Genetically Sequencing Healthy Babies Yielded Surprising Results

A newborn and mother in the hospital - first touch. (© martin81/Shutterstock)
Today in Melrose, Massachusetts, Cora Stetson is the picture of good health, a bubbly precocious 2-year-old. But Cora has two separate mutations in the gene that produces a critical enzyme called biotinidase and her body produces only 40 percent of the normal levels of that enzyme.
In the last few years, the dream of predicting and preventing diseases through genomics, starting in childhood, is finally within reach.
That's enough to pass conventional newborn (heelstick) screening, but may not be enough for normal brain development, putting baby Cora at risk for seizures and cognitive impairment. But thanks to an experimental study in which Cora's DNA was sequenced after birth, this condition was discovered and she is being treated with a safe and inexpensive vitamin supplement.
Stories like these are beginning to emerge from the BabySeq Project, the first clinical trial in the world to systematically sequence healthy newborn infants. This trial was led by my research group with funding from the National Institutes of Health. While still controversial, it is pointing the way to a future in which adults, or even newborns, can receive comprehensive genetic analysis in order to determine their risk of future disease and enable opportunities to prevent them.
Some believe that medicine is still not ready for genomic population screening, but others feel it is long overdue. After all, the sequencing of the Human Genome Project was completed in 2003, and with this milestone, it became feasible to sequence and interpret the genome of any human being. The costs have come down dramatically since then; an entire human genome can now be sequenced for about $800, although the costs of bioinformatic and medical interpretation can add another $200 to $2000 more, depending upon the number of genes interrogated and the sophistication of the interpretive effort.

Two-year-old Cora Stetson, whose DNA sequencing after birth identified a potentially dangerous genetic mutation in time for her to receive preventive treatment.
(Photo courtesy of Robert Green)
The ability to sequence the human genome yielded extraordinary benefits in scientific discovery, disease diagnosis, and targeted cancer treatment. But the ability of genomes to detect health risks in advance, to actually predict the medical future of an individual, has been mired in controversy and slow to manifest. In particular, the oft-cited vision that healthy infants could be genetically tested at birth in order to predict and prevent the diseases they would encounter, has proven to be far tougher to implement than anyone anticipated.
But in the last few years, the dream of predicting and preventing diseases through genomics, starting in childhood, is finally within reach. Why did it take so long? And what remains to be done?
Great Expectations
Part of the problem was the unrealistic expectations that had been building for years in advance of the genomic science itself. For example, the 1997 film Gattaca portrayed a near future in which the lifetime risk of disease was readily predicted the moment an infant is born. In the fanfare that accompanied the completion of the Human Genome Project, the notion of predicting and preventing future disease in an individual became a powerful meme that was used to inspire investment and public support for genomic research long before the tools were in place to make it happen.
Another part of the problem was the success of state-mandated newborn screening programs that began in the 1960's with biochemical tests of the "heel-stick" for babies with metabolic disorders. These programs have worked beautifully, costing only a few dollars per baby and saving thousands of infants from death and severe cognitive impairment. It seemed only logical that a new technology like genome sequencing would add power and promise to such programs. But instead of embracing the notion of newborn sequencing, newborn screening laboratories have thus far rejected the entire idea as too expensive, too ambiguous, and too threatening to the comfortable constituency that they had built within the public health framework.
"What can you find when you look as deeply as possible into the medical genomes of healthy individuals?"
Creating the Evidence Base for Preventive Genomics
Despite a number of obstacles, there are researchers who are exploring how to achieve the original vision of genomic testing as a tool for disease prediction and prevention. For example, in our NIH-funded MedSeq Project, we were the first to ask the question: "What can you find when you look as deeply as possible into the medical genomes of healthy individuals?"
Most people do not understand that genetic information comes in four separate categories: 1) dominant mutations putting the individual at risk for rare conditions like familial forms of heart disease or cancer, (2) recessive mutations putting the individual's children at risk for rare conditions like cystic fibrosis or PKU, (3) variants across the genome that can be tallied to construct polygenic risk scores for common conditions like heart disease or type 2 diabetes, and (4) variants that can influence drug metabolism or predict drug side effects such as the muscle pain that occasionally occurs with statin use.
The technological and analytical challenges of our study were formidable, because we decided to systematically interrogate over 5000 disease-associated genes and report results in all four categories of genetic information directly to the primary care physicians for each of our volunteers. We enrolled 200 adults and found that everyone who was sequenced had medically relevant polygenic and pharmacogenomic results, over 90 percent carried recessive mutations that could have been important to reproduction, and an extraordinary 14.5 percent carried dominant mutations for rare genetic conditions.
A few years later we launched the BabySeq Project. In this study, we restricted the number of genes to include only those with child/adolescent onset that could benefit medically from early warning, and even so, we found 9.4 percent carried dominant mutations for rare conditions.
