactly what happened to Kamil. After getting her diagnosis in 2013, she realized that she actually had a previous takotsubo episode. In 2010, she experienced similar symptoms after her son died. "The night after he died, I was having severe chest pain at night, but I was too overwhelmed with grief to do anything about it," she recalls. After a while, the pain subsided and didn't return until three years later.
For weeks after her second attack, she felt exhausted, listless and anxious. "You lose confidence in your body," she says. "You have these little twinges on your chest, or if you start having arrhythmia, and you wonder if this is another episode coming up. It's really unnerving because you don't know how to read these cues." And that's very typical, Merz says. Even when the heart muscle appears to recover, patients don't return to normal right away. They have shortens of breath, they can't exercise, and they stay anxious and worried for a while.
Women over the age of 50 are diagnosed with takotsubo more often than other demographics. However, it happens in men too, although it typically strikes after physical stress, such as a triathlon or an exhausting day of cycling. Young people can also get takotsubo. Older patients are hospitalized more often, but younger people tend to have more severe complications. It could be because an older person may go for a jog while younger one may run a marathon, which would take a stronger toll on the body of a person who's predisposed to the condition.
Notably, the emotional stressors don't always have to be negative—the heart muscle can get out of shape from good emotions, too. "There have been case reports of takotsubo at weddings," Merz says. Moreover, one out of three or four takotsubo patients experience no apparent stress, she adds. "So it could be that it's not so much the catecholamine storm itself, but the body's reaction to it—the physiological reaction deeply embedded into out physiology," she explains.
Merz and her team are working to understand what makes people predisposed to takotsubo. They think a person's genetics play a role, but they haven't yet pinpointed genes that seem to be responsible. Genes code for proteins, which affect how the body metabolizes various compounds, which, in turn, affect the body's response to stress. Pinning down the protein involved in takotsubo susceptibility would allow doctors to develop screening tests and identify those prone to severe repeating attacks. It will also help develop medications that can either prevent it or treat it better than just waiting for the body to heal itself.
Researchers at the Imperial College London found that elevated levels of certain types of microRNAs—molecules involved in protein production—increase the chances of developing takotsubo.
In one study, researchers tried treating takotsubo in mice with a drug called suberanilohydroxamic acid, or SAHA, typically used for cancer treatment. The drug improved cardiac health and reversed the broken heart in rodents. It remains to be seen if the drug would have a similar effect on humans. But identifying a drug that shows promise is progress, Merz says. "I'm glad that there's research in this area."
This article was originally published by Leaps.org on July 28, 2021.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Did Anton the AI find a new treatment for a deadly cancer?
Researchers used a supercomputer to learn about the subtle movement of a cancer-causing molecule, and then they found the precise drug that can recognize that motion.
Bile duct cancer is a rare and aggressive form of cancer that is often difficult to diagnose. Patients with advanced forms of the disease have an average life expectancy of less than two years.
Many patients who get cancer in their bile ducts – the tubes that carry digestive fluid from the liver to the small intestine – have mutations in the protein FGFR2, which leads cells to grow uncontrollably. One treatment option is chemotherapy, but it’s toxic to both cancer cells and healthy cells, failing to distinguish between the two. Increasingly, cancer researchers are focusing on biomarker directed therapy, or making drugs that target a particular molecule that causes the disease – FGFR2, in the case of bile duct cancer.
A problem is that in targeting FGFR2, these drugs inadvertently inhibit the FGFR1 protein, which looks almost identical. This causes elevated phosphate levels, which is a sign of kidney damage, so doses are often limited to prevent complications.
In recent years, though, a company called Relay has taken a unique approach to picking out FGFR2, using a powerful supercomputer to simulate how proteins move and change shape. The team, leveraging this AI capability, discovered that FGFR2 and FGFR1 move differently, which enabled them to create a more precise drug.
Preliminary studies have shown robust activity of this drug, called RLY-4008, in FGFR2 altered tumors, especially in bile duct cancer. The drug did not inhibit FGFR1 or cause significant side effects. “RLY-4008 is a prime example of a precision oncology therapeutic with its highly selective and potent targeting of FGFR2 genetic alterations and resistance mutations,” says Lipika Goyal, assistant professor of medicine at Harvard Medical School. She is a principal investigator of Relay’s phase 1-2 clinical trial.
Boosts from AI and a billionaire
Traditional drug design has been very much a case of trial and error, as scientists investigate many molecules to see which ones bind to the intended target and bind less to other targets.
“It’s being done almost blindly, without really being guided by structure, so it fails very often,” says Olivier Elemento, associate director of the Institute for Computational Biomedicine at Cornell. “The issue is that they are not sampling enough molecules to cover some of the chemical space that would be specific to the target of interest and not specific to others.”
Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
Some scientists have tried to use X-rays of crystallized proteins to look at the structure of proteins and design better drugs. But they have failed to account for an important factor: proteins are moving and constantly folding into different shapes.
David Shaw, a hedge fund billionaire, wanted to help improve drug discovery and understood that a key obstacle was that computer models of molecular dynamics were limited; they simulated motion for less than 10 millionths of a second.