At first, our interpretation around the high proportion of apparently healthy individuals with dominant mutations for rare genetic conditions was simple – that these conditions had lower "penetrance" than anticipated; in other words, only a small proportion of those who carried the dominant mutation would get the disease. If this interpretation were to hold, then genetic risk information might be far less useful than we had hoped.
Suddenly the information available in the genome of even an apparently healthy individual is looking more robust, and the prospect of preventive genomics is looking feasible.
But then we circled back with each adult or infant in order to examine and test them for any possible features of the rare disease in question. When we did this, we were surprised to see that in over a quarter of those carrying such mutations, there were already subtle signs of the disease in question that had not even been suspected! Now our interpretation was different. We now believe that genetic risk may be responsible for subclinical disease in a much higher proportion of people than has ever been suspected!
Meanwhile, colleagues of ours have been demonstrating that detailed analysis of polygenic risk scores can identify individuals at high risk for common conditions like heart disease. So adding up the medically relevant results in any given genome, we start to see that you can learn your risks for a rare monogenic condition, a common polygenic condition, a bad effect from a drug you might take in the future, or for having a child with a devastating recessive condition. Suddenly the information available in the genome of even an apparently healthy individual is looking more robust, and the prospect of preventive genomics is looking feasible.
Preventive Genomics Arrives in Clinical Medicine
There is still considerable evidence to gather before we can recommend genomic screening for the entire population. For example, it is important to make sure that families who learn about such risks do not suffer harms or waste resources from excessive medical attention. And many doctors don't yet have guidance on how to use such information with their patients. But our research is convincing many people that preventive genomics is coming and that it will save lives.
In fact, we recently launched a Preventive Genomics Clinic at Brigham and Women's Hospital where information-seeking adults can obtain predictive genomic testing with the highest quality interpretation and medical context, and be coached over time in light of their disease risks toward a healthier outcome. Insurance doesn't yet cover such testing, so patients must pay out of pocket for now, but they can choose from a menu of genetic screening tests, all of which are more comprehensive than consumer-facing products. Genetic counseling is available but optional. So far, this service is for adults only, but sequencing for children will surely follow soon.
As the costs of sequencing and other Omics technologies continue to decline, we will see both responsible and irresponsible marketing of genetic testing, and we will need to guard against unscientific claims. But at the same time, we must be far more imaginative and fast moving in mainstream medicine than we have been to date in order to claim the emerging benefits of preventive genomics where it is now clear that suffering can be averted, and lives can be saved. The future has arrived if we are bold enough to grasp it.
Funding and Disclosures:
Dr. Green's research is supported by the National Institutes of Health, the Department of Defense and through donations to The Franca Sozzani Fund for Preventive Genomics. Dr. Green receives compensation for advising the following companies: AIA, Applied Therapeutics, Helix, Ohana, OptraHealth, Prudential, Verily and Veritas; and is co-founder and advisor to Genome Medical, Inc, a technology and services company providing genetics expertise to patients, providers, employers and care systems.
Announcing "The Future of Science in America: The Election Issue"
This special magazine explores what's at stake for science & policy over the next four years.
As reviewed in The Washington Post, "Tomorrow's challenges in science and politics: Magazine offers in-depth takes on these U.S. issues":
"Is it time for a new way to help make adults more science-literate? What should the next president know about science? Could science help strengthen American democracy? "The Future of Science in America: The Election Issue" has answers. The free, online magazine is packed with interesting takes on how science can serve the common good. And just in time. This year has challenged leaders, researchers and the public with thorny scientific questions, from the coronavirus pandemic to widespread misinformation on scientific issues. The magazine is a collaboration of the Aspen Institute, a think tank that brings together a variety of public figures and private individuals to tackle thorny social issues, the digital science magazine Leapsmag and GOOD, a social impact company. It's packed with 15 in-depth articles about science with a view toward our campaign year."
The Future of Science in America: The Election Issue offers wide-ranging perspectives on challenges and opportunities for science as we elect our next national and local leaders. The fast-striking COVID-19 pandemic and the more slowly moving pandemic of climate change have brought into sharp focus how reliant we will be on science and public policy to work together to rescue us from crisis. Doing so will require cooperation between both political parties, as well as significant public trust in science as a beacon to light the path forward.
In spite of its unfortunate emergence as a flash point between two warring parties, we believe that science is the driving force for universal progress. No endeavor is more noble than the quest to rigorously understand our world and apply that knowledge to further human flourishing. This magazine aspires to promote roadmaps for science as a tool for health, a vehicle for progress, and a unifier of our nation.