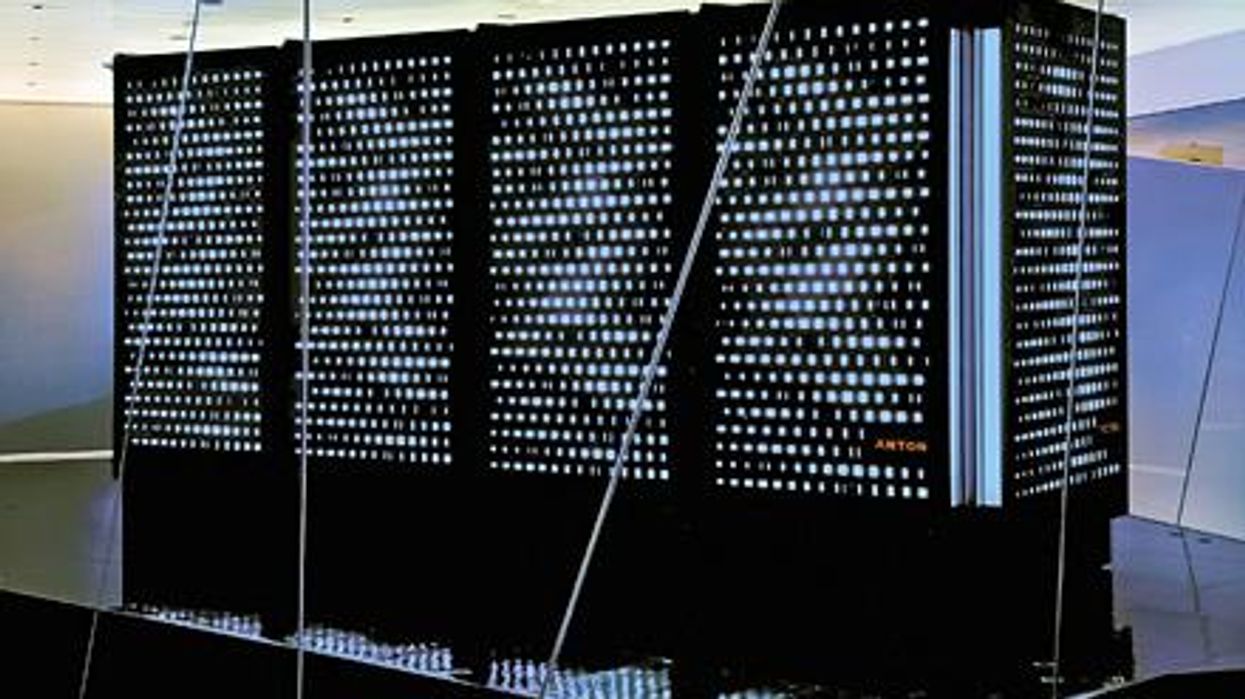
In 2001, Shaw set up his own research facility, D.E. Shaw Research, to create a supercomputer that would be specifically designed to simulate protein motion. Seven years later, he succeeded in firing up a supercomputer that can now conduct high speed simulations roughly 100 times faster than others. Called Anton, it has special computer chips to enable this speed, and its software is powered by AI to conduct many simulations.
After creating the supercomputer, Shaw teamed up with leading scientists who were interested in molecular motion, and they founded Relay Therapeutics.
Elemento believes that Relay’s approach is highly beneficial in designing a better drug for bile duct cancer. “Relay Therapeutics has a cutting-edge approach for molecular dynamics that I don’t believe any other companies have, at least not as advanced.” Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
How it works
Relay used both experimental and computational approaches to design RLY-4008. The team started out by taking X-rays of crystallized versions of both their intended target, FGFR2, and the almost identical FGFR1. This enabled them to get a 3D snapshot of each of their structures. They then fed the X-rays into the Anton supercomputer to simulate how the proteins were likely to move.
Anton’s simulations showed that the FGFR1 protein had a flap that moved more frequently than FGFR2. Based on this distinct motion, the team tried to design a compound that would recognize this flap shifting around and bind to FGFR2 while steering away from its more active lookalike.
For that, they went back Anton, using the supercomputer to simulate the behavior of thousands of potential molecules for over a year, looking at what made a particular molecule selective to the target versus another molecule that wasn’t. These insights led them to determine the best compounds to make and test in the lab and, ultimately, they found that RLY-4008 was the most effective.
Promising results so far
Relay began phase 1-2 trials in 2020 and will continue until 2024. Preliminary results showed that, in the 17 patients taking a 70 mg dose of RLY-4008, the drug worked to shrink tumors in 88 percent of patients. This was a significant increase compared to other FGFR inhibitors. For instance, Futibatinib, which recently got FDA approval, had a response rate of only 42 percent.
Across all dose levels, RLY-4008 shrank tumors by 63 percent in 38 patients. In more good news, the drug didn’t elevate their phosphate levels, which suggests that it could be taken without increasing patients’ risk for kidney disease.
“Objectively, this is pretty remarkable,” says Elemento. “In a small patient study, you have a molecule that is able to shrink tumors in such a high fraction of patients. It is unusual to see such good results in a phase 1-2 trial.”
A simulated future
The research team is continuing to use molecular dynamic simulations to develop other new drug, such as one that is being studied in patients with solid tumors and breast cancer.
As for their bile duct cancer drug, RLY-4008, Relay plans by 2024 to have tested it in around 440 patients. “The mature results of the phase 1-2 trial are highly anticipated,” says Goyal, the principal investigator of the trial.
Sameek Roychowdhury, an oncologist and associate professor of internal medicine at Ohio State University, highlights the need for caution. “This has early signs of benefit, but we will look forward to seeing longer term results for benefit and side effect profiles. We need to think a few more steps ahead - these treatments are like the ’Whack-a-Mole game’ where cancer finds a way to become resistant to each subsequent drug.”
“I think the issue is going to be how durable are the responses to the drug and what are the mechanisms of resistance,” says Raymond Wadlow, an oncologist at the Inova Medical Group who specializes in gastrointestinal and haematological cancer. “But the results look promising. It is a much more selective inhibitor of the FGFR protein and less toxic. It’s been an exciting development.”