This special issue is a collaboration among LeapsMag, the Aspen Institute Science & Society Program, and GOOD, with support from the Gordon and Betty Moore Foundation and the Rita Allen Foundation.
It is available as a free, beautifully designed digital magazine for both desktop and mobile.
TABLE OF CONTENTS:
- SCIENTISTS:
Award-Winning Scientists Offer Advice to the Next President of the United States - PUBLIC OPINION:
National Survey Reveals Americans' Most Important Scientific Priorities - GOVERNMENT:
The Nation's Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored? - TELEVISION:
To Make Science Engaging, We Need a Sesame Street for Adults - IMMIGRATION:
Immigrant Scientists—and America's Edge—Face a Moment of Truth This Election - RACIAL JUSTICE:
Democratize the White Coat by Honoring Black, Indigenous, and People of Color in Science - EDUCATION:
I'm a Black, Genderqueer Medical Student: Here's My Hard-Won Wisdom for Students and Educational Institutions - TECHNOLOGY:
"Deep Fake" Video Technology Is Advancing Faster Than Our Policies Can Keep Up - VOTERS:
Mind the (Vote) Gap: Can We Get More STEM Students to the Polls? - EXPERTS:
Who Qualifies as an "Expert" and How Can We Decide Who Is Trustworthy? - SOCIAL MEDIA:
Why Your Brain Falls for Misinformation—And How to Avoid It - YOUTH:
Youth Climate Activists Expand Their Focus and Collaborate to Get Out the Vote - SUPREME COURT:
Abortions Before Fetal Viability Are Legal: Might Science and a Change on the Supreme Court Undermine That? - NAVAJO NATION:
An Environmental Scientist and an Educator Highlight Navajo Efforts to Balance Tradition with Scientific Priorities - CIVIC SCIENCE:
Want to Strengthen American Democracy? The Science of Collaboration Can Help
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Envision a Universal Coronavirus Vaccine
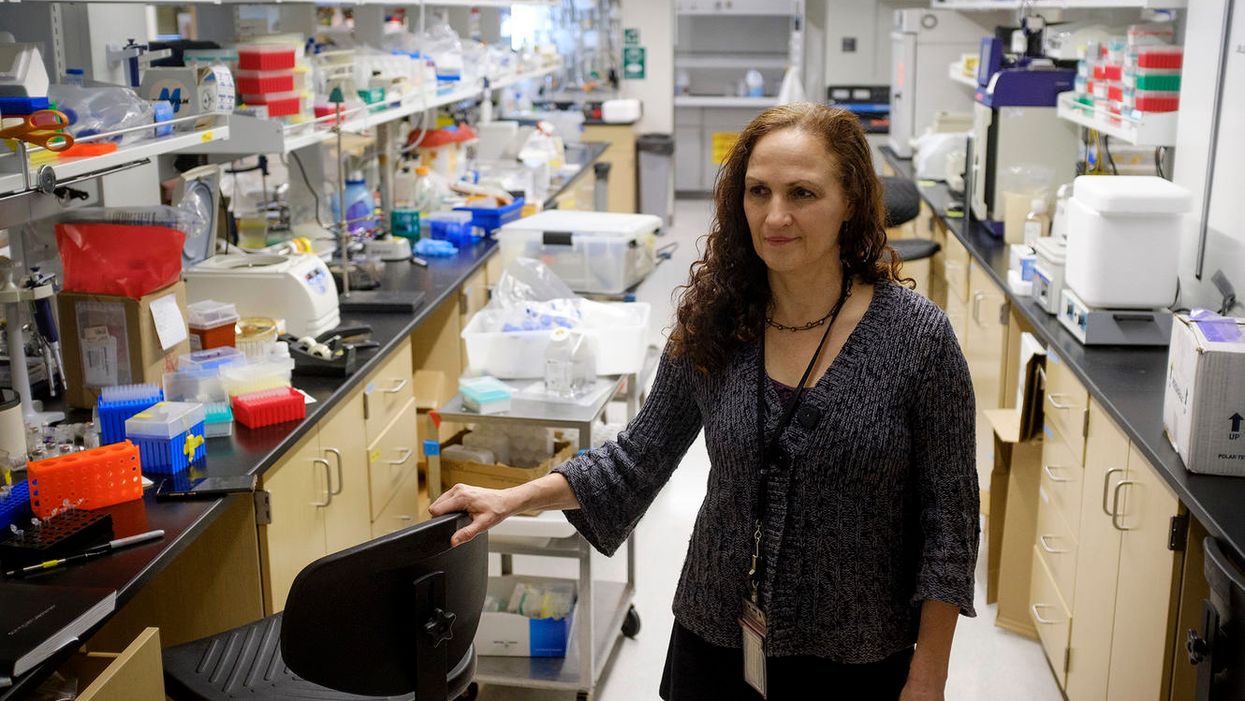
Dr. Deborah Fuller, a professor of microbiology at the Washington University School of Medicine, in her lab.
With several companies progressing through Phase III clinical trials, the much-awaited coronavirus vaccines may finally become reality within a few months.
But some scientists question whether these vaccines will produce a strong and long-lasting immunity, especially if they aren't efficient at mobilizing T-cells, the body's defense soldiers.
"When I look at those vaccines there are pitfalls in every one of them," says Deborah Fuller, professor of microbiology at the Washington University School of Medicine. "Some may induce only transient antibodies, some may not be very good at inducing T-cell responses, and others may not immunize the elderly very well."
Generally, vaccines work by introducing an antigen into the body—either a dead or attenuated pathogen that can't replicate, or parts of the pathogen or its proteins, which the body will recognize as foreign. The pathogens or its parts are usually discovered by cells that chew up the intruders and present them to the immune system fighters, B- and T-cells—like a trespasser's mug shot to the police. In response, B-cells make antibodies to neutralize the virus, and a specialized "crew" called memory B-cells will remember the antigen. Meanwhile, an army of various T-cells attacks the pathogens as well as the cells these pathogens already infected. Special helper T-cells help stimulate B-cells to secrete antibodies and activate cytotoxic T-cells that release chemicals called inflammatory cytokines that kill pathogens and cells they infected.
"Each of these components of the immune system are important and orchestrated to talk to each other," says professor Larry Corey, who studies vaccines and infectious disease at Fred Hutch, a non-profit scientific research organization. "They optimize the assault of the human immune system on the complexity of the viral, bacterial, fungal and parasitic infections that live on our planet, to which we get exposed."
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify.
The current frontrunner vaccines aim to train our body to generate a sufficient amount of antibodies to neutralize the virus by shutting off its spike proteins before it enters our cells and begins to replicate. But a truly robust vaccine should also engender a strong response from T-cells, Fuller believes.
"Everyone focuses on the antibodies which block the virus, but it's not always 100 percent effective," she explains. "For example, if there are not enough titers or the antibody starts to wane, and the virus does get into the cells, the cells will become infected. At that point, the body needs to mount a robust T-cytotoxic response. The T-cells should find and recognize cells infected with the virus and eliminate these cells, and the virus with them."
Some of the frontrunner vaccine makers including Moderna, AstraZeneca and CanSino reported that they observed T-cell responses in their trials. Another company, BioNTech, based in Germany, also reported that their vaccine produced T-cell responses.
Fuller and her team are working on their own version of a coronavirus vaccine. In their recent study, the team managed to trigger a strong antibody and T-cell response in mice and primates. Moreover, the aging animals also produced a robust response, which would be important for the human elderly population.
But Fuller's team wants to engage T-cells further. She wants to try training T-cells to recognize not only SARV-CoV-2, but a range of different coronaviruses. Wild hosts, such as bats, carry many different types of coronaviruses, which may spill over onto humans, just like SARS, MERS and SARV-CoV-2 have. There are also four coronaviruses already endemic to humans. Cryptically named 229E, NL63, OC43, and HKU1, they were identified in the 1960s. And while they cause common colds and aren't considered particularly dangerous, the next coronavirus that jumps species may prove deadlier than the previous ones.
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify. "T-cells can recognize these shared sequences across multiple different types of coronaviruses," she explains, "so we have this vision for a universal coronavirus vaccine."
Paul Offit at Children's Hospitals in Philadelphia, who specializes in infectious diseases and vaccines, thinks it's a far shot at the moment. "I don't see that as something that is likely to happen, certainly not very soon," he says, adding that a universal flu vaccine has been tried for decades but is not available yet. We still don't know how the current frontrunner vaccines will perform. And until we know how efficient they are, wearing masks and keeping social distance are still important, he notes.
Corey says that while the universal coronavirus vaccine is not impossible, it is certainly not an easy feat. "It is a reasonably scientific hypothesis," he says, but one big challenge is that there are still many unknown coronaviruses so anticipating their structural elements is difficult. The structure of new viruses, particularly the recombinant ones that leap from wild hosts and carry bits and pieces of animal and human genetic material, can be hard to predict. "So whether you can make a vaccine that has universal T-cells to every coronavirus is also difficult to predict," Corey says. But, he adds, "I'm not being negative. I'm just saying that it's a formidable task."
Fuller is certainly up to the task and thinks it's worth the effort. "T-cells can cross-recognize different viruses within the same family," she says, so increasing their abilities to home in on a broader range of coronaviruses would help prevent future pandemics. "If that works, you're just going to take one [vaccine] and you'll have lifetime immunity," she says. "Not just against this coronavirus, but any future pandemic by a coronavirus."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.